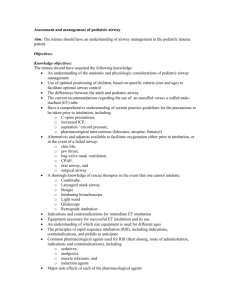
Mel`s Airway Management Outline
advertisement

Airway Management Course Objectives Define Rapid Sequence Intubation Identify patients that may benefit from RSI General overview of RSI procedure Discuss methods for identifying patients with possible difficult airways. Discuss pharmacology associated with RSI Discuss the use of adjunct airways in failed intubation attempts Define Rapid Sequence Intubation Identify patients that may benefit from RSI General overview of RSI procedure Discuss methods for identifying patients with possible difficult airways. Discuss pharmacology associated with RSI Discuss the use of adjunct airways in failed intubation attempts Airway Management Airway management is the single most important skill of emergency care providers Airway takes precedence over all other clinical considerations Without a secure airway and adequate oxygenation and ventilation, all other resuscitative measures will fail. Airway Anatomy – see book Basic Airway Assessment Assess airway Is it open/patent? (look, listen, feel) Assess breathing What is the rate? Is it adequate? Do I need to breath for them, or assist their breathing? CAN YOU OXYGENATE YOUR PATIENT Intervene Open the airway (jaw thrust or head tilt) Ventilate patient if needed Signs of Respiratory Distress Rapid Too slow Irregular Cyanosis Highly anxious Bolt upright posture Tripod posture Nasal flaring (MOST OFTEN SEEN IN CHILDREN) Don’t forget your BLS airway adjuncts: OPA, NPA Maintain C-spine precautions on ANY trauma patient or suspected cervical injury. Opening the Airway The #1 cause of an obstructed airway in a conscious patient is food The #1 cause of an obstructed airway in an unconscious patient is the tongue If you suspect trauma, stabilize the head and use the jaw-thrust maneuver If you do not suspect trauma, use the head-tilt/chin-lift maneuver Head Tilt/Chin Lift The head should only be tilted back slightly Too much tilt backwards (hyperextension) can cause the trachea to collapse Too much tilt forwards (hyperflexion) will also occlude the airway Placing a small towel beneath the patient’s shoulders should align their head (airway) properly Jaw Thrust Used when trauma is suspected This maneuver is not easy to maintain. Be aware you may get tired and need to switch rescuers You are basically giving the patient an under bite Oropharyngeal Airway Used to maintain the airway of an unresponsive patient who has no gag reflex (USED ON UNCONSCIOUS PATIENT) How to Insert an OPA Open the patient’s mouth Size the OPA (corner of the mouth to the tip of the earlobe, or angle of the jaw) Insert OPA with the tip pointed to the roof of the patient’s mouth Advance until you meet resistance from the hard palate Rotate the OPA 180 degrees Flange should rest on your patient’s teeth Reassess the patient’s airway Nasopharyngeal Airway Less likely to stimulate vomiting Can be used in patients that still have an intact gag reflex and are semiconscious This adjunct can be painful during insertion Sizing: measure from the tip of the earlobe to the tip of the nose; it should also fit inside the diameter of the nose How to Insert a NPA Size the NPA Lubricate the NPA with a water-soluble lubricant (Xylocaine jelly, K-Y jelly) Place the beveled edge against the septum If you meet resistance…..STOP Reassess the airway The Decision to Intubate Is there a failure of airway maintenance or is integrity compromised? Is there a failure of ventilation and oxygenation? What is the anticipated clinical course? Rapid Sequence Intubation The purpose of RSI is facilitate endotracheal intubation with the least likelihood of aspiration. Contraindications Absolute - Lack of training by personnel Predicted difficult intubation is NOT a contraindication Establish a back-up plan Indications for RSI Can the patient protect their airway? Ask the patient if he/she swallow strongly….this is due to the ability of the epiglottis opening Can you oxygenate the patient? What is the expected clinical course? The Technique The 7 P’s to successful intubation Preparation – this is where the nurse comes into play (get all the supplies ready…always have a backup plan…if the patient cannot be intubated) Preoxygenate Pretreatment Paralysis with induction Protection and positioning Placement and proof Postintubation management 1. Preparation Full patient assessment including assessing for possible difficult airway. All fall back plans established. Cardiac monitoring, BP monitoring, SaO2. Gathering of equipment.** 2. Preoxygenation Preoxygenation is essential to RSI (use a nonrebreather mask) Preoxygenation is required to establish the oxygen reservoir 100% O2 for approximately 5 mins Provide Oxygen Nasal Cannula Face Mask 24% - 44% O2 with reservoir 60% - 100% Bag valve mask Important skill for healthcare providers Dependent on adequate seal and patent airway Can deliver high concentrations of oxygen Two types - self inflating – big blue bubble bag (gives 100% O2) - flow inflating Oxyhemoglobin Dissociation Curve 3. Pretreatment The administration of drugs to mitigate adverse effects associated with intubation. Should be given approximately 3 mins prior to intubation. LOAD - Lidocaine 1.5 mg/kg ** Opiate (fentanyl)** Atropine 0.02 mg/kg (pediatric) Defasciculation 0.01 mg/kg 4. Paralysis with induction Administration of induction agent (Etomidate or Versed) to produce rapid LOC followed by a Neuromuscular blocking agent. Administration should be RAPID IV push. 5. Protection and Positioning LOC should be present after 30 sec. Sellick’s maneuver should be applied. Pressure on the cricoid cartilage to prevent passive regurgitation of gastric contents. – very very important for a Nurse to know and do Remember BURP (back, up, right, pressure) – helps to see the opening of the vocal cords How should you maintain cricoid pressure? Do not let up on pressure until tube is in place, cuff is inflated 6. Placement and Proof Placement and Proof Approximately 45 seconds after the administration of neuromuscular blocking agent, the tube should be placed. Techniques for confirmation Feeling of going through cords Bilateral breath sounds End tidal CO2 (gold standard) -- Capnography Misting Pulse oximetry Breath Sounds Colormetric end tidal CO2 Aspiration techniques 7. Postintubation Management Administration of appropriate sedating agent should be given 1 min following OETT placement. Bradycardia post intubation should be assumed attributed to esophageal intubation until proven otherwise. Hypertension usually indicates inadequate sedation. A (LONG TERM) sedative agent and neuromuscular blocking agent should be administered according to protocol. Tips and Timing Ideal time required for each RSI step. Preoxygenation should be 5 mins or 8 vital capacity breaths. Pretreatment drugs should be given 3 mins before the administration of the sedative and neuromuscular blocking agent. Common Mistakes Making the difficult airway more difficult 1. Rushing 2. Poor equipment preparation (including lack of suction) IN REVIEW Preparation Preoxygenate Pretreatment Paralysis with induction Protection and positioning Placement and proof Postintubation management What if I lose SaO2? Remember…….. DOPE!!!!! Dislodged Obstructed Pneumothorax Equipment failure Adjunct Airways CombiTube Laryngeal Mask Airway (LMA) CombiTube Indications Failed airway which is not due to foreign body obstruction. When skill level of personnel does not permit intubation. When endotracheal intubation is felt to be impossible. Contraindications Pt is responsive Intact gag reflex Known esophageal disease Ingestion of caustic substances Upper airway obstruction due to foreign body. Laryngeal Mask Airway (LMA) Designed to cover the supraglottic area. Used as a temporizing agent in a failed airway situation. Patient must be sedated. LMA Disadvantages Not a definitive airway device Does not protect against aspiration. Different sizes needed. Pharmacology Premedications - Fentanyl Sedatives and Induction Agents - Benzodiazepines (Versed, Valium, Ativan) - Etomidate Muscle Relaxants (paralytics) - depolarizing neuromuscular blocking - nondepolarizing neuromuscular blocking Pretreatment Lidocaine Opioid Atropine Defasciculation Pretreatment Lidocaine -1.5mg/kg 3 mins prior to intubation - increases depth of anesthesia - decreases cerebral oxygen demand - decreases cerebral blood flow - suppresses cough reflex (important because with patient with head injury, this will decrease ICP) Premedications Fentanyl (Sublimaze) 100 times more potent than Morphine Classification – Opioid analgesic Binds with the opiate receptors in the CNS No direct effect on ICP Suppress respiratory effort (hypercarbia) Potential for hypotension Dose 1-3 mcg/kg - Sedatives and Induction Agents midazolam (Versed) etomidate (Amidate) propofol (Diprivan) Etomidate (Amidate) A carboxylated imidazole-containing hypnotic anesthetic (induction agent) Dose: 0.2-0.4 mg/kg IV only Onset: 15-45 seconds Duration: 3-12 minutes Contraindications: none (except in pedi) Effects pain on injection, venoirritation involuntary myoclonic movements due to brain stem stimulation anticonvulsant properties decreased CBF, ICP adrenal suppression (5-8 hrs duration) no histamine release minimal cardiorespiratory depression no blunting of sympathetic response unless combined with opioid Midazolam (Versed) Benzodiazepine Very important to monitor BP while using this medication IV, PO, IM, PR, intranasal Onset: 2-3 minutes, duration of IV dose ~ 2 hours Uses: Anxiolytic Induction of anesthesia Sedation Anticonvulsant Amnestic Dosages: Sedation: IV bolus: 1-2 mg IV Q 2 min Infusion: 1-7 mg/hr Anticonvulsant: 1-2 mg IV Q 2 min Induction of anesthesia: 0.3 mg/kg IVP Reduce dosage in elderly, pt’s with hepatic failure Contraindications: Allergy Propofol (Diprivan) Alkylphenol derivative - hypnotic agent Indicated for induction of anesthesia Good procedural drug Significant hypotension Some myocardial depression Dose range 10-100 mcg/kg/min Muscle Relaxants (Paralytic) Muscle Relaxants (2 classifications) - depolarizing neuromuscular blocking - non-depolarizing neuromuscular blocking Muscle Relaxants does not have a analgesic affect, YOU MUST USE A SEDATIVE AND PAIN CONTROL Succinylcholine (clears in 3-5mins) Noncompetitive Depolarizing NMBA Binds with Nicotinic acetylcholine receptors resulting in depolarization of the muscle Benefits -Rapid onset - Short duration - Low histamine release Pharmacokinetics of Succs Succinylcholine binds with and depolarizes nicotinic acetylcholine receptors to cause paralysis. Side Effects of SCh Fasciculations – involuntary muscle twitching caused by the stimulation of acetylcholine receptors. Hyperkalemia**** Refractory bradycardia Hypotension (histamine release) Prolonged neuromuscular blockage Malignant hyperthermia**** Trismus Contraindications to SCh Anyone with ongoing or suspected hyperkalemia Progressive ongoing neuromuscular disease Renal considerations Malignant hyperthermia Dosing SCh Dose – 1.5mg/kg to 2mg/kg IV Onset - 45-60 sec Return of spontaneous resp. – 3-5 mins NEVER REDOSE!! Competitive, non depolarizing NMBA Compete and block the action of acetylcholine at the neuromuscular junction. Does not cause fasciculations. Major drawback is the longer onset of action and the longer duration of action. May be reversed by acetylcholinesterase inhibitors such as neostigmine. Mivacron, Vecuronium, Rocuronium, Pavulon Vecuronium Competitive non-depolarizing NMBA Onset - 2-3 minutes Dose – 0.1 mg/kg Duration – 30-45 minutes Higher dose of 0.3 mg/kg may be used to reduce onset to 90 sec. Vecuronium considerations Children may require higher doses (per medical control). Those under 1 year of age may have pronounced effects. Those patients with existing neuromuscular diseases such as Myasthenia gravis may have profound effects. Malignant Hyperthermia