Chapter 8 Nursing Care of Women with Complications During Labor
advertisement

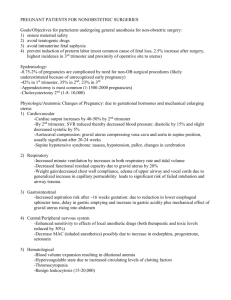
• • • • • • • • Chapter 8 Nursing Care of Women with Complications During Labor and Birth Obstetric Procedures Amnioinfusion – – – – – Oligohydramnios Umbilical cord compression Reduction of recurrent variable decelerations Dilution of meconium-stained amniotic fluid Replaces the “cushion” for the umbilical cord and relieves the variable decelerations Obstetric Procedures (cont.) Amniotomy – – – – – The artificial rupture of membranes Done to stimulate or enhance contractions Commits the woman to delivery Stimulates prostaglandin secretion Complications • • • Prolapse of the umbilical cord Infection Abruptio placentae Obstetric Procedures (cont.) Observe for complications post-amniotomy • • • • • • • • • • • • • • • – – – – Fetal heart rate outside normal range (110-160 beats/min) suggests umbilical cord prolapse Observe color, odor, amount, and character of amniotic fluid Woman’s temperature 38° C (100.4° F) or higher is suggestive of infection Green fluid may indicate that the fetus has passed a meconium stool Nursing Tip Observe for wet underpads and linens after the membranes rupture. Change them as often as needed to keep the woman relatively dry and to reduce the risk for infection or skin breakdown. Induction or Augmentation of Labor Induction is the initiation of labor before it begins naturally Augmentation is the stimulation of contractions after they have begun naturally Indications for Labor Induction Gestational hypertension Ruptured membranes without spontaneous onset of labor Infection within the uterus Medical problems in the woman that worsen during pregnancy Fetal problems such as slowed growth, prolonged pregnancy, or incompatibility between fetal and maternal blood types Placental insufficiency Fetal death Contraindications to Labor Induction Placenta previa • • • • • • • • • • • • • • Umbilical cord prolapse Abnormal fetal presentation High station of the fetus Active herpes infection in the birth canal Abnormal size or structure of the mother’s pelvis Previous classic cesarean incision Pharmacological Methods to Stimulate Contractions Cervical ripening – – Prostaglandin in a gel or vaginal insert is applied before labor induction to soften the cervix Laminaria is an alternative to cervical ripening by swelling inside the cervix Oxytocin induction and the augmentation of labor – – Used to initiate or stimulate contractions Most commonly used method Benefit of Augmentation Usually requires less total oxytocin than induction Uterus is more sensitive to the drug when labor has already begun Nonpharmacological Methods to Stimulate Contractions Walking – – – Stimulates contractions Eases pressure of the fetus on the mother’s back Adds gravity to the downward force of contraction • • • • • • • • • • • • • Nipple stimulation of labor – Causes the pituitary gland to secrete natural oxytocin Complications of Oxytocin Induction and Augmentation of Labor Most common is related to – Overstimulation of contractions • • Fetal compromise Uterine rupture Water intoxication – Inhibits excretion of urine and promotes fluid retention Bishop’s Scoring System Evaluates the cervical response to induction procedures A high score (above 6) is predictive of successful labor induction because the cervix has ripened or softened in preparation for labor Version A method used to change fetal presentation – Two methods • • External Internal Risks and Contraindications of Version Disproportion between mother’s pelvis and fetal size Abnormal uterine or pelvic size or shape Abnormal placental placement • • • • • • • • • • • • • • • • • • • • Previous cesarean birth with vertical uterine incision Active herpes virus infection Inadequate amniotic fluid Poor placental function Multifetal gestation Fetus can become entangled in umbilical cord Episiotomy and Lacerations Episiotomy—controlled surgical enlargement of the vaginal opening during birth Lacerations—uncontrolled tear of the tissues that results in a jagged wound Perineal Lacerations First degree—superficial vaginal mucosa or perineal skin Second degree—involves vaginal mucosa, perineal skin, and deeper tissues of the perineum Third degree—same as second degree, plus involves anal sphincter Fourth degree—extends through the anal sphincter into the rectal mucosa Episiotomies Indications for an Episiotomy Better control over where and how much the vaginal opening is enlarged An opening with a clean edge rather than the ragged opening of a tear Note: Perineal massage and stretching exercises before labor may be an alternative to an episiotomy Forceps Extraction • • • • • • • • • • • • • • • • • • Provides traction and rotation of the fetal head when the mother’s pushing efforts are insufficient to accomplish a safe delivery Forceps may also help the physician extract the fetal head through the incision during a cesarean birth Forceps to Assist the Birth of the Fetal Head Vacuum Extraction Birth Uses suction applied to the fetal head so the physician can assist the mother’s expulsive efforts Used only with occiput presentation Vacuum Extraction Birth (cont.) Risks of Forceps or Vacuum Extraction Trauma to maternal or fetal tissues Mother may have a laceration or hematoma in her vagina Infant may have bruising, facial or scalp lacerations or abrasions, cephalhematoma, or intracranial hemorrhage Cesarean Birth The surgical delivery of the fetus through incisions in the mother’s abdomen and uterus Indications for Cesarean Birth Abnormal labor Inability of the fetus to pass through the mother’s pelvis Maternal conditions such as GH or DM Active maternal herpes virus • • • • • • • • • Previous surgery on the uterus Fetal compromise Placenta previa or abruptio placentae Risks of Cesarean Birth Mother – – – – – – – Anesthesia Respiratory complications Hemorrhage Blood clots Injury to urinary tract Delayed intestinal peristalsis Infection Neonate – – – Inadvertent preterm birth Respiratory problems because of delayed absorption of lung fluid Injury Types of Incisions Skin – – Vertical allows more room for a large fetus Transverse (a.k.a. Pfannenstiel) Uterine – – – • • • • • • • • • • • • • • • • Low transverse: not likely to rupture during another birth; VBAC possible with this type Low vertical: minimal blood loss; more likely to rupture during another birth Classic: rarely used; more blood loss; most likely to rupture during another pregnancy Sequence of Events in Cesarean Birth Cesarean Section Birth Woman may need more emotional support Emotional care of the partner and family is essential Nursing Care in the Recovery Room Vital signs to identify hemorrhage or shock IV site and rate of solution flow Fundus for firmness, height, and midline position Dressing for drainage Lochia for quantity, color, and presence of clots Urine output from the indwelling catheter Safety Alert Although assessing the uterus after cesarean birth causes discomfort, it is important to do so regularly The woman can have a relaxed uterus that causes excessive blood loss, regardless of how she delivered her child Abnormal Labor Called dysfunctional labor • • • • • • • • • • • • • – Does not progress Dystocia – Difficult labor Risk Factors for Dysfunctional Labor Advanced maternal age Obesity Overdistention of uterus – Hydramnios or multifetal pregnancy Abnormal presentation Cephalopelvic disproportion (CPD) Overstimulation of the uterus Maternal fatigue, dehydration, fear Lack of analgesic assistance Problems with the Powers of Labor Hypertonic – – – – Increased muscle tone Usually occurs during the latent phase of labor Characterized by contractions that are frequent, cramplike, and poorly coordinated Painful but nonproductive • Uterus is tense, even between contractions, leads to reduced blood flow to the placenta Hypotonic – – – Decreased muscle tone Labor begins normally, but diminishes during active phase More likely to occur if uterus is overdistended • • • • • • • • • • • • • Ineffective Maternal Pushing Woman may not understand which technique to use or fears tearing her perineal tissues Epidural or subarachnoid blocks may depress or eliminate the natural urge to push An exhausted woman may be unable to gather enough energy to push Problems with the Fetus Fetal Size Macrosomia—large fetus; weighs more than 4000 g (8.8 pounds) – – • • May not fit through birth canal Can contribute to hypotonic labor dysfunction Shoulder Dystocia Usually occurs when fetus is too large Is an emergency Fetal chest cannot expand and the fetus needs to be able to breathe After delivery, mother and infant need to be assessed for injuries – – – • Stretches the muscle fibers and reduces their ability to contract effectively Mother may have torn perineal tissue More at risk for uterine atony and postpartum hemorrhage • Uterus does not contract well after birth Infant may have fractured clavicle Abnormal Fetal Presentation or Position Prevents the smallest diameter of the fetal head to pass through the smallest diameter of the pelvis Abnormal Presentations • • • • • • • • • • • • • • • • Does not pass easily Interferes with most efficient mechanisms of labor Can cause cord compression May require external version Abnormal Positions Common cause is a fetus that remains in a persistent occiput posterior position Labor may last longer Woman may experience intense and poorly relieved back and leg pain May require forceps-assisted delivery Breech Birth Nursing Care for Abnormal Fetal Presentation or Positions Encourage woman to assume positions that favor fetal rotation and descent and reduce back pain – – – – – Sitting, kneeling, or standing while leaning forward Rocking the pelvis back and forth while on hands and knees (encourages rotation) Side-lying Squatting (in second stage of labor) Lunging by placing one foot in a chair with the foot and knee pointed to that side Multifetal Pregnancy May cause dysfunctional labor Uterine overdistention contributes to poor contraction quality Abnormal presentation or position of one or more fetuses interferes with labor mechanisms • • • • • • • • • • • Often one fetus is delivered as cephalic and the second as breech, unless a version is done Problems with the Pelvis and Soft Tissues Bony pelvis – Gynecoid pelvis most favorable for vaginal birth Soft tissue obstructions – Most common is a full bladder The Psyche Most common factors that can prolong labor – – – – Lack of analgesic control of excessive pain Absence of a support person or coach Immobility and restriction to bed Lack of ability to carry out cultural traditions Increased Anxiety Causes hormones to be released – – – Epinephrine Cortisol Adrenocorticotropic Reduces contractility of the smooth muscle Effects of Hormones Released The uterus uses more glucose for energy • • • • • • • • • • • • • • Diverts blood from the uterus Increases tension of pelvic muscles; can impede fetal descent Increases perception of pain Abnormal Duration of Labor Friedman’s curve – – Often used to graph the progress of cervical dilation and fetal descent Used as a guide to assess and manage the normal progress of labor Prolonged labor can cause – – – – Maternal or newborn infection Maternal exhaustion Postpartum hemorrhage Greater anxiety and fear Precipitate Birth A birth that is completed in less than 3 hours Labor begins abruptly and intensifies quickly Contractions may be frequent and intense May have uterine rupture, cervical lacerations, or hematoma Fetal oxygenation may be compromised Birth injury may occur from rapid passage through the birth canal Injuries can include – – Intracranial hemorrhage Nerve damage • • • • • • • • • • • • • • • • • • Premature Rupture of Membranes (PROM) Spontaneous rupture of membranes at term, more than 1 hour before labor contractions begin Vaginal or cervical infection may cause PROM Diagnosis confirmed by – – Nitrazine paper test Looking for a “ferning” pattern from vaginal fluid placed on a slide and viewed under the microscope Patient Teaching for a Woman with Infection or in Preterm Labor Report a temperature that is above 38° C (100.4° F) Avoid sexual intercourse or insertion of anything into vagina Avoid orgasms Avoid breast stimulation Maintain any activity restrictions prescribed Note any uterine contractions, reduced fetal activity, and other signs of infection Record fetal kick counts daily and report fewer than 10 kicks in a 12-hour period Preterm Labor Occurs after 20 weeks and before 37 weeks gestation Main risks are problems of immaturity in the newborn Signs of Impending Preterm Labor A shortened cervix on ultrasound at 20 weeks may be predictive of preterm labor A fibronectin test – – • • • • • • • • • • • • • • • • • • • • The presence of fibronectin in vaginal secretions between 22 and 24 weeks gestation is predictive of preterm labor Fibronectin is a protein produced by the fetal membranes that can leak into vaginal secretions if uterine activity, infection, or cervical effacement occurs Maternal Symptoms of Preterm Labor Contractions that may be either uncomfortable or painless Feeling that the fetus is “balling up” frequently Menstrual-like cramps Constant low backache Pelvic pressure or a feeling that the fetus is pushing down A change in vaginal discharge Abdominal cramps with or without diarrhea Pain or discomfort in the vulva or thighs “Just feeling bad” or “coming down with something” Some Risk Factors for Preterm Labor Exposure to DES Underweight Chronic illness Dehydration Preeclampsia Previous preterm labor or birth Previous pregnancy losses Substance abuse Chronic stress • • • • • • • • • • • • • • • • • • Infection Anemia Preterm PROM Inadequate prenatal care Poor nutrition Low education level Poverty Smoking Multifetal presentation Tocolytic Therapy Goal is to stop uterine contractions Keep fetus in utero until lungs are mature enough to adapt to extrauterine life Magnesium sulfate IV drug of choice Beta-adrenergic drugs given orally Calcium channel blockers given orally Contraindications – – – – – Preeclampsia Placenta previa Abruptio placentae Chorioamnionitis Fetal demise Stopping Preterm Labor Initial measures to stop preterm labor • – – – • • • – Hydration Steroids increase fetal lung maturity • Betamethasone Thyroid-releasing hormone also enhances lung maturity in fetuses younger than 28 weeks Prolonged Pregnancy Lasts longer than 42 weeks Risks Placenta ages – – – – • • Activity restriction If it appears preterm birth is inevitable – • Identifying and treating infection Delivers oxygen and nutrients to the fetus less efficiently • • Fetus may lose weight Fetal skin may peel Fetus continues to grow Meconium may be expelled Low blood glucose levels in the fetus Tests Used to Confirm the Diagnosis of Prolonged Pregnancy Any pregnancy that lasts longer than 40 weeks may require – – – Nonstress tests (NST) Amniotic fluid index (AFI) Biophysical profiles (BPP) • • • • • • • • • • • – Kick counts Emergencies During Childbirth Prolapsed umbilical cord – – – Complete Palpated Occult Uterine rupture – – – Complete Incomplete Dehiscence Prolapsed Umbilical Cord Nursing Care of a Woman with Umbilical Cord Prolapse Uterine Inversion Uterus turns inside out after delivery of the infant Most likely to occur – – If the uterus is not firmly contracted During vigorous fundal massage Amniotic Fluid Embolism Occurs when amniotic fluid, with its particles such as vernix, fetal hair, and sometimes meconium, enter the woman’s circulation and typically obstructs small blood vessels in her lungs Characterized by abrupt onset of hypotension, respiratory distress, and coagulation abnormalities • • Question for Review What nonpharmacological techniques can be used to stimulate labor?