Nursing Care Plan for Dislocated or Fractured Jaw. Dislocation and
advertisement
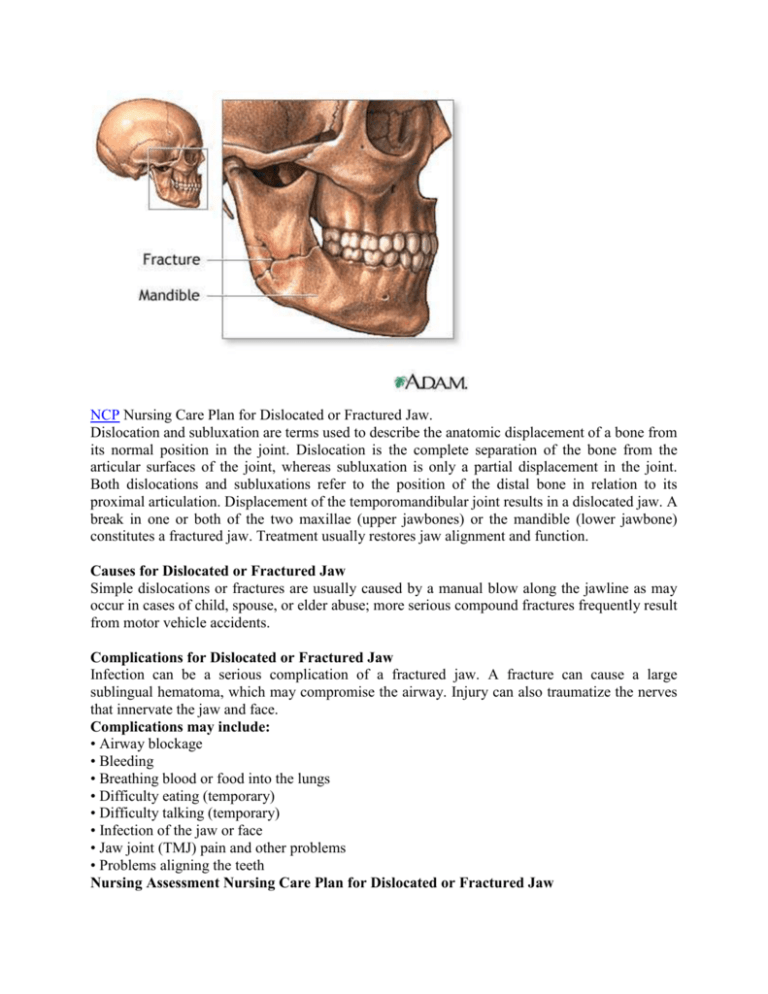
NCP Nursing Care Plan for Dislocated or Fractured Jaw. Dislocation and subluxation are terms used to describe the anatomic displacement of a bone from its normal position in the joint. Dislocation is the complete separation of the bone from the articular surfaces of the joint, whereas subluxation is only a partial displacement in the joint. Both dislocations and subluxations refer to the position of the distal bone in relation to its proximal articulation. Displacement of the temporomandibular joint results in a dislocated jaw. A break in one or both of the two maxillae (upper jawbones) or the mandible (lower jawbone) constitutes a fractured jaw. Treatment usually restores jaw alignment and function. Causes for Dislocated or Fractured Jaw Simple dislocations or fractures are usually caused by a manual blow along the jawline as may occur in cases of child, spouse, or elder abuse; more serious compound fractures frequently result from motor vehicle accidents. Complications for Dislocated or Fractured Jaw Infection can be a serious complication of a fractured jaw. A fracture can cause a large sublingual hematoma, which may compromise the airway. Injury can also traumatize the nerves that innervate the jaw and face. Complications may include: • Airway blockage • Bleeding • Breathing blood or food into the lungs • Difficulty eating (temporary) • Difficulty talking (temporary) • Infection of the jaw or face • Jaw joint (TMJ) pain and other problems • Problems aligning the teeth Nursing Assessment Nursing Care Plan for Dislocated or Fractured Jaw Patient's history reveals an injury to the jaw, and he reports mandibular pain beginning right after the injury. Patient may report Bite that feels "off" or crooked, Difficulty speaking, Drooling because of inability to close the mouth, Inability to close the mouth, Jaw that may protrude forward, Pain in the face or jaw, located in front of the ear on the affected side, and gets worse with movement, Teeth that aren't normally aligned Inspection reveals malocclusion (the most obvious sign of dislocation or fracture), swelling, ecchymosed, loss of function, and asymmetry. Palpation of the injured area reveals pain and swelling. During palpation, note whether the patient experiences any altered sensation. A mandibular fracture that damages the alveolar nerve produces paresthesia or anesthesia of the chin and lower lip. Diagnostic tests For Dislocated or Fractured Jaw X-rays usually most accurate confirm the diagnosis Nursing diagnosis Nursing Care Plan for Dislocated or Fractured Jaw Acute pain Ineffective airway clearance Anxiety Disturbed body image Imbalanced nutrition: Less than body requirements Impaired verbal communication Risk for aspiration Risk for deficient fluid volume Risk for infection Nursing Key outcomes Nursing Care Plan for Dislocated or Fractured Jaw Nursing outcomes Nursing Care Plan for Dislocated or Fractured Jaw, Patient will: Express feelings of comfort and relief of pain. Demonstrate methods (coughing, suctioning) to maintain a patent airway. Express that he feels less anxious. Express positive feelings about self. Have no further weight loss. Use an alternative method of communication if unable to communicate with language. Avoid aspiration. Fluid volume will remain adequate. Exhibit no signs or symptoms of infection. Nursing interventions Nursing Care Plan for Dislocated or Fractured Jaw Pain Management, Analgesic Administration, and Environmental Management Comfort: Alleviation of pain or a reduction in pain to a level of comfort that is acceptable to the patient. Use of pharmacologic agents to reduce or eliminate pain. Manipulation of the patient’s surroundings for promotion of optimal comfort Respiratory Monitoring, Airway Management: Facilitation of patency of air passages. Collection and analysis of patient data to ensure airway patency and adequate gas exchange Anxiety Reduction: Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source or anticipated danger. Calming Technique: Reducing anxiety in patient experiencing acute distress Body Image Enhancement: Improving a patient’s conscious and unconscious perceptions and attitudes toward patient body. Self-Esteem Enhancement: Assisting a patient to increase patient personal judgment of self-worth Nutrition Management Assisting with or providing a balanced dietary intake of foods and fluids. Weight Gain Assistance Facilitating gain of body weight. Eating impairment Management Communication Enhancement: Speech Deficit: Assistance in accepting and learning alternative methods for living with impaired speech. Active Listening Attending closely to and attaching significance to a patient’s verbal and nonverbal messages Aspiration Precautions Prevention or minimization of risk factors in the patient at risk for aspiration Fluid Monitoring, Hemodynamic Regulation, Bleeding Precautions: Collection and analysis of patient data to regulate fluid balance, Optimization of heart rate, preload, afterload, and contractility, Reduction of stimuli that may indicate bleeding or hemorrhage in at-risk patients Infection Protection, Infection Control, infection Surveillance: Prevention and early detection of infection in a patient at risk. Minimizing the acquisition and transmission of infectious agents Purposeful and ongoing acquisition, interpretation, and synthesis of patient data for clinical decision making