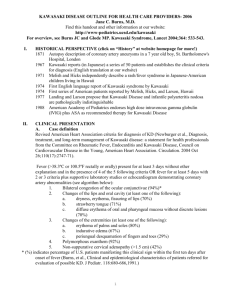
I. Clinical Diagnosis
advertisement

Doernbecher Children’s Hospital Kawasaki Disease Management Guidelines Division of Pediatric Infectious Diseases Division of Pediatric Cardiology Please consult both the Infectious Diseases and Cardiology services for all Kawasaki disease admissions. This is to be used as a guide in managing patients admitted with this diagnosis. I. Clinical Diagnosis The diagnosis of Kawasaki disease (KD) is based on the findings listed below. Please note that a patient may not manifest 4 clinical criteria (“Incomplete KD”), but has the same risk of coronary sequelae as a classic KD patient. Fever for > 5 days plus 4 out of 5 clinical criteria: 1. Polymorphous rash 2. Prominent cervical lymph node >1.5 cm, usually unilateral 3. Edema and/or erythema of hands and/or feet 4. Nonpurulent bilateral bulbar conjunctivitis 5. Oropharyngeal changes, including strawberry tongue II. Laboratory Evaluation The following labs are routinely used as supportive data: CBC with platelet and differential Liver set (liver function panel) ESR (sometimes CRP is useful if ESR is not elevated) Urinalysis (bagged specimen is acceptable if UTI is not on differential diagnosis) III. Treatment Goal is to treat patients within the first 10 days of fever. If a patient is diagnosed with KD beyond the 10th day of onset, treatment may still be recommended if the patient continues to display signs of ongoing systemic inflammation. Intravenous gamma globulin: 2 grams/kg single infusion High-dose oral aspirin: 80-100 mg/kg/day divided every 6 hours Nursing order for NO AXILLARY TEMPS, ONLY ORAL OR RECTAL (exception during IVIG infusion) On day #14 of illness and 48 hours after fever cessation, the oral aspirin dose is decreased to 3-5 mg/kg/dose qD. Day #14 is determined by counting from the first day of fever. For example, if a patient is diagnosed and treated on day #10 of fever and defervesces with IVIG, then he will receive only 4 days of high-dose aspirin. Low-dose aspirin should be continued until the 6-8 week follow-up appointment (minimum). If the echocardiogram, platelet count, and ESR are normal at the 6-8 weeks follow-up visit, then low-dose aspirin can be discontinued. IV. Initial echocardiogram All patients should have a baseline echocardiogram during hospital admission V. Follow-up Prior to hospital discharge, page or call Erin Merrifield, RN (Peds ID) to assist with scheduling the follow-up outpatient appointment. Erin will assist with coordinating the echocardiogram and ID appointment. o Ideally, the first follow-up appointment date/time should be scheduled prior to hospital discharge Patients should be scheduled for follow-up with Infectious Disease [Dr. Guzman-Cottrill (non-Kaiser) or Dr. Chun (Kaiser)] approximately 1-2 weeks after discharge home (at least 7 days following initial echo). A cardiology follow-up appointment should be scheduled approximately 6-8 weeks after illness onset. Remember to order annual influenza vaccine on day of discharge (specific indication: chronic ASA therapy) Patient should not receive any live vaccines for 11 months post-IVIG (Varicella and MMR) o o Patients will have an echocardiogram at the Infectious Disease clinic appointment Patients will have an echocardiogram, CBC with platelet, differential and ESR at the cardiology appointment revised 04/2011