Case 1 Closed reduction and K wiring pinning.
advertisement
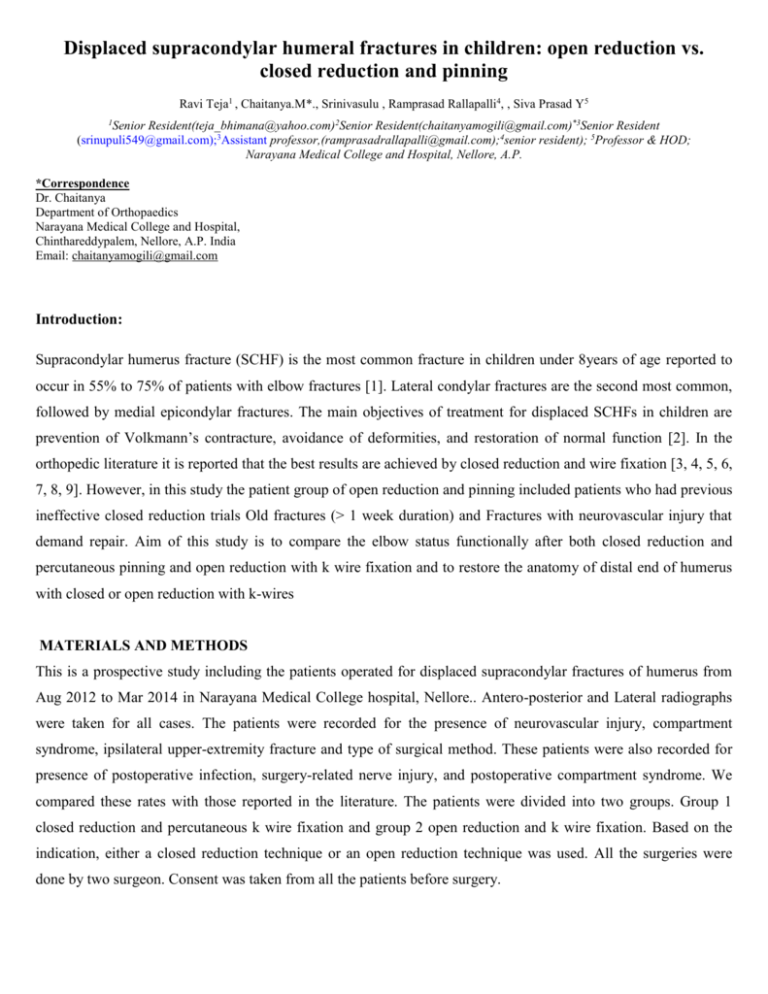
Displaced supracondylar humeral fractures in children: open reduction vs. closed reduction and pinning Ravi Teja1 , Chaitanya.M*., Srinivasulu , Ramprasad Rallapalli4, , Siva Prasad Y5 1 Senior Resident(teja_bhimana@yahoo.com)2Senior Resident(chaitanyamogili@gmail.com)*3Senior Resident (srinupuli549@gmail.com);3Assistant professor,(ramprasadrallapalli@gmail.com);4senior resident); 5Professor & HOD; Narayana Medical College and Hospital, Nellore, A.P. *Correspondence Dr. Chaitanya Department of Orthopaedics Narayana Medical College and Hospital, Chinthareddypalem, Nellore, A.P. India Email: chaitanyamogili@gmail.com Introduction: Supracondylar humerus fracture (SCHF) is the most common fracture in children under 8years of age reported to occur in 55% to 75% of patients with elbow fractures [1]. Lateral condylar fractures are the second most common, followed by medial epicondylar fractures. The main objectives of treatment for displaced SCHFs in children are prevention of Volkmann’s contracture, avoidance of deformities, and restoration of normal function [2]. In the orthopedic literature it is reported that the best results are achieved by closed reduction and wire fixation [3, 4, 5, 6, 7, 8, 9]. However, in this study the patient group of open reduction and pinning included patients who had previous ineffective closed reduction trials Old fractures (> 1 week duration) and Fractures with neurovascular injury that demand repair. Aim of this study is to compare the elbow status functionally after both closed reduction and percutaneous pinning and open reduction with k wire fixation and to restore the anatomy of distal end of humerus with closed or open reduction with k-wires MATERIALS AND METHODS This is a prospective study including the patients operated for displaced supracondylar fractures of humerus from Aug 2012 to Mar 2014 in Narayana Medical College hospital, Nellore.. Antero-posterior and Lateral radiographs were taken for all cases. The patients were recorded for the presence of neurovascular injury, compartment syndrome, ipsilateral upper-extremity fracture and type of surgical method. These patients were also recorded for presence of postoperative infection, surgery-related nerve injury, and postoperative compartment syndrome. We compared these rates with those reported in the literature. The patients were divided into two groups. Group 1 closed reduction and percutaneous k wire fixation and group 2 open reduction and k wire fixation. Based on the indication, either a closed reduction technique or an open reduction technique was used. All the surgeries were done by two surgeon. Consent was taken from all the patients before surgery. INCLUSION CRITERIA: Children with displaced supracondylar fracture of humerus with an open physis, (Grade III Gartland’s Type) coming to Narayana Medical College during study period willing to participate in study after giving informed consent. EXCLUSION CRITERIA: 1. Patients with displaced fracture but with closed physis. 2. Un displaced & minimally displaced fractures (Gartland type I and II). 3.Compound fractures INDICATIONS: FOR CLOSED REDUCTION: 1. Fresh closed displaced fractures of less than 1 week duration & with no neurovascular injury that demand repair. FOR OPEN REDUCTION: 1. Failed closed reduction 2. Old fractures (> 1 week duration) 3. Fractures with neurovascular injury that demand repair In group 1 closed reduction was done by Milking maneuver and either lateral pinning or crossed pinning was used according to surgeon preference. In group 2 The intubated patient was placed prone with a sandbag under- neath the abducted arm. The surgery was performed through a posteromedial incision posterior to the medial epicondyle. After isolating the ulnar nerve the distal humerus was exposed between the brachialis and triceps muscles as in the medial approach. The average period between injury and operation was 15 h (range 11–48) in the open group and 17 h (10–72) in the closed group. In both groups two smooth Kirschner wires were used. After the operation three to 4 weeks of dorsal long arm splint at 90° was used for each group. By the end of fourth week the fracture was examined by radiology, and wires were removed. In the case of improper radio- logical callus formation follow-up radiography was performed in the 6th week. Active elbow range of motion rehabilitation program was encouraged in the 4th week under the supervision of a physical therapist. The patients were followed radiologically and clinically and were called for a final assessment at 18 months in both groups after the initial surgery. Patients were evaluated for the radiological humeral-ulnar angle as the carrying angle and clinically for flexion and extension degrees, and the findings were compared with those in the contralateral normal elbow. Final results were graded by the criteria of Flynn et al. [4] Statistical analysis used Student’ s t Yates’ correction for qualitative vari- ables. RESULTS: This is a prospective study including the patients operated for displaced supracondylar fractures of humerus from Aug 2010 to Mar 2014. This study includes 20 patients with 10 patients in closed reduction and percutaneous k wire fixation(group 1) and open reduction and k wire fixation(group 2). All cases selected had open physis and between 0-12yrs of age with mean age of 7.5 years in group 1 and 8.9 years in group 2. In group 1 50% were males and 50 % were female whereas in group 2 all the patients are males. In the present series all cases of both groups had a history of trauma either direct or indirect and their distribution by various mechanisms is shown in (table 1) Most of the fractures were sustained when the patient had fallen down on out stretched hand while playing or slip and fall. In both groups left side is more involve then right. Associated injuries in group 1 are 1 case (Green stick #both bones forearm)(1%) ,1 case(closed # distal radius) and in those group 2, 3 cases(30%) of those operated by open reduction are associated with vascular injury, 2 cases: Brachial artery impingement, 1 case: Brachial artery injury and Overall 4 cases(20%) had associated neurological injury . Type of construct used in both groups is show in table 2 and 3 Indication of open reduction in our series in table 4. Complications occurred are 1case of ulnar nerve palsy in case treated by closed reduction and cross construct. 1 case of cubitus varus and 2 cases of pin tract infection. Grading of results(as per flynns) for both groups is shown in table 5 and 6 DISCUSSION Supracondylar fractures of humerus are common fractures occurring in childhood. Prompt and effective treatment should be given to these injuries to achieve best possible results. Adequate history and clinical evaluation including neurovascular status of the limb, radiological diagnosis and classifying the fracture are imperative before giving any mode of treatment. Anatomical reduction and stable fixation followed by proper physiotherapy are mandatory to get good results Our series consists of 20 cases of displaced (Gartland’s Type III) supracondylar fractures of humerus in children treated by either closed reduction and percutaneous K wire fixation or open reduction and K wire fixation under general anesthesia and C-arm control. Of all the supracondylar fractures, only those patients with open physis & who belonged to Gartland's Type Ill are included in our study. Out of 20 cases, all the cases were of extension type with either postero-medial or postero-lateral displacement of distal fragment. KAYE E.WILKINS; JAMES H.BEATY et al[10] compiled data from 7212 fractures occurring in 6l major series. They observed male dominance with 62.8%; non-dominant limb involved in 60.5% of cases. Average age was 6.7 years.1%of cases were flexion type. In 1% of the cases, ipsilateral fractures of forearm were found; 1% were open fractures. Neurological injury found in 7.7% of cases, out of these radial nerve was involved in 41.2%; median nerve was involved in 36% of cases, ulnar nerve in 22.8%of cases. According to CHENG AND LAM et al.[11] median age at presentation was 6yrs (6.6 years in boys, and 5 years in girls, with the non-dominant humerus 1.5times more commonly injured and they found flexion type of fractures in l% of cases. In our series, average age was found to be 7.5 in cases operated by closed reduction &8.9 yrs in cases operated by open reduction. Overall the average age was found to be 8.2yrs ,with 8.46yrs in boys and 7.4 yrs in girls. When compared to KAYE E.WILKINS study average age of incidence in our study is 1.5 yrs more towards elder side. There is male preponderance with 75%(overall),which is comparable to WILKINS study(62.8%).In our series supracondylar fractures are common in non dominant side with an incidence of 65% which is comparable to WILKINS study and observation of CHENG AND LAM et al [11]It was found that the injury was caused by low energy trauma. Most of them were sustained due to fall on outstretched hand due to slip and fall or while playing at home or school, which accounts for 70% of cases.15% of cases were injured in R.T.A and 15%of cases sustained injury due to fall from height. Out of the 20 cases,3 cases had an association with vascular injury . 1% of cases , one each in those treated by closed reduction and open reduction were associated with fractures of ipsilateral forearm .Green stick # of distal end of both bones associated with closed supracondylar # was managed conservatively and the distal radius # associated with supra condylar fracture was managed with percutaneous K wire fixation. CULP RW; OSTERMAN et al [12]observed 12.8% neural injuries in their retrospective review of displace extension type of supracondylar fractures in 101 children.70%of them spontaneously resolved at a mean of 2.5 months .They concluded that observation and supportive therapy is the preferred initial approach; if there is no clinical or electromyographic evidence of return of neural function at 5 months after injury ,exploration and neurolysis is indicated LYONS ST ;QUINN et al [13]found 13.3%of neural compromise ,combined nerve and vascular compromise in 2.9%of patients. Median nerve injury accounted for 58.9% of nerve injuries, followed by radial (26.4%) and ulnar (14.7%) lesions,80%of them are anterior interosseous nerve compromise. In our series the overall incidence of neural involvement was 20%. Out of these median nerve was involved in 2 cases(10%) and radial nerve was involved in 2 cases(10%).Spontaneous recovery occurred in all within a mean time of 4 months without any surgical intervention. Vascular compromise was found in 3 case. The overall incidence was 15%.Exploration was done in all cases .Compression of the artery was released in two cases. Intimal injury and thrombus was found in one case which was treated by thrombectomy and end to end anastomosis. Majority of the cases were admitted on the day of injury. All cases were taken up under general anesthesia as early as possible. Out of 10 cases operated by open reduction ,40% had irreducible # by closed method,20% had # with delayed presentation(>1 week),20% had closed vascular injury,10% had vascular injury and 10% had nerve palsy. REITMAN RD, WATERs P et al [14] managed 65 type III fractures with open reduction and pinning. Of the 65 patients who were managed with open reduction, 46(71%)were due to irreducibility of fracture , 16(24%) had associated vascular compromise, 8(12%)were open ,and one was associated with post reduction nerve palsy .According to the criteria of Flynn et al 18(55%)elbows were rated excellent,8(24%) were rated good three(9%)were rated fair and 4(12%) were rated poor after an average of 5.8 months post injury. SKAGGS DL HALE J1. et al [15] concluded that there was no difference with regard to maintenance or fracture reduction between the crossed pins configuration and the two lateral pin configuration .They found that use of a medial pin was associated with ulnar nerve injury in 4% of the cases. REYNOLDS RA.MIRZAYAN R.et al [16] have shown that there is a biomechanical advantage of crossed pin construct as opposed to two lateral pin construct .However they have found 4.5% incidence of ulnar nerve injury with medial pin placement. We have fixed the reduced fracture with a crossed pin technique in 25% of cases and a lateral two pin construct in 75% of cases. Our criteria for a medial pin was to place it if the fixation is found to be unstable with two lateral pins alone. No neuro vascular deficit occurred in cases of open reduction and K wire fixation. Ulnar neuropraxia was identified in 1 case of closed reduction and crossed pin construct and it recovered within 4 weeks. Immediately after identifying the palsy the K wire was removed. In order to protect the ulnar nerve during medial pin placement, push the nerve anteriorly during pinning or use a small incision over the medial epicondyle in the presence of gross swelling. The results of the treatment were assessed using the criteria of FLYNN et al [17] to compare the motion and carrying angle of the injured and the un injured elbow. The function is graded in 5 degree intervals of loss of flexion or extension, and the cosmetic appearance of elbow is graded in 5 degree intervals of change in the carrying angle, with any varus angulation resulting in a poor grade. YAOKREH J.B.,GICQUEL .P et al [18]observed that In paediatric extensiontype supracondylar fractures of elbow,Out of 58 children, Outcomes were satisfactory in 30 (90.9%) patients treated with percutaneous pinning and in 23 (92%) patients treated with open reduction and cross-wiring. Iatrogenic nerve injury in two (3.4%) patients. Cubitus varus occurred in two (6.06%)patients after closed treatment and in one (4%) patient after open treatment. In our study out of 10 cases managed by closed reduction excellent to good results are seen in 90% of cases and only 1 case had a poor result, which had a varus deformity due to loss of reduction. Out of 10 cases that were managed by open reduction, excellent result is seen in 4 cases (40%), good result is seen in 3 cases(30%),and poor result in 3(30%)cases. Poor result is seen in one case of fracture with vascular injury and in two cases that presented late with resolved compartment syndrome. The most probable causes of poor results are Vascular injury,Extensile incisions given for the vessel repair and grafting, Delayed mobilization,Delayed presentation with compartment syndrome, Decreases the pliability of the soft tissue preventing closed reduction aIatrogenic damage to soft tissue adds up to the stiffness. In summary excellent to good results were obtained in about 90% of cases of closed reduction and K wire fixation and excellent to good results in 70% of cases operated by open reduction and K wire fixation. The indication of open reduction remains limited because of risk of stiffness of injury due to iatrogenic soft tissue injury. It is recommended to limit lateral approach for prevention of stiffness which may be more common in posterior approach. Open reduction and internal fixation is an effective and safe method of treatment if indicated and is associated with good outcome. The concept of anatomical reduction and percutaneous pinning, followed by early and proper physiotherapy is the choice of obtaining excellent results functionally and cosmetically in Gartland’s type III supracondylar fracture humerus management in children. Shortcome of this study was cases size was small and and crossed and lateral pin construct are not equally used in both groups but this study clearly tells the indications for open reduction and k wire fixation and outcome in these cases. Conclusion: Fall on outstretched hand is the commonest cause and higher incidence in males and in non-dominant humerus. A minimum distance of 10mm at the fracture site should separate the K wires. The C-arm should be rotated, and not the arm to get an intra operative lateral view. The concept of gentle closed reduction and percutaneous K wire fixation followed by early physiotherapy is the treatment of choice for obtaining excellent results functionally and cosmetically in Gartland’s Type III supracondylar fractures of humerus in children. Open reduction through lateral approach and internal fixation wire K wires is safe and effective method of treatment, if indicated, in supracondylar fractures of humerus in children and is associated with a good outcome. A small incision medially in cases where medial epicondyle cannot be defined to visualize the epicondyle and the ulnar nerve ,by which iatrogenic ulnar nerve palsy in percutaneous fixation can be prevented. Observation and supportive therapy is the preferred initial approach in nerve injuries associated with this fracture. K wires can be removed safely at 3-4 weeks after injury and mobilization of the elbow should be started after the third week. CONFLICT OF INTEREST None of the authors has any conflict of interest. ACKNOWLEDGEMENTS The authors did not receive any funds for the preparation of this manuscript. References: 1. Cheng JC, Shen WY (1993) Limb fracture pattern in different pediatric age groups: a study of 3:350 children. J Orthop Trauma 7:15–22 2. Siris IE (1939) Supracondylar fractures of the humerus. An analysis of 330 cases. Surg Gynecol Obstet 68:201 3. Boyd DW, Aronson DD (1992) Supracondylar fractures of the humerus: a prospective study of percutaneous pinning. J Pedi- atr Orthop 12:789–794 4.Flynn JC, Matthews JG, Benoit RL (1974) Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am 56:263–272 5. Haddad RJ Jr, Saer JK, Riordan DC (1970) Percutaneous pin-ning of displaced supracondylar fractures of the elbow in chil-dren. Clin Orthop 71:112–117 6. Mehserle WL, Meehan PL (1991) Treatment of the displaced supracondylar fracture of the humerus (type III) with closed re- duction and percutaneous cross-pin fixation. J Pediatr Orthop 11:705–711 7. Nacht JL, Ecker ML, Chung SM, Lotke P A, Das M (1983) Supracondylar fractures of the humerus in children treated by closed reduction and percutaneous pinning. Clin Orthop 177:203–209 8. Peters CL, Scott SM, Stevens PM (1995) Closed reduction and percutaneous pinning of displaced supracondylar humerus frac- tures in children: description of a new closed reduction tech- nique for fractures with brachialis muscle entrapment. J Orthop Trauma 9:430–434 9. Pirone AM, Graham HK, Krajbich JI (1998) Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg Am 70:641–650 10. Wilkins KE, Beaty J. Fractures in Children. Philadelphia: Lippincott-Raven, 1996. 11. Cheng JC, Lam TP, Shen WY. Closed reduction and percutaneous pinning for type III displaced supracondylar fractures of the humerus in children. J Orthop Trauma 1995; 9(6):511-515 12. Culp RW, Osterman AL, Davidson RS et al: Neural injuries associated with supracondylar fractures of the humerus in children. J Bone and Joint Surg 72-A:1211-1215, 1990. 13. Lyons ST ,Quinn M, Stanitski CL. Neurovascular injuries in type III humeral supracondylar fractures in children. Clin Orthop Relat Res.2000 Jul;(376):62-7. 14. Reitman RD , Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures in children. J Pediatr Orthop. 2001 Mar-Apr;21(2):157-161. 15. Skaggs DL(1), Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT.Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement.J Bone Joint Surg Am. 2001 May;83-A(5):735-40. 16. Reynolds RA(1), Mirzayan R. A technique to determine proper pin placement of crossed pins in supracondylar fractures of the elbow. J Pediatr Orthop. 2000 Jul-Aug;20(4):485-9. 17. Flynn JC, Mathews JG, benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children : sixteen years experience with long term follow up. J Bone Joint Surg [Am] 1974; 56 A:26372 18. J.B. Yaokreha,P. Gicquel, L. Schneider , C. Stanchina , C. Karger ,E. Saliba , O. Ossenoua, J.-M. Clavert . Compared outcomes after percutaneous pinning versus open reduction in paediatric supracondylar elbow fractures . Orthopaedics & Traumatology: Surgery & Research (2012) 98, 645—651 Cases illustrations Case 1 Closed reduction and K wiring pinning. Post op Pre op At 4 month Case 2 open reduction and cross pinning 8 wks Post op Pre op A 4 months Tables 8 wks Table 1 Sl.No Mode Of Injury 1 Fall on outstretched hand No of Cases Percentage 8 40% 6 30% while playing 2 Slip and fall on outstretched hand 3 Fall from height 3 15% 4 R.T.A 3 15% Table 2 Sl.no construct No. of cases percentage 1. Lateral pinning 7 70% 2. Crossed pinning 3 30% Table 3 Sl.no construct No. of cases percentage 1. Lateral pinning 8 80% 2. Crossed pinning 2 20% Table 4 Sl.no Indication No of cases percentage 1. Failed closed reduction 4 40% 2. Vascular injury 3 30% 3. Delayed presentation(>1 wk) 3 30% Table 5 Result No of cases Percentage EXCELLENT 7 70% GOOD 2 20% FAIR 0 --- POOR 1 10% Table 6 Result No of cases Percentage EXCELLENT 4 40% GOOD 3 30% FAIR 0 --- POOR 3 30%