PEM Board Review Series: Dental, Neck, and Thoracic Trauma
PEM Board Review Series:
Dental, Neck, and Thoracic Trauma
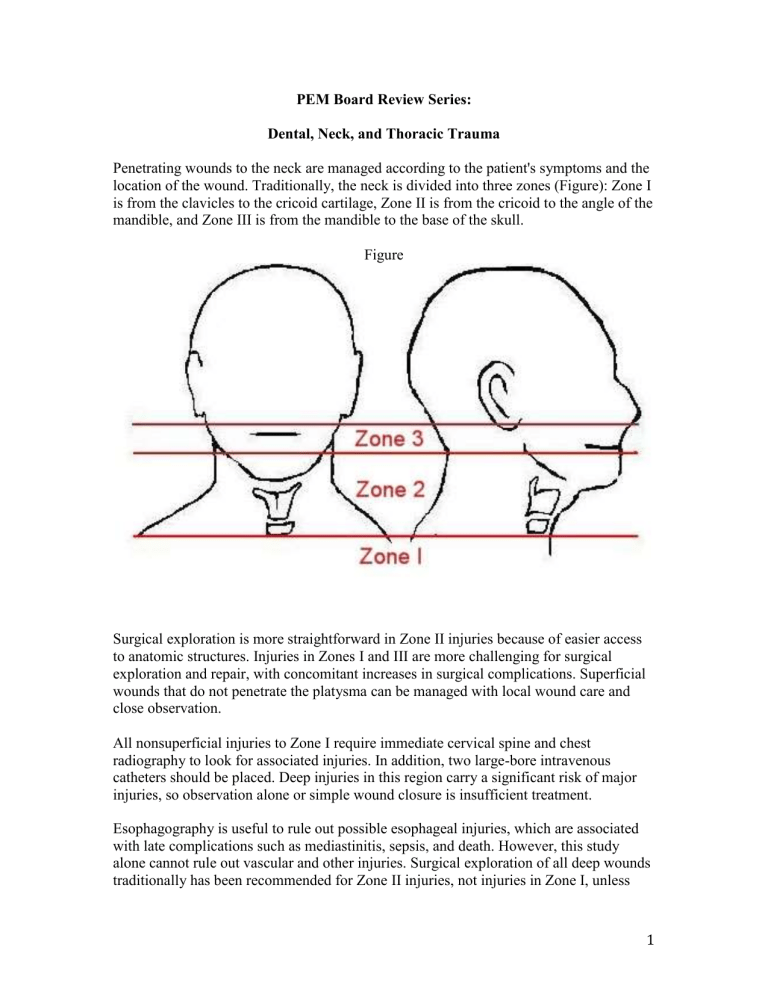
Penetrating wounds to the neck are managed according to the patient's symptoms and the location of the wound. Traditionally, the neck is divided into three zones (Figure): Zone I is from the clavicles to the cricoid cartilage, Zone II is from the cricoid to the angle of the mandible, and Zone III is from the mandible to the base of the skull.
Figure
Surgical exploration is more straightforward in Zone II injuries because of easier access to anatomic structures. Injuries in Zones I and III are more challenging for surgical exploration and repair, with concomitant increases in surgical complications. Superficial wounds that do not penetrate the platysma can be managed with local wound care and close observation.
All nonsuperficial injuries to Zone I require immediate cervical spine and chest radiography to look for associated injuries. In addition, two large-bore intravenous catheters should be placed. Deep injuries in this region carry a significant risk of major injuries, so observation alone or simple wound closure is insufficient treatment.
Esophagography is useful to rule out possible esophageal injuries, which are associated with late complications such as mediastinitis, sepsis, and death. However, this study alone cannot rule out vascular and other injuries. Surgical exploration of all deep wounds traditionally has been recommended for Zone II injuries, not injuries in Zone I, unless
1
there is a rapidly expanding lesion or shock. Recent literature suggests that even Zone II injuries may be amenable to careful evaluation with ancillary studies and selective exploration. Management of Zone III injuries is controversial; such injuries are handled on an individual basis.
Mortality from penetrating neck trauma is between 3% and 6%. Early mortality is related to airway compromise and hemorrhagic shock; most late mortality is related to undiagnosed esophageal injuries. Even low-velocity wounds are associated with major injuries in 50% of cases.
If it does penetrate the platysma muscle, the management depends on the zone:
Zone I: CT Angio, Esophagram, Bronch
Zone II: Surgical exploration if unstable—if stable, do CT Angio instead
Zone III: CT Angio, Esophagram, Bronch
Dental Trauma:
Permanent tooth avulsion:
A true dental emergency. Prognosis is best if dental re-implantation and splinting is instituted within 30-60 minutes. The ED physician may GENTLY rinse the tooth, and then reinsert it into the empty socket (in the cooperative child) prior to definitive care by a dentist. Otherwise, the tooth may be preserved in a medium such as Viaspan, Save-atooth, or whole milk.
Management of Dental Fractures:
Uncomplicated (Ellis Class 1, enamel alone: chip/ragged edge; no increased sensitivity; or Ellis Class 2, enamel + dentin: yellow exposed—sensitivity to touch, temp or air) dental fractures. These cases can be referred to the dentist within 48 hours for tooth insulation with calcium hydroxide or glass ionomer to protect against pulpal necrosis; children under 12 years are at higher risk of extension of infection into pulp since their dentin layer is thinner.
Complicated (Ellis Class 3, enamel, dentin, and pulp; sensitive to touch, fluid, temp, and air; exposed pulp may be bleeding or red in the middle) dental fractures: need to see a dentist immediately to institute pulpal therapy.
Extraction of a fractured tooth rarely is necessary and should be avoided. Outpatient follow-up with a dentist is appropriate after initial management, as described. Antiseptic mouthwash is not useful in this setting. Approximately 50% of children suffer dental injuries, 90% of which involve central or lateral incisors. Falls are the most common causes of dental trauma in preschool and school-age children; sports-related injuries are more common in adolescents. Early interventions can improve cosmetic results, prevent tooth loss, and decrease the risk of infection, so every attempt should be made to initiate care in the emergency department. Careful and comprehensive examination, including evaluation for injuries such as luxation, intrusion, and avulsion of teeth, should be performed. Intraoral dental radiographs and panoramic views should be obtained. Trauma to the teeth may be associated with injury to supporting structures
2
such as the alveolar bone and periodontium.
3
Dietary advice (soft diet), and outpatient follow-up with dentistry (within 24 to 48 hours) are recommended for all patients.
If it is unclear whether a tooth is primary or permanent, such age ranges, along with the appearance of the tooth (larger size, serrated crown in permanent teeth), can be used to make this determination. Primary (deciduous) teeth should not be reimplanted due to the potential for trauma to the developing permanent tooth bud. The most commonly avulsed teeth are the upper central incisors, followed by the upper lateral and lower central incisors.
The most important determinant of outcome after permanent tooth avulsion is extraoral
“dry” time, with the best prognosis associated with immediate reimplantation. When such implantation is not feasible, storage and transport in appropriate liquid media improves the likelihood of successful reimplantation. Appropriate storage/transport media (in order of preference) include ViaSpan™ (organ preservation solution) (DuPont Pharma) or
Hank's balanced salt solution (cell culture media), cold milk, saliva, or saline. Water can be used but is less desirable because of associated cell lysis and resultant inflammation.
The use of appropriate liquid media can extend the time of cell viability from less than 1 hour (dry) to several hours (milk or saliva) and up to 1 day or more (ViaSpan™ or Hank's balanced salt solution).
Scrubbing or damage to the root surface should be avoided because remaining periodontal ligament fibers are the key to healing after reimplantation. The tooth should be handled only by the crown to avoid trauma to the root. If there is a large clot or debris within the alveolar socket, gentle irrigation or probing can be used to clear the socket.
Once the tooth is reimplanted, it can be held in place with a gauze pad or tongue blade until formal splinting can be accomplished. Dental radiographs should be obtained to assess for any alveolar fractures. Tetanus prophylaxis should be administered if appropriate, and prophylactic antibiotic therapy should be considered. Patients should be instructed to eat a soft diet for 2 weeks.
Published contraindications to reimplantation include damage to the tooth root (fracture), damage or deformity of the alveolar bone, underlying immune defect or complex heart disease, uncontrolled seizure disorder, or an uncooperative patient. Prolonged “dry time”
4
(>60 min) makes successful reimplantation and long-term viability of the tooth unlikely.
Teeth probably should be reimplanted in the emergency department while awaiting dental consultation. Complications after reimplantation of a permanent tooth include abscess formation, tooth discoloration, root resorption, and ankylosis.
Thoracic Trauma:
Most chest injuries in younger children are caused by blunt chest trauma in contrast to the more common penetrating chest trauma seen in adolescents. Pneumothorax from blunt chest trauma can be a result of rib fractures penetrating the pleura or alveolar rupture from sudden compression of the thorax. tension pneumothorax: absent breath sounds on the affected side, respiratory distress, chest pain, tachycardia, and hemodynamic compromise. Other findings suggesting tension pneumothorax include: asymmetry in chest excursion, hyperresonance of the ipsilateral hemithorax, tracheal deviation away from the affected side, and jugular venous distention. Similar symptoms also might be seen with a massive hemothorax, although there would be dullness to percussion on the ipsilateral side.
Simple traumatic pneumothoraces are managed either with close observation in the hospital or a pleural drainage device. The pleural drainage device should be placed in patients who are managed with positive pressure ventilation or prior to medical air transport because of their potential for conversion into a tension pneumothorax.
Endotracheal intubation should be considered in the trauma patient who has apnea, loss of protective airway reflexes, or significant head injury. Needle cricothyrotomy might be considered for the patient who has severe neck or facial trauma and cannot be ventilated or oxygenated, for whom bag-valve-mask ventilation is ineffective, and for whom previous attempts at tracheal intubation have failed.
Pericardiocentesis is indicated in a patient who has suspected cardiac tamponade. Cardiac tamponade is not very common in the pediatric patient who has blunt chest trauma.
However, the diagnosis should be considered in the presence of distant/muffled heart sounds, hemodynamic instability (hypotension with narrowed pulse pressure), and distended neck veins. Ultrasonography, if available, allows a rapid and much more accurate confirmation of cardiac tamponade.
Some pediatric case series report high rates of extraction for dental abscesses in the acute setting, but this is not the standard of care at many pediatric centers. The initial treatment of choice in the pediatric emergency department is oral antibiotic therapy to address the underlying pathogen. Organisms that predominate in dental abscesses are gram-positive cocci, such as alpha-hemolytic streptococcal species; Peptostreptococcus sp; and anaerobic gram-negative rods such as Prevotella, Porphyromonas , and Fusobacterium sp. Penicillin or amoxicillin are the antibiotics of choice, with many practitioners choosing amoxicillin for its greater palatability in liquid form and less frequent dosing.
For those who are allergic to penicillin, clindamycin is the treatment of choice. Follow-up
5
with a dentist as soon as possible to confirm the infection with a periapical radiograph is recommended.
Incision and drainage is not recommended routinely for pediatric patients because it is more invasive and poorly tolerated by young children; acute infection frequently clears with antibiotics alone. Extraction of the necrotic tooth is recommended after the acute infection is under control and usually can be accomplished with local anesthesia in a school-age child. Acute infection impairs the absorption of local anesthetic, making anesthetizing the tooth more difficult in the acute setting.
Thoracic Trauma:
The child described in the vignette most likely has a thoracic injury. Severe blunt chest trauma is a rare but often deadly injury in pediatric patients. Thoracic injuries are the second leading cause of death from trauma in pediatrics (after head injury) and often are associated with multisystem injuries. Because children have compliant chest walls and less body fat, significant transmission of kinetic energy from the point of impact to the intrathoracic structures may occur. Thus, there may be few external signs of trauma despite an underlying major intrathoracic injury. The acute decompensation described for the child in the vignette mandates rapid diagnosis. There is no evidence of a tension pneumothorax in this boy. A portable chest radiograph can help to rule out several lifethreatening thoracic injuries: tension pneumothorax, large hemothorax, and pericardial effusion. Other injuries, such as tracheal rupture and aortic dissection, also may be suggested by findings on the chest radiograph.
Cardiac injuries resulting from blunt chest trauma are rare in children. They include cardiac contusion, atrial and ventricular rupture, and great vessel injuries. The signs and symptoms of cardiac injuries are nonspecific and overlap with those resulting from injuries to the respiratory apparatus. They include hypotension, tachycardia, jugular venous distention, and muffled heart sounds. Occasionally, blunt cardiac injuries can lead to potentially fatal ventricular arrhythmias. In particular, commotio cordis, a sudden disruption of normal heart rhythm after a blow to the chest (eg, from a baseball or hockey puck) can cause ventricular tachycardia or fibrillation, leading to sudden cardiac arrest.
Computed tomography scan of the head and neck should be performed only after acute cardiopulmonary decompensation has been addressed. A complete blood count frequently is used in diagnosing acute hemorrhage. However, the value of this test in the emergency setting is questionable because sufficient blood loss to cause a decrease in hematocrit may not occur rapidly. Electrocardiography may be useful in diagnosing pericardial effusion. Characteristic findings include sinus tachycardia and ST segment elevations. If there is strong clinical suspicion for pericardial effusion, bedside echocardiography is the diagnostic test of choice.
6
Hemothorax: (following a GSW to left chest)
The most appropriate next step is tube thoracostomy to drain the blood from the pleural space that is producing cardiorespiratory compromise. A chest tube also allows determination of the total volume of blood lost in the thorax and the rate of potential ongoing hemorrhage, which, in turn, helps to define the need for an operative intervention with open thoracotomy. Other indications for tube thoracostomy include: a large, enlarging, or symptomatic pneumothorax; tension pneumothorax; chylothorax; significant pleural effusion; or empyema. The relative contraindications for tube thoracostomy are a bleeding diathesis or skin/soft-tissue infection in the overlying area intended for tube placement. However, these conditions do not preclude performing the procedure in a life-threatening situation.
The procedure for tube thoracostomy is as follows:
Position the patient supine (in nontraumatic situations, recumbent or upright positioning is an alternative), with the ipsilateral arm placed above the patient’s head and the area prepped and draped in a sterile fashion.
Locate the insertion site in the mid to anterior axillary line in the fifth or sixth intercostal space. The nipple is used commonly as an anatomic landmark to help identify the appropriate intercostal space.
If the clinical situation permits, use local anesthesia prior to making the overlying skin incision.
7
Use a curved hemostat for blunt dissection of the intercostal muscles and subcutaneous tissue over the rib to avoid damaging the neurovascular bundle.
Use the tip of the hemostat to puncture the parietal pleura.
Use a finger to explore the subcutaneous track carefully and to exclude adhesions between the lung and the chest wall.
Use the largest chest tube that can be accommodated between the ribs for fluid drainage. The chest tube is directed through the track anteriorly and superiorly for a pneumothorax and posteriorly for drainage of blood or other fluids.
Needle decompression could be useful if there is an associated pneumothorax, but it usually does not improve a large hemothorax. No absolute contraindications to needle decompression of the chest exist, other than performing it in a situation that does not warrant it originally, thus potentially causing an iatrogenic pneumothorax. The primary indication for needle decompression of the chest is to treat a suspected tension pneumothorax, especially when tube thoracostomy cannot be performed expeditiously.
The key steps required to perform needle decompression are to:
Use a large-bore 16- or 18-gauge needle/catheter, with a smaller-gauge needle for neonates.
Locate the insertion site in the anterior midclavicular line, usually in the second or third intercostal space, advancing over the underlying rib to avoid the neurovascular bundle that runs inferior to the rib.
Aspirate air into the syringe as the thoracic cavity is entered and the pressure is released. A three-way stopcock attached to the syringe allows continued, periodic evacuation of air from a reaccumulated tension pneumothorax until tube thoracostomy can be performed.
Endotracheal tube exchange to a cuffed tube might be necessary in a more stable patient who demonstrates a significant air leak or if a need for higher peak airway pressures is anticipated. A tracheostomy might be appropriate for the patient who experienced significant facial or upper airway trauma and requires an emergent surgical airway because of difficulty with obtaining an oropharyngeal airway.
Injuries to the hard palate are managed with supportive care; injuries to the lateral soft palate require CT angio to rule out damage to major vessels.
Frenulum lacs do not require suturing unless bleeding cannot be controlled by direct pressure.
Most midline superficial tongue lacs heal without suturing; Indications for suturing include lacs that are “thru and thru”, those where hemostasis cannot be obtained; and deep lacs on the margins of the tongue. Injuries to the margins can result in “flap” or
“forked” appearance and possibly interfere with phonation.
8
The most common facial bone fractures in children are those involving the nasal bones, followed by those of the mandible. The most common mandible fracture location is at the neck of the condyles, followed by the mandibular angle. Inability to fully open the mouth is a common presentation of those with mandibular fractures. Patients with unilateral mandible condyle fractures will present with the mandible deviated toward the affected side when the child opens the mouth. If 2 fractures of the mandible are present, the child will need stabilization either by open or closed techniques.
Unilateral or bilateral mandible dislocations can occur following an extreme opening of the mouth (i.e. a deep yawn or a prolonged dental treatment session.) Initial treatment consists of reassuring the patient and gently massaging the mastication muscles. If this treatment fails, the patient should be given a sedative for relaxation, the mastication muscles massaged, and then gentle downward and backward pressure should be applied by the physician’s thumb (wrapped in gauze) on the occlusal surfaces of the posterior teeth.
A pulmonary contusion is the most common thoracic injury in children who sustain major blunt trauma. In 50% of these children there is the absence of tachypnea, abnormal breath sounds, external thoracic wall contusions, and/or fractures of the bony thorax. In addition, pulmonary contusions may not be visible on the initial chest x-ray; chest CT is more sensitive. In children with minimal or no symptoms, admission for close observation and supportive care is recommended. Because of the elasticity and flexibility of the thoracic cage in children, chest wall injuries are often associated with internal organ injury.
A pulmonary lac (i.e. from a stab to the chest) often causes tachypnia and decreased breath sounds. Large lacs may cause hemoptysis or hemothorax. Treatment includes adequate IV access and blood for transfusion if there is evidence of hemodynamic compromise. A thoracostomy tube should be inserted (NOT at the site of the lac—rather, an occlusive dressing should be applied over the lac after the chest tube insertion.) ET intubation should be reserved for patients with respiratory distress, with significant hemoptysis, and/or who require ventilatory support despite chest tube insertion.
If a patient has an open pneumothorax, initial treatment includes placement of an occlusive dressing at the wound site. This is best done when the patient is in full expiration. A chest tube should be placed immediately (NOT through the wound) to prevent development of a tension pneumothorax. Patients with persistent respiratory distress despite application of an occlusive dressing and thoracostomy tube, should be intubated and receive positive pressure ventilation.
In a chest/neck injury with the presence of a pneumomediastinum, along with the absence of a pneumothorax, tracheal rupture should be suspected. CT of the chest and neck can confirm the diagnosis and identify other injuries. Treatment is airway stabilization by bronchoscopy in the OR (do NOT intubate in the ED unless absolutely required due to respiratory failure as orotracheal intubation can extend a partial tracheal tear.)
9
In patients with evidence of esophageal perforation—may be spitting up some blood
(from gsw or knife injury) the airway should be secured by ET intubation. A CXR may show a pneumothorax, pneumomediastinum and/or air/fluid level in the mediastinum.
The patient should be started on IVF and broad-specturm antibiotics covering Grampositive, gram-negative, and anerobic organisms given. The diagnosis can be made by esophagography or esophagoscopy. Then surgical repair is required. Diagnoses made within 24 hours have a 5% mortality whereas delayed diagnoses are associated with a
70% mortality.
A diaphragmatic rupture is demonstrated by a scaphoid shaped abdomen, and requires surgical repair in the OR. The rupture usually occurs on the same side as the impact.
80% of these occur on the left since it is relatively unprotected compared to the right
(protected more by the liver). Associated injuries, including pulmonary contusions, hepatic and splenic lacs, and fractures, are present in more than 75% of these patients.
The initial CXR is normal in 50% of patients so serial chest radiographs are required.
Chest and abdominal CT’s with contrast can help confirm the diagnosis.
Traumatic rupture of the thoracic aorta carries a 95% mortality rate in children. Clinical signs may include differences in pulses between upper and lower extremities, thoracic ecchymoses, thoracic and back contusions, paraplegia and anuria. 90% will have abnormal CXR; classic findings include a widened mediastinum, loss of the aortic knob, left-sided pleural cap, tracheal deviation, and NG tube deviation. The gold standard of diagnosis is aortography.
In patients suffering from blunt cardiac injury as evidenced by a new cardiac murmur following trauma, a TE Echo should be performed since it is more sensitive than transthoracic echo in detecting myocardial injuries.
Do surgery after massive hemothorax if initial chest tube output is 25% of circulating blood volume (or 25cc/kg) or the ongoing output is 2.5% of circulating blood volume per hour (or 2.5cc/kg/hr).
The nature of the injury suffered by the boy described in the vignette and his sudden cardiopulmonary arrest in the emergency department make him a suitable candidate for an emergency thoracotomy. The situation does not allow time for transport to the operating theater; the procedure should be performed in the emergency department. The few pediatric studies that have examined the use of emergency thoracotomy appear to agree with recommendations based on adult literature that this is an arguably heroic, lifesaving measure of limited utility for selected patients. Outcomes appear to be better for patients who have sustained nonballistic, single penetrating injuries compared with blunt trauma. Ultimately, the purpose of emergency thoracotomy is to provide temporary stabilization of a patient's injuries for subsequent definitive repair in the operating theater. The particular patient situations for which emergency thoracotomy is indicated are:
Sudden cardiopulmonary arrest just prior to arrival or while in the emergency department in a patient who has suffered penetrating injury to the chest
10
Sudden cardiopulmonary arrest in the emergency department after blunt trauma cardiopulmonary arrest in the field after blunt trauma is not an indication for thoracotomy because the outcome is uniformly poor
Persistent severe hypotension or shock with suspected intrathoracic hemorrhage or pericardial tamponade
The pathophysiologic objectives of emergent thoracotomy are to:
Alleviate massive pericardial tamponade, especially if there is clotted blood in the pericardium that cannot be drained by pericardiocentesis
Control thoracic vascular or cardiac hemorrhage directly
Improve temporary shunting of blood preferentially to the brain and heart by allowing open cardiac massage and cross-clamping of the thoracic aorta
Reduce further hemorrhage below the diaphragm from intra-abdominal compartment trauma by cross-clamping the thoracic aorta
The procedural technique is as follows:
Place the patient supine, with the side to be operated on slightly elevated.
After sterile preparation of the entire chest wall, make an opening in the left fifth intercostal space anterolaterally, starting from the sternum, avoiding the pectoralis major muscle and breast tissue in females, and following the line of the rib up to the axilla.
The left side is incised more commonly because it allows more immediate exposure of the pericardium and affords easier access if open cardiac massage is necessary. Incision of the intercostal muscles and parietal pleura should occur across the superior margin of the rib to avoid the neurovascular bundle. The left-sided approach can be extended, if necessary, to include the right side, sawing through the sternum in the so-called
“clamshell” thoracotomy. Most investigators agree that emergency thoracotomy is not appropriate for patients who have no signs of life in the field and upon arrival to the emergency department after suffering either penetrating or blunt trauma to the chest.
Potential problems associated with emergency thoracotomy include:
Injuries to underlying thoracic structures, such as breast tissue, heart, and lung
Injuries to intercostal, coronary, and thoracic blood vessels
Complications in survivors, such as bleeding and infections of the pericardium, pleural spaces, sternum, and chest wall; arrhythmias; and postpericardiotomy syndrome
Exposure of the health-care worker to the patient's blood
External pacing is indicated for symptomatic bradycardia, sinus or atrioventricular node dysfunction, or to overdrive a tachydysrhythmia not responding to medications or conventional measures. Intraosseous and femoral central venous catheters are unnecessary in this patient because he already has two large-bore intravenous catheters established. Rapid infusion of blood may be indicated for patients who have penetrating trauma wounds and shock, but it is not appropriate to wait for type-specific blood.
11
GSW to Abdomen/Chest:
The presence of a suspected entrance wound in the abdomen with respiratory and cardiovascular signs suggests a multisystem and multicompartment injury, including a likely pneumothorax. In addition to managing the patient’s airway, tube thoracostomy is most likely to be performed immediately upon arrival in the emergency department.
Emergency thoracotomy is only indicated in the patient in just recent full cardiac arrest who has a penetrating injury.
Any child who has a penetrating abdominal injury, especially from a projectile such as a bullet, should be suspected of having injuries beyond the obvious site of injury. A bullet can traverse many different areas and organ systems and be redirected by organs, bones, and vessels. Evaluation should start, as always, with the airway, breathing, and circulation, looking for any signs of compromise. This child has tachypnea, tachycardia, and hypotension, suggestive of pulmonary involvement and blood loss. Tachypnea and tachycardia can present with other causes, but in this situation, intrathoracic and intraabdominal injuries are most likely, and administration of 100% oxygen, intravenous line placement, and fluid resuscitation are indicated. Laboratory evaluation and blood typing and cross-matching are required because the boy may need immediate transfusion if he experiences further cardiovascular deterioration. Radiologic studies, if the patient is stable, can help work through the possibilities. Portable chest and abdominal radiographs, focused assessment with sonography for trauma (FAST) examination, and bedside echocardiography can be useful adjuncts in rapid screening.
Not all patients who have penetrating abdominal trauma require operative intervention.
Isolated stab wounds to the abdomen can be considered for nonoperative management as long as the patient is in a center with skilled assessors who can perform serial examinations and provide rapid, on-site surgical intervention if the need arises. Even patients who have gunshot wounds to the abdomen may be considered for nonoperative management in some centers if radiographic evaluations (computed tomography [CT] scan) demonstrate no violation of the peritoneum. Of note, the track of a bullet is well seen on CT scan, but that of a stab wound is more difficult to determine. If an isolated solid viscus injury is identified, nonoperative observation may be considered at the discretion of the surgical team. There are also reports of selective nonoperative management of omental evisceration after penetrating trauma. However, if any of these injuries is associated with hemodynamic instability, evidence of hollow viscus injury (eg, peritonitis, diffuse abdominal tenderness), or associated free fluid, operative intervention is indicated. Additionally, patients who have head injuries or need for other surgical interventions may not be good candidates for nonoperative management.
All patients who have penetrating injuries to the upper abdomen should be evaluated for thoracic trauma. Tension pneumothorax, hemothorax, pulmonary contusion, pulmonary laceration, diaphragmatic injury, tracheal or esophageal injury, cardiac tamponade, neurologic injury, and other cardiac and large/small vascular compromise can be seen in patients who have this presentation.
12