Medical Surveillance SOP
advertisement
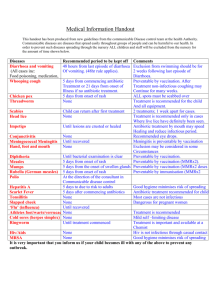
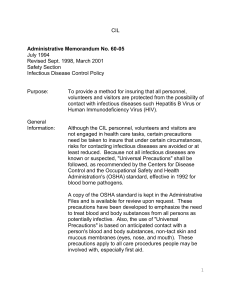
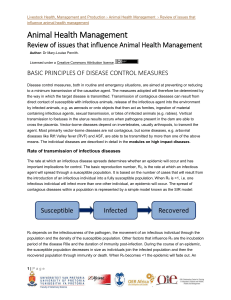
Medical Surveillance A Medical Surveillance Plan is an integral part of exposure control and Biosafety because it provides a foundation where employees can be monitored over time to ensure that they are not receiving occupational exposure and if they are exposed, it does not exceed the allowable limits. Should exposure exceeding allowable limits occur, especially as the result of an accident, misconduct or spill, it is the incident response plan will give insight into emergency response. Regardless of exposure however, all employees are represented under a medical surveillance plan that will monitor the employee over time to track their health as well as maintain their confidentiality. Risk Assessment Screening Questionnaire (RASQ) To efficiently assess health related risks with specific types of research, Cal Poly offers a Risk Assessment Screening Questionnaire to screen employees for risks such as pregnancy, immunosuppression, allergies etc. The benefit of using the RASQ is to maintain employee/patient confidentiality by screening them to determine if a Health History Questionnaire is required. Answering “YES” to any of the questions on the RASQ will trigger the need to complete a confidential Health History Questionnaire. Health History Questionnaire (HHQ) If the completion of a RASQ triggers the need to complete a confidential Health History Questionnaire (HHQ), the document can be filled out either securely online or on paper. Regardless of the method, all HHQ’s must be evaluated by a physician with the employee/patient present. The physician will be the only person to physically see the confidential medical information. The physician is responsible for making a health assessment on if the individual is fit and capable for the specific research in question. In this situation, the physician will give a simple “Pass” or “Fail” to the Institutional Biosafety Committee. A “Pass” will signify that the individual is healthy and physically able to perform the research in question, while a “Fail” will signify that the individual may be at a greater risk of health complications by performing the research or being exposed to a specific agent. The IBC does not need any confidential medical information, just the physician’s approval to grant the individual approval to work on the research in question. Exposure Incidents All employees are required to report all exposure incidents to the PI and RO immediately or within a reasonable time frame from the exposure incident. The PI and the RO will investigate and document each exposure incident. It is the responsibility of the PI and RO to ensure that all required information is transferred to the healthcare provider for post-exposure evaluation. This may include the following: 1. A copy of 29 CFR 1910.1030, OSHA’s Bloodborne Pathogen Standard, with emphasis on the confidentially requirements contained therein; 2. A written description of the exposed employee’s duties as they relate to the exposure incident; 3. Written documentation of the route of exposure and circumstances under which the exposure occurred; 4. Results of the source individual’s blood testing, if available; and 5. All medical records relevant to the appropriate treatment of the employee, including vaccination status. The healthcare provider shall provide a written opinion limited to: 1. A statement that the employee has been informed of the results of the evaluation; and 2. A statement that the employee has been told about any medical conditions resulting from the exposure or other potentially infectious materials that require further evaluation or treatment. Medical Follow-ups Any exposed employees shall immediately receive a confidential post-exposure evaluation and followup by a qualified healthcare provider determined by the employer. The evaluation and follow-up must include the following elements. 1. Documentation of the route of exposure, and the circumstances under which the exposure occurred. 2. Identification and documentation of the source individual, unless it can be established that identification is infeasible or prohibited by state or local law. 3. The source individual’s blood shall be tested and documented as soon as feasibly possible and after consent is obtained (if required) in order to determine HBV, HIV or other agent as necessary. If consent is required and cannot be established, the RO must document the lack of consent. 4. If an individual being tested is known to have HBV or HIV infection, blood tests are not required. Additional agents specific to the work at the time of exposure should be screened as well. 5. Test results shall be made available to the employee as well as informed of all applicable laws and regulations concerning the disclosure of infectious status. 6. Blood shall be collected as soon as possible and tested only after consent is given. 7. The employee has the option of being tested for HBV and HIV. Their blood shall be preserved for up to 90 days to allow the employee to decide if their blood should be tested. Initial/ Annual Screening for Infectious Disease If working with an infectious or disease causing agent, you will be medically tested (if a test is medically available) initially to ensure no previous exposure and tested annually thereafter until research ceases. Any research where M. Tuberculosis is likely to be used, requires medical monitoring pursuant to OSHA standards according to Aerosol & Transmissible Diseases. Vaccination Policy It is the University policy that all employees working with infectious materials where a vaccination exists should receive the vaccination at no cost. A declination process exists for those who still wish to decline vaccination provided those individuals are made aware of any and all risks associated with their declination. The employer will make vaccines available to all employees who have the potential for occupational exposure as well as post-exposure follow-up to employees who have experienced an exposure incident. 1. Working with Animals Employees working with animals must be trained and registered through the Animal Care and Use Committee (ACUC) to ensure that all employees are made aware of the hazards related to working with animals which include zoonotic diseases, aerosol transmissible diseases and blood borne pathogens. Special vaccinations may also be required when working with animals and can include the following: a. Tetanus A condition caused by Clostridium tetani, an anaerobic bacterium which secretes a neurotoxin, tetanospasmin which is responsible for causing severe muscle spasms. While tetanus is not spread by animals, the texture of metal (rusty or otherwise) is a suitable material for it to reside and can enter the body through a puncture wound from a piece of metal. A large part of proper animal handling requires handling and decontamination of animal cages which may increase an animal handler’s risk of contracting tetanus. b. Rabies A viral infection which causes acute encephalitis is a zoonotic disease which can be transferred by a bite from an infected animal. Rabies is almost always fatal in humans if post-exposure treatment is not administered prior to the onset of severe symptoms. The virus attacks the central nervous system and can cause disease within the brain in weeks to months after exposure. 2. Declination An employee may decline vaccination after being appropriately trained and made aware of any risks and hazards for their specific lab duties. Should the employee still wish to decline vaccination, a declination form must be completed and submitted to the RO. Tier 1 BSAT workers Those that are approved to work with BSAT Tier 1 must be enrolled in the occupational health program for BSAT workers which require initial examinations, and medical surveillance. Contact EH&S for more information.