There are many ways to manage diabetes type 1, and while
advertisement
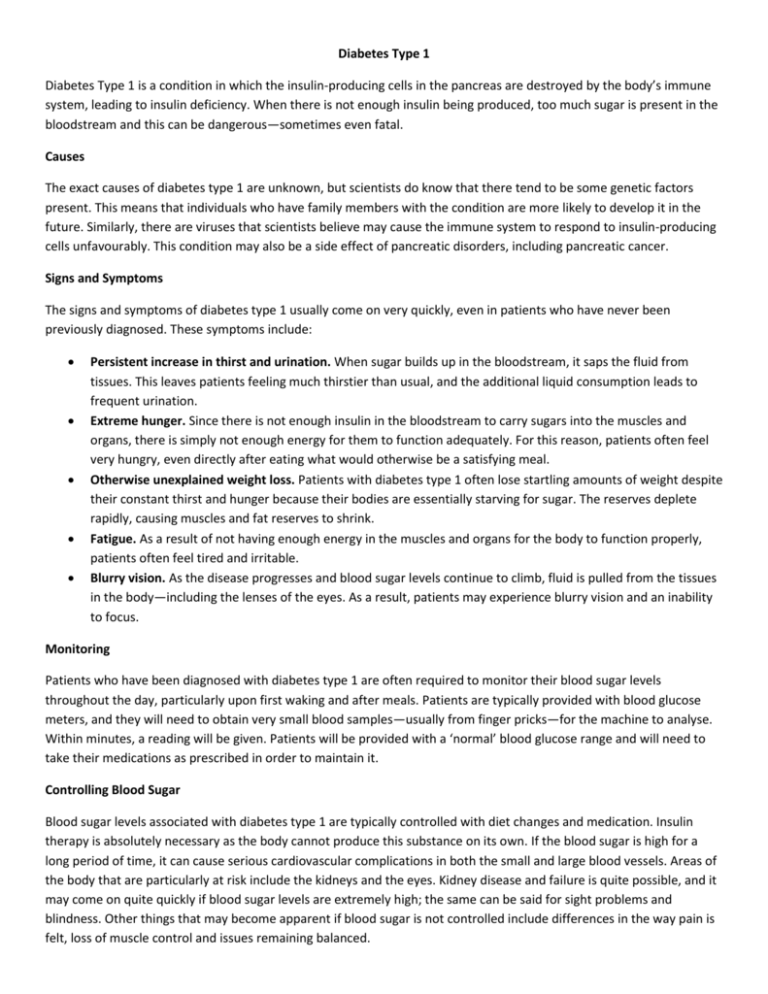
Diabetes Type 1 Diabetes Type 1 is a condition in which the insulin-producing cells in the pancreas are destroyed by the body’s immune system, leading to insulin deficiency. When there is not enough insulin being produced, too much sugar is present in the bloodstream and this can be dangerous—sometimes even fatal. Causes The exact causes of diabetes type 1 are unknown, but scientists do know that there tend to be some genetic factors present. This means that individuals who have family members with the condition are more likely to develop it in the future. Similarly, there are viruses that scientists believe may cause the immune system to respond to insulin-producing cells unfavourably. This condition may also be a side effect of pancreatic disorders, including pancreatic cancer. Signs and Symptoms The signs and symptoms of diabetes type 1 usually come on very quickly, even in patients who have never been previously diagnosed. These symptoms include: Persistent increase in thirst and urination. When sugar builds up in the bloodstream, it saps the fluid from tissues. This leaves patients feeling much thirstier than usual, and the additional liquid consumption leads to frequent urination. Extreme hunger. Since there is not enough insulin in the bloodstream to carry sugars into the muscles and organs, there is simply not enough energy for them to function adequately. For this reason, patients often feel very hungry, even directly after eating what would otherwise be a satisfying meal. Otherwise unexplained weight loss. Patients with diabetes type 1 often lose startling amounts of weight despite their constant thirst and hunger because their bodies are essentially starving for sugar. The reserves deplete rapidly, causing muscles and fat reserves to shrink. Fatigue. As a result of not having enough energy in the muscles and organs for the body to function properly, patients often feel tired and irritable. Blurry vision. As the disease progresses and blood sugar levels continue to climb, fluid is pulled from the tissues in the body—including the lenses of the eyes. As a result, patients may experience blurry vision and an inability to focus. Monitoring Patients who have been diagnosed with diabetes type 1 are often required to monitor their blood sugar levels throughout the day, particularly upon first waking and after meals. Patients are typically provided with blood glucose meters, and they will need to obtain very small blood samples—usually from finger pricks—for the machine to analyse. Within minutes, a reading will be given. Patients will be provided with a ‘normal’ blood glucose range and will need to take their medications as prescribed in order to maintain it. Controlling Blood Sugar Blood sugar levels associated with diabetes type 1 are typically controlled with diet changes and medication. Insulin therapy is absolutely necessary as the body cannot produce this substance on its own. If the blood sugar is high for a long period of time, it can cause serious cardiovascular complications in both the small and large blood vessels. Areas of the body that are particularly at risk include the kidneys and the eyes. Kidney disease and failure is quite possible, and it may come on quite quickly if blood sugar levels are extremely high; the same can be said for sight problems and blindness. Other things that may become apparent if blood sugar is not controlled include differences in the way pain is felt, loss of muscle control and issues remaining balanced. Benefits of Exercise Since maintaining proper blood sugar levels is more difficult for people with diabetes type 1, they should exhaust all measures—including lifestyle changes—to do so. Exercising can help people with this form of diabetes by: Improving how injected insulin works within the body Decreasing the amount of insulin that must be injected Reducing cardiovascular risk factors and increasing health and fitness Decreasing the risk of diabetes-related complications Reduces symptoms of depression Improves overall quality of life While it is true that no amount of exercise can reverse the pancreatic damage that is responsible for diabetes type 1, it can improve and positively influence the way the muscles respond to the insulin that the patient injects. This in turn helps the glucose levels remain steady for hours after the exercise is completed. Best Types of Exercise Individuals suffering from diabetes type 1 can engage in the same activities as the general population provided they do not have any diabetes complications that prevent them from doing so. Resistance and aerobic exercise is both safe and recommended for diabetics. Aerobic exercise should be performed at medium to high intensity for 20 to 60 minutes per day on most days of the week in order to provide the maximum benefits. Resistance training such as weightlifting should be performed two or three days per week, and major muscle groups should be worked with eight to 10 different exercises in repetitions of eight to twelve, with each set being performed two or three times. There are many ways to manage diabetes type 1, and while exercise can never replace insulin as a lifesaving therapy, it can greatly enhance the way the insulin works within the body. Exercise can also improve patients’ overall quality of life by decreasing diabetes symptoms and reducing the risk for complications. Modes Diabetes: Exercise Programming Goals Intensity/Frequency / Duration ↑ aerobic capacity 50 – 90% peak HR* ↑ time to exhaustion 50 – 85% VO2 peak* ↑ work capacity Monitor RPE ** Improve BP response to exercise 4 – 7 days / wk ↓ cardiovascular risk factors 20 – 60min / session Aerobic Large muscle activities Strength Free weights Weight machines Isokinetic machines Anaerobic High intensity intervals Flexibility Stretching / Yoga Neuromuscular Yoga ↑ maximal number of reps Improve performance for patients interested in competition Only for athletes in good condition Maintain / ↑ ROM Improve gait Improve balance Improve coordination Time to Goal 4–6 months ↓ resistance, ↑ repetitions for most clients High resistance OK for athletes with well-controlled diabetes Same as healthy athletes 4–6 months Limited data available; 2 – 3 sessions / wk may suffice Limited data available; 2 – 3 sessions / wk may suffice 4–6 months ↑ ADLs Individualized to each other. ↑ vocational potential Increase physical self confidence (Source: ACSM’s Exercise Management for Persons with Chronic Disease and Disabilities; 2nd Edition) Functional Activity specific exercise