Basic asthma action plan
advertisement

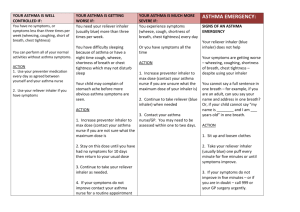
Personalised Asthma Action Plan This document has been developed as part of the National Paediatric Asthma Collaborative, by a collaborative of organisations: **Please note, this document is not NHS England mandated, but is designed to be a useful resource that local clinicians and commissioners can adapt and implement locally. Please therefore add your own branding and logos, as appropriate. The content is what the National Paediatric Asthma Collaborative consider to be the minimum standard for a personalised asthma action plan, hence its’ basic format.** Page 1 of 5 National Paediatric Asthma Collaborative Personalised Asthma Action Plan Patient name: Date of birth: Next of kin / parents: Contact numbers: The information in this plan can help you maintain good health, and stay out of hospital. It also give you guidance and instruction as what to do if your asthma becomes a problem, and the medication you need to take regular, which may need to be increased, or decreased or up stay the same. Usual doctor: Asthma nurse: Contact numbers: Contact numbers: Email: Email: I have a peak flow meter: Yes My best peak flow (in the last year) is: 85% of my best is: 75% of my best is: 50% of my best is: My Asthma triggers are: My Drug allergies are: Date of last Review / Update: Date of next Review / Update: Date of Next Annual Review: Page 2 of 5 National Paediatric Asthma Collaborative Personalised Asthma Action Plan My asthma is well controlled when: • There are no regular daytime symptoms (cough, wheeze, chest tightness, shortness of breath). • There are no night time symptoms. • Asthma does not interfere with my usual activities (eg work, study, housework). • The peak flow is above 85% of personal best. 85% of my best peak flow is: My usual treatment is: My reliever medications (taken when needed to relieve symptoms) are: Name Inhaler or Medicine Colour Dose (When I need to re order this medicine it is called…………………………………………………) My first preventer medication is (taken regularly even when you have no asthma symptoms): Name Inhaler or Medicine Colour Used with a Spacer Y/N Dose (When I need to re order this medicine it is called……………………………………………………………) My second preventer medication is (taken regularly even when you have no asthma symptoms): Name Inhaler or Medicine Colour Used with a Spacer Y/N Dose (When I need to re order this medicine it is called……………………………………………………………) My third preventer medication is (taken regularly even when you have no asthma symptoms): Name Inhaler or Medicine Colour Used with a Spacer Y/N Dose (When I need to re order this medicine it is called……………………………………………………………) Page 3 of 5 National Paediatric Asthma Collaborative Personalised Asthma Action Plan My asthma is getting worse when: Moderate symptoms: • Take the reliever puffer (Colour……………) every 2-4 hours or more often. • I am having constant wheezing, coughing, chest tightness. • I am having difficulty with normal activity. • My peak flow is between 50 to 75% of personal best peak flow 50% is 75% is What should I do? • Acute treatment • Monitor response • When symptoms have returned to being well controlled, switch back to your usual treatment after 4 days. My asthma is an emergency if: • My am having great difficulty breathing. • Difficulty speaking or walking due to severe shortness of breath. • The reliever puffer is giving little or no improvement when taken every hour or more often. • Symptoms are getting worse quickly. • Peak flow is less than (50% of personal best). 50% is Action: • Take the reliever puffer (Blue) How much…………………………… How often…………………………… • If there is no immediate improvement, contact a doctor urgently and, if one is not available, call 999 for an ambulance. Emergency treatment Whilst waiting for doctor/ambulance: Take……………………………………. Page 4 of 5 National Paediatric Asthma Collaborative Personalised Asthma Action Plan Updating my action plan: • I should see my nurse/doctor for a regular asthma review at least once a year. My next one is due: • If your medication has been increased, see the nurse or doctor after a month to review progress. The date for this review is: • If your symptoms have been very well controlled over at least 3 months, arrange a review as it may be possible to step down your treatment. Page 5 of 5 National Paediatric Asthma Collaborative