[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
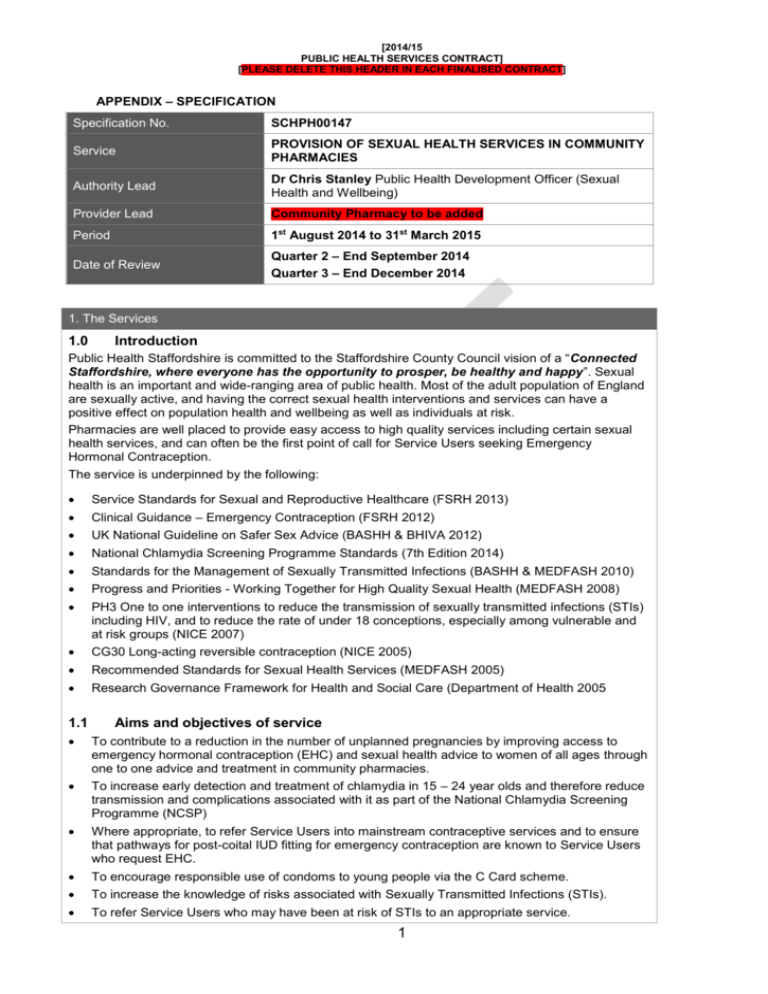
APPENDIX – SPECIFICATION
Specification No.
SCHPH00147
Service
PROVISION OF SEXUAL HEALTH SERVICES IN COMMUNITY
PHARMACIES
Authority Lead
Dr Chris Stanley Public Health Development Officer (Sexual
Health and Wellbeing)
Provider Lead
Community Pharmacy to be added
Period
1st August 2014 to 31st March 2015
Date of Review
Quarter 2 – End September 2014
Quarter 3 – End December 2014
1. The Services
1.0
Introduction
Public Health Staffordshire is committed to the Staffordshire County Council vision of a “Connected
Staffordshire, where everyone has the opportunity to prosper, be healthy and happy”. Sexual
health is an important and wide-ranging area of public health. Most of the adult population of England
are sexually active, and having the correct sexual health interventions and services can have a
positive effect on population health and wellbeing as well as individuals at risk.
Pharmacies are well placed to provide easy access to high quality services including certain sexual
health services, and can often be the first point of call for Service Users seeking Emergency
Hormonal Contraception.
The service is underpinned by the following:
Service Standards for Sexual and Reproductive Healthcare (FSRH 2013)
Clinical Guidance – Emergency Contraception (FSRH 2012)
UK National Guideline on Safer Sex Advice (BASHH & BHIVA 2012)
National Chlamydia Screening Programme Standards (7th Edition 2014)
Standards for the Management of Sexually Transmitted Infections (BASHH & MEDFASH 2010)
Progress and Priorities - Working Together for High Quality Sexual Health (MEDFASH 2008)
PH3 One to one interventions to reduce the transmission of sexually transmitted infections (STIs)
including HIV, and to reduce the rate of under 18 conceptions, especially among vulnerable and
at risk groups (NICE 2007)
CG30 Long-acting reversible contraception (NICE 2005)
Recommended Standards for Sexual Health Services (MEDFASH 2005)
Research Governance Framework for Health and Social Care (Department of Health 2005
1.1
Aims and objectives of service
To contribute to a reduction in the number of unplanned pregnancies by improving access to
emergency hormonal contraception (EHC) and sexual health advice to women of all ages through
one to one advice and treatment in community pharmacies.
To increase early detection and treatment of chlamydia in 15 – 24 year olds and therefore reduce
transmission and complications associated with it as part of the National Chlamydia Screening
Programme (NCSP)
Where appropriate, to refer Service Users into mainstream contraceptive services and to ensure
that pathways for post-coital IUD fitting for emergency contraception are known to Service Users
who request EHC.
To encourage responsible use of condoms to young people via the C Card scheme.
To increase the knowledge of risks associated with Sexually Transmitted Infections (STIs).
To refer Service Users who may have been at risk of STIs to an appropriate service.
1
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
To strengthen the local network of contraceptive and sexual health services to help ensure easy
and swift access to advice.
1.2
Service description/pathway
In all cases, people declaring symptoms suggestive of sexual ill health should be risk assessed and
managed appropriately. This may include referral to specialist sexual health services.
Levonorgestrel 1.5mg, Ulipristal acetate 30mg and Azithromycin must only be prescribed by an
accredited pharmacist who has completed the training specified, under the current Patient Group
Directions authorised by Staffordshire Public Health.
It is expected that there will be a named lead within each participating pharmacy responsible for
responding to queries relating to EHC and Chlamydia screening and testing. The named lead will
act as the Governance Lead and Champion for the service(s).
1.2.1
EHC provision
To provide, where clinically indicated, a free supply of EHC as specified within the Patient Group
Direction (PGD) for Levonorgestrel or Ulipristal acetate.
The pharmacist must provide the service in person. Medicine counter staff must refer all such
Service Users to the accredited pharmacist without delay.
If an accredited pharmacist is unavailable the Service User should be informed when an
accredited pharmacist will be available or signposted to an alternative service where EHC can be
obtained or post-coital IUD can be fitted (list in EHC support pack).
Service Users attending an accredited pharmacist should be given access to the service even
where this may mean that the consultation is completed after opening hours. This is at the
discretion of the pharmacist who should always ensure the safety of the Service User, staff and
themselves. If this is not possible pharmacists should advise the Service User of a timely
alternative source of EHC or post-coital IUD.
The pharmacist takes a Service User history to ensure that they have sufficient information to
assess the appropriateness of the supply.
If the pharmacist is satisfied that emergency contraception is appropriate and that the Service
User understands the circumstances in which emergency contraception will be effective, the
pharmacist supplies, according to the PGD, Levonorgestrel 1.5mg as a single dose within 72
hours, or Ulipristal acetate 30mg as a singe dose between 72 – 120 hours of unprotected sexual
intercourse.
The product may only be supplied to be taken on the premises of the pharmacy and should not be
supplied for possible future use.
The pharmacist must ensure that the Service User is counselled on other sexual health matters
and related topics. Written information should also be available on these topics. Referral with local
sexual health services should be made as appropriate.
The pharmacist must ensure maintenance of records for each supply and may be required to
share information with appropriate parties in line with confidentiality protocols.
The pharmacist must use their professional judgement to consider, and where appropriate, act on
any safeguarding children issues coming to their attention as a result of providing the service.
This should be in line with local safeguarding children procedures and any national or local
guidance on sexual activity in the under 16s.
The Sexual Offences Act 2003 states that no child under 13 years is able to consent to any
sexual activity. If a child under 13 years of age requests EHC, the pharmacist taking the
consultation must keep accurate records, and if there is a reasonable concern that sexual activity
has taken place, the pharmacist should always speak to their identified child protection lead or
senior manager within their pharmacy. There must always be a presumption that the case will be
referred to the Children’s Social Care Services in the area where the child lives (see the
Flowchart at the end of this specification). If a decision is made not to refer following discussion
with the safeguarding lead/senior manager, then the reasons should be fully
documented. However, the duty to safeguard the child from most harm would include protecting
them from an unintended pregnancy, so providing that they have been assessed as “Fraser
2
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
competent”, treatment should not be withheld.
If, after receiving all the necessary information, the Service User does not wish to take the tablet
they should be advised to see their GP or attend a Contraceptive & Sexual Health clinic as an
emergency. It should be documented that they did not wish to proceed and a claim for the
consultation only can still be made. Some Service Users may want time to consider their options
and therefore are free to leave the pharmacy and return later when they have made their
decision.
If, on the grounds of moral or religious beliefs a pharmacist does not supply Emergency Hormonal
Contraception (EHC), women must be referred to an alternative appropriate source of supply
available within the time limits for EHC to be effective and which will not compromise the woman’s
contraceptive cover.
1.2.2
Chlamydia Screening
The objective of the service is to reduce onward transmission, and the consequences of untreated
infection in young, sexually active men and women:
Chlamydia screening should always be offered as part of the Emergency Hormonal Contraception
service and be proactively offered with all existing services / sales in under 25s that are
appropriate for offering a Chlamydia screen e.g., contraceptive pill prescriptions and condom
sales
Service Users under the age of 25 years should be advised about the risks associated with
undiagnosed Chlamydia, supplied with National Chlamydia Screening Programme (NCSP) test
kits and strongly encouraged to undertake the screening test and return the postal Chlamydia
screening kit to the NCSP lab as directed within the pack.
Pharmacists should seek to increase the understanding and awareness of the importance of
reducing the risk of transmission of Chlamydia and other sexually transmitted infections.
1.2.3 Chlamydia treatment
To treat eligible young people aged 16-24 years who have been diagnosed with Chlamydia
trachomatis following the PGD for the supply of Azithromycin.
Azithromycin can only be supplied under the PGD by an accredited pharmacist who has
completed the training specified.
To screen and treat all partners of young people diagnosed with Chlamydia trachomatis following
the Azithromycin PGD.
The pharmacist must provide the service in person. Medicine counter staff must refer all such
Service Users to the accredited pharmacist.
If providing treatment, the pharmacist must initiate the Partner Notification process using the
BClear “Management of Chlamydia Positive Clients” forms which will be supplied to all
participating pharmacies
If an accredited pharmacist is unavailable the Service User should be informed when an
accredited pharmacist will be available or signposted to an alternative service where treatment
can be obtained.
All eligible Service Users are given sexual health advice and the importance of treating all current
and previous partners is stressed. Service Users should be encouraged to notify current and
recent partners.
As Service Users who have tested positive for Chlamydia are also at increased risk of having
contracted other sexually transmitted infections, all eligible Service Users should be referred on
and encouraged to attend local GUM services.
1.2.4
Condom Provision
Pharmacists are encouraged to be distribution sites for free condoms to under 25 year olds, ideally
through the C-Card condom distribution scheme where it is in place. This enables pharmacies to
provide 13-25 year olds who have registered with the scheme free condoms on presentation of their
C-Card. At present, the C-Card scheme only operates in the north of Staffordshire; pharmacies in the
south of Staffordshire will be notified when the scheme is implemented in their area.
3
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
1.3
Population covered
The EHC service is for all women presenting at the pharmacy irrespective of home location or GP
practice.
The pharmacy will offer the service to all women of all ages including under 16 year olds seeking
advice or information taking into account appropriate accreditation and issues around Fraser
competencies and Safeguarding.
The NCSP Chlamydia Screening Programme is for all people aged 15-24 presenting at the
pharmacy irrespective of home location or general practice (GP).
1.4
Any acceptance and exclusion criteria
The Provider has the right to refuse service provision to the users for any unreasonable behaviour
unacceptable to the Provider, its staff, or the named professional clinically responsible for the
management of the care of such Service User.
1.4.1
EHC service acceptance
The EHC service is available to all women who think they may be at risk of pregnancy and who if
under 16 are deemed competent to consent to treatment (refer to Fraser guidelines)
Whilst there is no limit to the number of times a Service User can access the EHC service
pharmacists must use their discretion when faced with repeat attendees. It must be stressed to
the Service User that it is an emergency measure only and as above, they should see their GP or
the Contraceptive & Sexual Health (CASH) Service to discuss regular methods of contraception.
1.4.2
EHC service exclusion
Women who are unsuitable for treatment under the conditions of the PGD or this service
specification.
Women aged 16 and under who are deemed not competent to consent to treatment (See Fraser
guidelines in EHC Support Pack)
Women who have not validly consented to the treatment provided under the Services
Friends, relatives or third parties requesting EHC on behalf of the intended user
The EHC should not be supplied for possible future use.
If the Service User requires EHC but is excluded from supply under the PGD they should be advised
to see their GP or attend a Contraceptive & Sexual Health clinic as an emergency. They should also
be offered information and advice on how to access local Contraceptive & Sexual Health Services,
GPs and the GU Medicine Service. A claim can still be made for the consultation only, provided it is
documented as to why a supply wasn’t made.
1.4.3
Chlamydia screening and treatment service acceptance
Any young person who is identified as sexually active between 15 and 24.
A person of any age who is identified as a partner of a young person (15-24) who has tested
positive for Chlamydia
1.4.4
Chlamydia screening and treatment service exclusion
Service Users who are unsuitable for treatment under the conditions of the PGD or this service
specification
Individuals with symptoms of sexually transmitted infections (who should be redirected to GP or
GUM)
Individuals outside the target age group of the Programme (other than partners of those NCSP
Service Users who have tested positive)
Young people under the age of 16 years deemed not competent to consent to treatment (See
4
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
Fraser guidelines in EHC Support Pack)
1.5
Interdependencies with other services
The Service User should be made aware of the need to consider long term methods of
contraception and the support and follow up that is available to them through the Contraceptive &
Sexual Health (CASH) Services, their own GP and the GU Medicine Service.
Individuals with symptoms of sexually transmitted infections should be advised to immediately
access the local GUM services.
Other services which may refer people in to this service such as school nursing, or which may
also be suitable for further referral such as alcohol, lifestyle, mental health services.
5
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
2. Key Service Outcomes and Quality Requirements
ACTIVITY OUTCOMES DATA
Outcome indicator
Threshold
Method of
measurement
PharmOutcomes
report
Consequence of
breach
n/a
Number of consultations
where supply made of
Levonorgestrel
n/a
Number of consultations
where supply made of
Ulipristal acetate 30mg
n/a
PharmOutcomes
report
n/a
Number of consultations
where EHC not supplied
n/a
PharmOutcomes
report
n/a
Percentage of chlamydia kits
offered to EHC service users
aged 15-24
100%
PharmOutcomes
report
Remedial Action
Plan
Percentage of chlamydia kits
accepted by EHC service
users aged 15-24
90%
PharmOutcomes
report
Remedial Action
Plan
Number of tests received at
laboratory from pharmacy
service users
No of consultations where
supply made of Azithromycin
for Chlamydia treatment
Number of referrals made to
GP/CASH for LARC fitting
n/a
PharmOutcomes
report
n/a
n/a
PharmOutcomes
report
n/a
To establish a
baseline for future
activity.
To be established
upon
implementation of
condom
distribution
scheme
To be established
upon
implementation of
condom
distribution
scheme
PharmOutcomes
report
n/a
PharmOutcomes
report
Remedial Action
Plan
% EHC consultation where
free condoms were supplied
% Chlamydia treatment
consultation where free
condoms were supplied
PharmOutcomes
report
QUALITY STANDARDS
Data item
Purpose
Threshold
Identification of a clinical governance lead for
EHC provision and Chlamydia screening
All staff delivering EHC to have completed
relevant CPPE courses/refresher training
within last 3 years
Care pathways to other services defined and
referrals made where appropriate.
Achieve or maintain Young people friendly
standards e.g. You’re Welcome/DASH
Maintain or achieve LGB friendly standards
e.g. Rainbow Charter
Quality
indicator
Quality
indicator
Name
provided
Evidence
provided
Consequence
of breach
Remedial
action plan
Remedial
action plan
Quality
indicators
Quality
indicator
Quality
indicator
Assurance
given
Assurance
given
Assurance
given
Remedial
action plan
Remedial
action plan
Remedial
action plan
6
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
Information/feedback forms (to be provided by
the Authority) handed out to all EHC and
Chlamydia treatment service users.
Number of service users making formal
complaints about the service (verbal or
written)
Serious incidents/ near misses to be reported
to the commissioner within contract specified
timescales.
Compliance with safeguarding policies and
processes (children and adults in vulnerable
circumstances)
Quality
indicator
Assurance
given
Remedial
action plan
Quality
indicator
0
Learning and
action plan
Quality
indicator
0
Learning and
action plan
Quality
indicator
Assurance
given
Remedial
action plan
N.B. – Assurance standards to be reported annually via a template to be supplied by the
Authority
3. Applicable Service Standards
3.1
Standards required (including NCSP core requirements for Chlamydia screening and
treatment)
Pharmacies providing any element of these sexual health services should:
Ensure that staff are appropriately trained to deliver the services.
Offer user friendly, non judgemental, Service User centred and confidential services
Adhere to national and local requirements regarding the management of under 18s, including
use of the Department of Health’s You’re Welcome quality criteria1 and local resources where
available, as guiding principles when planning and implementing changes and improvements,
in order for the service to become young people friendly where appropriate.
Achieve or work towards bronze award criteria of Staffordshire Buddies “Rainbow Charter
Mark”2 to ensure that lesbian, gay and bisexual Service Users are treated fairly and able to
discuss issues openly with service providers.
Utilise and prominently display relevant national and local sexual health, emergency
contraception and chlamydia screening materials.
Provide people testing for chlamydia with an information leaflet as part of the consent process
Be responsible for ensuring timely onward referral for those people who they are not able to
manage.
Be responsible for providing all mandatory data reporting to the local coordination.
Be responsible for undertaking a satisfactory system of audit in line with the annual
requirements to audit key performance indicators of the programme
Always include consultation with service users and local populations for any service planning
and improvement
3.2
Pharmacy (premises) requirements
The service will only be provided in a pharmacy with a suitable NHS England accredited consultation
area. To confirm an approved consultation area is available the pharmacist will complete a
registration form indicating the full postal address of the premises and confirming the availability of a
‘private’ area for consultation that meets the criteria stipulated in the Community Pharmacy
Contractual Framework for Medicines Use Reviews (MURs).
3.3
Pharmacist accreditation
Department of Health (2011).You’re Welcome: Quality Criteria for Young People Friendly Health Services
(http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_126813)
1
2
Staffordshire Buddies “Rainbow Charter Mark” http://www.staffordshirebuddies.co.uk/health/rcm.htm
7
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
The pharmacy contractor has a duty to ensure that pharmacists and staff involved in the provision of
the service have the relevant knowledge and are appropriately trained in the operation of the service.
Accredited training specified by the Authority must be completed satisfactorily by the pharmacist
before the service may be provided.
3.3.1
3.3.2
3.3.3
3.3.4
For provision of any of the above sexual health services, the accredited pharmacists
delivering the service will:
Be registered with the General Pharmaceutical Council, based within registered premises.
Only provide the service in a Pharmacy that is signed up to the service with The Authority.
Have provided evidence of their enhanced DBS clearance
Have completed the CPPE distance learning pack on Safeguarding, and provided The
Authority with a copy of their certificate.
Be expected to attend safeguarding training and other relevant training events organised
by the Authority or the Local Pharmaceutical Committee.
Additionally, for provision of the EHC service, the accredited pharmacists delivering the
service will have:
Passed the CPPE e-assessment “Emergency Hormonal Contraception” or “Emergency
Contraception”, and provided The Authority with a copy of their certificate. The CPPE elearning Emergency Contraception can be used to support pharmacists preparing for this
e-assessment
Read the PGDs for Levonorgestrel and Ulipristal acetate, and sent a signed declaration to
Additionally - to provide Ulipristal acetate 30mg , pharmacists must have completed the
EHC e-assessment which covered supply of Ulipristal acetate (as introduced in 2013).
Pharmacists may wish to complete the CPPE e-learning “Dealing with Difficult
Discussions” to aid them in delivering sexual health services.
Additionally, for provision of the Chlamydia treatment service, the accredited pharmacists
delivering the service will have:
Completed the downloadable CPPE open learning “Sexual Health in Pharmacies”.
Read the PGD for Azithromycin, and sent a signed declaration to The Authority
All pharmacists must return the relevant documentation to:
Dr Chris Stanley
Public Health Development Officer (Sexual Health and Wellbeing)
Public Health Staffordshire,
Staffordshire County Council,
Wedgwood Building,
Tipping Street,
Stafford, ST16 2DH.
3.4
Review/Audit
The services delivered by this contract will be subject to clinical audit as appropriate or necessary.
Ongoing monitoring will be carried out through PharmOutcomes, and through assurances within an
annual report template (to be provided by Public Health Staffordshire).
8
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
4. Payment of the Charges
4.1
In accordance with the provisions of clause 8 of the Contract (Charges and Payment), the
Charges will be:
4.2
EHC provision
Each consultation will be remunerated at the cost of £14.
Each issuing of Levonorgestrel 1.5mg tablets or Ulipristal acetate 30mg will be
remunerated at the current drug tariff list plus VAT (5%)
4.2
Chlamydia Screening
4.3
£10 per test received at NCSP lab.
Chlamydia Treatment
Each consultation will be remunerated at the cost of £6
Each issuing of Azithromycin will be remunerated at the current drug tariff list plus VAT
(5%)
5. Required Insurances
5.1
As a minimum, the levels of cover are:
5.1.1
Public liability insurance with a limit of indemnity of not less than £5 million in relation
to any one claim or series of claims;
5.1.2
Employer's liability insurance with a limit of indemnity of not less than £5 million; and
5.1.3
Professional indemnity insurance with a limit of indemnity of not less than £2 million
in relation to any one claim or series of claims and shall ensure that all professional
consultants and sub-contractors involved in the provision of the Services hold and
maintain appropriate cover.
6. Representatives
6.1
6.2
6.3
The person set out below is authorised from the Commencement Date to act on behalf of the
Authority on all matters relating to this Contract (the “Authority Representative”).
Name:
Dr Chris Stanley
Title:
Public Health Development Officer (Sexual Health and Well-being)
Telephone:
01785 854625
Email:
chris.stanley@staffordshire.gov.uk
The person set out below is authorised from the Commencement Date to act on behalf of the
Provider on all matters relating to this Contract (the “Provider Representative”).
Name:
[insert name]
Title:
[insert title]
Telephone:
[insert]
Email:
The Provider may replace the Provider Representative and the Authority may replace the
Authority Representative at any time by giving written notice to the other Party.
7. Population Needs
7.1
The rate for under- 18 conceptions is reducing, but remains slightly higher than the England
average. Abortion rates and teenage pregnancy rates in some areas of Staffordshire are
9
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
7.2
7.3
7.4
7.5
significantly higher than the England average.
There are a high proportion of repeat abortions in Staffordshire which may indicate issues with
access to contraceptive services.
Trends in under-16 conceptions in Staffordshire show a 7% reduction in rates between 20012003 and 2009-2011 across Staffordshire compared with a 14% reduction nationally.
Local authorities are required to provide STI testing services, and this includes chlamydia
testing. Chlamydia is the most common bacterial sexually transmitted infection, with sexually
active young people at highest risk. As chlamydia often has no symptoms and can have
serious and costly health consequences (e.g. pelvic inflammatory disease, ectopic pregnancy
and tubal factor infertility) it is vital that it is picked up early and treated.
The National Chlamydia Screening Programme (NCSP) in England was established in 2003. It
offers free, opportunistic screening, treatment and partner management and prevention to
sexually active young men and women under the age of 25. Community based chlamydia
testing, treatment and partner notification services will support the development of sexual
health services in primary care and will help to achieve the population based chlamydia
screening at rates of the 35 - 50 percent coverage necessary to reduce prevalence.
8. Location of Provider Premises
The Provider’s Premises are located at:
[Insert address of Provider’s Premises if applicable]
10
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
SUMMARY OF SAFEGUARDING REQUIREMENTS FOR PHARMACISTS
DELIVERING SEXUAL HEALTH SERVICES TO CHILDREN AND
VULNERABLE ADULTS IN STAFFORDSHIRE
Everybody (including under 13s) has a right to confidential advice and treatment on sexual health.
EHC should be supplied if the client fully understands the medical treatment that is proposed (i.e. if a child is
under 16 they should be Gillick competent)
The client is:
Under 13
Under 13s cannot
give consent, so an
offence has been
committed.
First Response –
0800 13 13 126 or
the Police 999
13 - 15
16 -17
A vulnerable adult
Where the practitioner has concerns about a client’s welfare, a sexual health Risk
Assessment form should be completed and filled in the clients records or identified file.
Was the sexual activity
with someone over 16,
with somebody in a
position of trust or
otherwise thought to be
exploitative or abusive?
NB The age of consent
is 16 years, but the
legislation is not
intended to prosecute
consensual sex
between similar aged
young people.
Was the sexual
activity with
somebody in a
position of trust or
otherwise thought to
be exploitative or
abusive?
Yes
Was the sexual
activity with
somebody in a
position of trust or
otherwise thought to
be exploitative or
abusive?
Yes
Yes
The client must be informed of your concerns and of your duty to seek professional advice. (If this occurs out of
office hours you must consider offering the client a further appointment to feedback the professional advice
sought) This should be documented in the client’s records together with the agreed appointment date.
Discuss with safeguarding lead/senior manager of the pharmacy and contact:
First Response Team
Tel. 0800 1313 126
Staffordshire and Stoke-on-Trent Adult
Safeguarding Partnership
Emergency Duty Team (outside office hours) – 0845 6042886
Fax 01785 854223
e.mail firstr@staffordshire.gov.uk
OR THE POLICE ON 999
Tel. 0845 604 2719;
Fax 01785 276026.
email:
VAStaffordshire@staffordshire.gov.uk
N.B. If a decision is made not to refer following discussion with the safeguarding lead/senior manager at
the pharmacy, then the reasons must be fully documented.
11
[2014/15
PUBLIC HEALTH SERVICES CONTRACT]
[PLEASE DELETE THIS HEADER IN EACH FINALISED CONTRACT]
Emergency contraception/sexual heath advice in Community Pharmacies
Risk Assessment for children and vulnerable adults in Staffordshire
Service User’s name…………………………………………………………………………
Date of birth…………………………………………………………………………..
Date of assessment…………………………………………………………………
YES
NO
N/A
Is Service User under 13?
If under 16 – is the Service User Gillick Competent?
If under 16 – Are there any concerns that there is a
significant age difference between your Service User
and their partner (Please consider an age gap of 4
years plus a potential concern)
Are there any concerns that your Service User has
been forced to have sexual intercourse (this includes
rape)?
Are there any concerns that your Service User is
being sexually abused?
Are there any concerns that your Service User is in
an incestuous relationship?
Are there any concerns that the person may not have
the necessary mental capacity to make decisions
about sexual activity or is there any reason to believe
that they are being coerced?
Has there been any disclosure from your Service
User that leads you to be concerned?
If you answer YES to any of the above, please discuss your concern with your Service User and
inform them that you need to seek advice.
Following the above risk assessment – if concerns are identified obtain address and GP details
for any future follow up/referral to First Response Team (for Service Users aged under 18) or
Adult Safeguarding Partnership (Service Users aged 18 and above)
YES
NO
Have your concerns been discussed with your Service User?
Have you discussed your concerns with a member of the First
Response Team/Adult Safeguarding Partnership?
Has your discussion with the relevant safeguarding team led to
a referral?
If a decision is made not to refer following discussion with the safeguarding lead/senior
manager at the pharmacy, then the reasons must be fully documented.
12