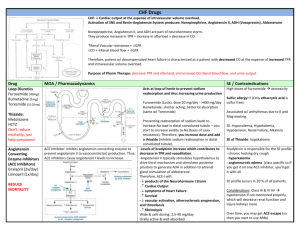
clinical pharmacology of drugs used in treatment of internal disseases
advertisement

Ministry of Education and Science of Ukraine Ministry of Public Health of Ukraine Sumy State University Medical Institute 3924 METHODICAL INSTRUCTIONS for practical work on the topic “Clinical Pharmacology of Drugs Used in the Treatment of Internal Diseases” (аccording to the Bologna Process) for the students of speciality 7.110101 “Medical Care” of the full-time course of study Sumy Sumy State University 2015 Methodical instructions for practical work on the topic “Clinical Pharmacology of Drugs Used in the Treatment of Internal Diseases” / compiler A. A. Roschupkin. – Sumy : Sumy State University, 2015. – 134 p. The Department of Biophysics, Biochemistry, Pharmacology, and Biomolecular Engineering 1. GENERAL PRINCIPLES PHARMACOLOGY OF CLINICAL 1.1. PRINCIPLES OF PHARMACOKINETICS PHARMACODYNAMICS AND Any substance that produces a change in biological function through its chemical actions and has been registred as a drug in specific drug's form by Ukrainian Pharmocology Committee may be used as a DRUG. Drugs may be synthetic in origin, chemicals obtained from plants or animals, or products of genetic engineering. A MEDICINE is a chemical preparation, which usually but not necessarily contains one or more drugs, administered with the intention of producing a therapeutic effect. Medicines usually contain other substances (excipients, stabilisers, solvents, etc.) besides the active drug to make them more convenient to use. To be a drug, the substance must be administered in the body rather than being released by physiological mechanism. In majority of cases the drug molecule interacts with specific molecules in the biological system that plays a regulatory role (receptor). The receptors are different components of a cell or an organism that interact with drugs and initiate a chain of biochemical events leading to the drug's intended effects. In most cases, drugs known as chemical antagonists may interact directly with other drugs, while a few other drugs (e.g., osmotic agents) interact almost exclusively with water molecules. Drugs may be synthesized within the body (e.g., hormones) or may be chemicals not synthesized in the body (xenobiotics). Poisons may be used as drugs too. The effects (positive or toxical) depend on the doses. Toxins are usually defined as poisons of biologic origin, i.e., synthesized by plants or animals, in contrast to inorganic poisons such as lead and arsenic. Receptors have become the central focus of investigation of drug effects and their mechanisms of action (Pharmocodynamics). Many drug receptors have been isolated and characterized in detail, thus 3 opening the way to precise understanding of the molecular basis of drug action. The actions and clinical uses of drugs may be categorised as follows: Receptors largely determine the quantitative relations between dose or concentration of drug and pharmacologic effects. The receptor's affinity for binding a drug determines the concentration of the drug required forming a significant number of drug-receptor complexes, and the total number of receptors may limit the maximal effect of a drug. Receptors are responsible for selectivity of drug action. The molecular size, shape, and electrical charge of a drug determine whether and with what affinity it will bind to a particular receptor among the vast array of chemically different binding sites available in a cell, tissue, or a patient. Accordingly, changes in the chemical structure of a drug can dramatically increase or decrease a new drug affinity for different classes of receptors, with resulting alterations in therapeutic and toxic effects. Receptors mediate the actions of both pharmacologic agonists and antagonists. Some drugs and many natural ligands, such as hormones and neurotransmitters, regulate the function of receptor macromolecules as agonists, i.e., they activate the receptor to signal as a direct result of binding to it. Other drugs function as pharmacologic antagonists, i.e., they bind to receptors but do not activate generation of a signal. Consequently, they interfere with the ability of an agonist to activate the receptor. Thus, the effect of a socalled "pure" antagonist on a cell or in a patient depends entirely on its preventing the binding of agonist molecules and blocking their biological actions. Some of the most useful drugs in clinical medicine are pharmacological antagonists. In regular clinical practice, a drug is intended to reach its site of action after administration by a convenient route. In some cases, the drug is either readily absorbed or distributed, or it is administered and then converted into active drugs by biological processes in the body. This process is known as Pharmacokinetics. In only a few cases, it is possible to directly apply a drug to its target site, e.g., 4 topical application of anti-inflammatory agent to inflamed skin or mucous membrane. Most often, a drug is administered into one body compartment, e.g., the gut, and must move to its site of action in another compartment, eg, the brain. This requires that the drug should be absorbed into the blood from its site of administration and distributed to its site of action, permeating through the various histological barriers that separate these compartments. For a drug given orally to produce an effect in the central nervous system, these barriers include the tissues that comprise the wall of the intestine, the capillaries that perfuse the gut, and the "blood-brain barrier," the walls of the capillaries that perfuse the brain. Finally, after bringing about its effect, a drug should be eliminated at a reasonable rate by metabolic inactivation, by excretion from the body, or by a combination of these processes. 1.2. ROUTES OF ADMINISTRATION Common routes of administration and some of their features include the following: 1. Oral (swallowed): The oral route offers maximum convenience, but absorption may be slower and less complete than when parenteral routes are used. Ingested drugs are subject to the first-pass effect, in which a significant amount of the agent is metabolized in the gut wall and the liver before it reaches the systemic circulation. Thus, some drugs have low bioavailability when given orally. 2. Intravenous: The intravenous route offers instantaneous and complete absorption (by definition, bioavailability is 100%). This route is potentially more dangerous, however, because of the high blood levels that am produced if administration is too rapid. 3. Intramuscular: Absorption from an intramuscular injection site is often (not always) faster and more complete (higher bioavailability) than with oral administration. Large volumes (e.g., > 5 mL into each buttock) may be given. First-pass metabolism is avoided. 5 4. Subcutaneous: The subcutaneous route offers slower absorption than the intramuscular route. Large volume bolus doses are less feasible. First-pass metabolism is avoided. 5. Buccal and sublingual: The buccal route (in the pouch between gums and cheek) permits direct absorption into the systemic venous circulation, bypassing the hepatic portal circuit and first-pass metabolism. This process may be fast or slow depending on the physical formulation of the product. The sublingual route (under the tongue) offers the same features as the buccal route. 6. Rectal (suppository): The rectal route offers partial avoidance from the first-pass effect (though not as complete as the sublingual route). Larger amounts of drugs and drugs with unpleasant taste are better administered rectally than by the buccal or sublingual routes. Some drugs administered rectally may cause significant irritation. 7. Inhalation: In case of respiratory diseases, the inhalation route offers delivery closest to the target tissue. This route often provides rapid absorption because of the large alveolar surface area available. 8. Topical: The topical route includes application to the skin or to the mucous membrane of the eye, nose, throat, airway, or vagina for local effect. The rate of absorption varies with the area of application and the drug formulation but is usually slower than any of the routes listed above. 9. Transdermal: The transdermal route involves application to the skin for systemic effect. Absorption usually occurs very slowly, but the first-pass effect is avoided. 1.3. DRUG INTERECTIONS The practical doctors prescribe more than one drug usually. But, if the doctor wants to prescribe a few different drugs by chemical structure and pharmacological action, he must remember about interactions’ between the drugs. There are several types of drug-drug interections - Addition, Synergism, Potentation, Antagonism (Table 1). 6 Table 1- Type of drug-drug interactions Type of interaction ADDITION – the response elicited by combined drugs is EQUAL TO the combined responses of individual drugs SYNERGISM – the response elicited by combined drugs is MORE THAN the combined responses of individual drugs POTENTATION – a drug which has no effects or has small effect enhances the effect of a another drug ANTAGONISM – a drug inhibits the effect of another drug. Usually the antagonism has no inherent activity Mathematical example 1+1=2 1+1>2 0+1>1 1+1=0 Drug ANTAGONISM occurs by various mechanisms: – Chemical antagonism (interaction in solution) – Pharmacokinetic antagonism (one drug affects the absorption, metabolism or excretion of another) – Competitive antagonism (both drugs bind to the same site of the receptors); the antagonism may be reversible or irreversible – Non-competitive antagonism (the antagonist interrupts receptor-effector linkage) – Physiological antagonism (two agents produce opposing physiological effects) The goal of therapy is to achieve a positive outcome with least side effects. When a medicine is selected for a particular patient, the doctor must determine the lowest possible dose to achieve the desirable goal. This aim is achieved by creating the therapeutic concentration of the drug in the tissue close to the target receptor. This “safe dosing” is achieved by testing on healthy volunteers and patients with average physical ability to absorb, distribute, and eliminate this drug; although it has to be kept in mind that this drug 7 may not be suitable for all patients. Several physiological factors and parameters require the reorganization of dose levels and calibration of the aimed concentration. These factors may be physiological (organ maturation in infants) or pathological (heart failure, renal failure etc). In most clinical setups, medications are administered in a way so as to maintain a constant presence of the active biological form of the drug in the body, i.e., just the required amount of medication is administered so as to replenish the volume of drug lost from the body by process of elimination. Therefore, calculation of the appropriate maintenance dose is, also, of vital importance. In the next step, the clinician should consider the time of action of the drug administered. This decision is based upon the approach to treatment and the severity of the disease. The frequency of administration per day depends upon various pharmacological parameters like volume of distribution, availability, elimination rate, half-life of the drug, bioavailability, etc. The most frequent areas of concern which can cause dangerous consequences are creation of very low or very high target concentration for a very long period of time and incidences of drug accumulation which may cause toxicity. Whenever drug doses are repeated, the drug will accumulate in the body until dosing stops. This is because it takes an infinite time (in theory) to eliminate all of a given dose. In practical terms, this means that if the dosing interval is shorter than four half-lives, accumulation will be detectable. Accumulation is inversely proportional to the fraction of the dose lost in each dosing interval. The fraction lost is 1 minus the fraction remaining just before the next dose. The fraction remaining can be predicted from the dosing interval and the half-life. THERAPEUTIC RANGE is the ratio between the dose that produces toxicity and the therapeutic dose of the drug, used as a measure of the relative safety of the drug for particular treatment. THERAPEUTIC INDEX = Toxic Dose/Effective Dose The drug is administered once every half-life (i.e., every 8 hours). Drug continues to accumulate (i.e., concentrations rise) until steady state (rate in = rate out) is reached at approximately 5 half-lives (about 40 hours). It is very important in practical work to remember 8 about the therapeutic index and therapeutic range of a drug. (by Charles R. Craig et al.) Thus therapeutic index is a measure of the drug's safety, since a large value indicates that there is a wide margin between doses that are effective and doses that are toxic. The therapeutic index is used assessing safety of drugs. It is the difference between the mimimum and Picture 1 - Concentration / time profile for a maximum therapeutic hypothetical drug administered orally in toxic concentrations multiple doses of a drug. A narrow therapeutic index is a very small range of doses at which a medication provides benefits without causing severe or fatal complications. 2. ANTIHYPERTENSIVE AGENTS 2.1. GENERAL PRINCIPLES TREATMENT OF HYPERTENSION Hypertension is diagnosed when through regular check-ups of high blood pressure in a patient. The diagnosis is primarily a prediction to consequences for the patient rather than citing the cause of the pathology. Epidemiological studies indicate that high blood pressure poses a direct risk to organs such as heart, kidney and brain and may 9 cause damage to them. Even incidences of mild hypertension (BP 140/90 mmHg) increase the overall risk of organ damage. Hypertension is caused by an increase in peripheral vascular smooth muscle tone, which leads to increased arteriolar resistance and thereby reduced capacitance of the venous system. In most cases, the cause of the increased vascular tone is unknown. Hypertension is an extremely common disorder, and it has been estimated that 20 percent of the population is suffering from this chronic disorder. It has also been noted that most of these individuals are mostly asymptomatic, but chronic hypertension may be systolic or diastolic and can lead to increased risk of cardiovascular problems which may be strokes, acute myocardial infarction, and congestive heart failure or renal damage. Tablе 2 - Classification of hipertension for adults Pressure Category Blood Pressure (mm Hg) Systolic Diastolic Normal < 120 < 80 Pre-hypertension 120–139 80–89 Hypertension, stage 1 140–159 90–99 Hypertension, stage 2 < 160 < 100 A specific cause of hypertension can be established in only 1015% of patients. It is important to consider specific causes in each case, however, because some of them are amenable to definite surgical treatment: renal artery constriction, coarctation of the aorta, pheochromocytoma, Cushing's disease, and primary aldosteronism. Patients in whom no specific cause of hypertension can be found are said to have essential hypertension. High blood pressure is usually caused by a combination of several (multifactorial) disorders. Epidemiologic evidence points to genetic inheritance, psychological stress, and environmental and dietary 10 factors (high salt and low potassium or calcium intakes) that perhaps contribute to the development of hypertension. Blood pressure increase with age does not occur in populations with low daily sodium intake. Ther are many factors influencing blood pressure. More often, we have the combination of three factors: Arterial blood pressure = CARDIAC OUTPUT × PERIPHERAL RESISTANCE x BLOOD VOLUME Picture 2 - Main pharmacological groups that are clinicaly used in the treatment of hypertension Mild hypertension can often be controlled with a single drug. More severe hypertension may require treatment with several drugs that are selected to minimize adverse effects of the combined regimen. 11 Table 3 - Exampels of target action Reduce overload fluid Diuretics and captopril decrease blood volume by increasing the volume of water in the excreted urine Reduce sympathetic Clonidine is an agonist at α2 receptors. outflow from the Postsynaptic α2 receptors inhibit brain sympathetic outflow, and presynaptic α2 receptors inhibit further release of the sympathetic agonist, norepinephrine Block adrenergic Atenolol is a β1 adrenergic receptor receptors in the antagonist that reduces heart rate and heart myocardial work Dilate blood vessels Prasosin blocks α1 adrenergic receptors, causing vasodilation. Nifedipine blocks calcium entry into smooth muscle cells of arterial walls, preventing contraction. Hydralazine relaxes arterioles 2.2. CLINICAL USES OF ANTIHYPERTENSIVE DRUGS Ther are some more important aspects that doctors must remember: Pharmacotherapy: Treatment for hypertension is complex because the disease is often asymptomatic and is diagnosed by chance. Also, the fact is that the drugs are expensive and may cause adverse compensatory effects which may precipitate into a crisis long with significant drug related toxicity. Howewer, the overall toxic effect of the drugs can be reduced, and the effect over compensation can be minimized by use of combination of drugs prescribed at a lower dose. This therapeutic approach is generally accepted in patients with severe or resistant hypertension. In normal practice, these drugs are added in a stepwise fashion and each additional drug 12 is chosen from a different subgroup until target blood pressure has been achieved. The regulatory steps include lifestyle modification like restriction of amount of salt in diet, weight management, physical exercises and medications. Treatment is generally initiated with any of the 5 firstline choice drugs, depending upon the patient: 1. Diuretics. 2. Sympathoblockers. 3. Ca+ channel blockers. 4. ACE inhibitors. 5. Angiotensin II receptor blockers. If blood pressure is inadequately controlled, a second drug is added. A β-blocker is usually added if the initial drug was a diuretic, or a diuretic is added if the first drug was a β-blocker. A vasodilator can be added as a third step for those patients who still fail to respond. 2.3. CLASSIFICATION OF ANTIHYPERTENSIVE DRUGS I First-line therapy: - Diuretics: 1. Thiazides and related agents (hydrochlorothiazide, chlorthalidone, etc.) 2. Loop diuretics (furosemide, bumetanide, torsemide, ethacrynic acid) 3. Potassium sparing diuretics (spironolacton, triamteren) - Adrenoreceptor-blocking agents: 1. β-Adrenergic antagonists (metoprolol, atenolol, bisoprolol etc.) 2. Mixed adrenergic antagonists (labetalol, carvedilol) - Blockers of slow Ca2+channels (verapamil, diltiazem, nimodipine, felodipine, nicardipine, isradipine, amlodipine) 13 - Angiotensin-converting enzyme inhibitors (captopril, enalapril, lisinopril, quinapril, ramipril, benazepril, fosinopril, moexipril, perindopril, trandolapril) – Angiotensin II receptor antagonists (or blockers) (losartan, candesartan, irbesartan, valsartan, telmisartan, eprosartan) II Second-line therapy: - Vasodilators: 1. Arterial (hydralazine, minoxidil, diazoxide, fenoldopam) 2. Myotropical (dibazol, papaverin) - Sympatholytic drugs: 1. Alpha-adrenergic antagonists (prazosin, terazosin, doxazosin, phenoxybenzamine, phentolamine) 2. Centrally acting antyhypertensive agents (methyldopa, clonidine, guanabenz, guanfacine) 3. Adrenergic neuron blocking agents (guanadrel, reserpine) - Potassium channel activators (monoxidil, diazoxidum) - Nitric oxide donors (sodium nitroprusside) – Gangloiblockers (pentaminum, hygronium, benzohexonium) The ability of drugs to control the compensatory responses induced by other drugs in steps 2 and 3 should be noted (e.g., propranoloi reduces the tachycardia induced by hydralazine). Thus, rational polypharmacy minimizes toxicities while producing additive or supra-additive therapeutic effects. 1. Monotherapy: It has been found in large clinical studies that many patients do well on a single drug (e.g., an ACE inhibitor, calcium channel blocker, or α-blocker). This approach to the treatment of mild and moderate hypertension has become more popular than stepped care because of its simplicity, better patient compliance, and with modern drugs, a relatively low incidence of toxicity. 2. Age and Ethnicity: Older patients of most races respond better to diuretics and beta-blockers than to ACE inhibitors. Blacks of all ages respond better to diuretics and calcium channel blockers, less well to ACE inhibitors. 14 3. Malignant Hypertension: Malignant hypertension is an accelerated phase of severe hypertension associated with rising blood pressure and rapidly progressing damage to vessels and end organs. This condition may be signaled by deterioration of renal function, encephalopathy, and retinal hemorrhages or by angina, stroke, or myocardial infarction. Management of malignant hypertension must be carried out on an emergency basis in the hospital. Powerful vasodilators (nitroprusside or diazoxide) are combined with diuretics (furosemide) and β-blockers to lower blood pressure to the 140–160/90–110 mm Hg range promptly (within a few hours). Further reduction is then pursued more slowly. 2.3.1. DIURETICS These agents are inhibitors of renal ion transporters that decrease the reabsorption of Na+ at different sites in nephron. As a result, Na+ and other ions, such as Cl-, enter the urine in greater than normal amounts along with water, which is carried passively to maintain osmotic equilibrium. Diuretics thus increase the volume of urine and often change its pH as well as the ionic composition of the urine and blood. The efficacy of the different classes of diuretics varies considerably: with the increase in Na+ secretion varying from less than two percent for the weak, potassium-sparing diuretics to over 20% for the most potent loop diuretics. In addition to these iontransport inhibitors, there are osmotic diuretics that prevent water reabsorption as well as aldosterone antagonists and a carbonic anhydrase inhibitor. The major clinical uses of diuretics are in managing disorders involving abnormal fluid retention (edema) or treating hypertension in which their diuretic action causes a decreased blood volume, leading to reduced blood pressure. Initial decrease of blood pressure owing to diuretics use is the result of increased sodium and water excretion and reduced volume of circulating blood. In 6–8 weeks after initiation of treatment with diuretics, diuretic effect is gradually reduced and cardiac output is normalized. It is the result of renin activity increase owing to reduction of plasma volume and blood pressure. Under these 15 conditions, hypotensive effect of diuretics develops owing to decrease of peripheral vessels resistance. Reduction of blood-vessel tone is the result of gradual decrease of intracellular sodium and increase of intracellular potassium in cells of vessel walls. Drug Mechanism of Action Indication Adverse Effect 1 2 3 4 5 Chlorothiazide Chlorthalidone Hydrochlorothiazide Indapamide Metolazone Inhibits sodium and chloride reabsorpion in thick ascending loop of Henle and early distal tubule. Loss of K+, Na+, and CIcauses 3 × increases in urine output. Sodium loss results in GFR Ideal starting agent for hypertension, chronic edema, idiopathic hypercalcuria. Used to DECREASE urine output in diabetes insipidus (low GFR causes increased reabsorption in proximal nephron, works only with saltrestricted diet) Hypokalemia, hyponatremia, hyperglycemia, hyperuricemia, hypercalcemia, oliguria, anuria, weakness, decreased placental flow, sulfonamide allergy, GI distress Thiazide diuretics Group Table 4 - Summaries of diuretic drugs 16 Table 4 continuation Potassium- sparing diuretics Loop acting diuretics 1 2 3 4 Furosemide Torasemide Bumetanide Etnacrynic acid Inhibits chloride reabsorption in the thick ascending limb of the loop of Henle. High loss of K+ in urine Preferred diuretic in patients with low GFR and in hypertensive emergencies, edema, pulmonary edema, to mobilize large volumes of fluid, and reduce serum potassium levels Hyponatremia, hypokalemia, dehydration, hypotension, hyperglycemia, hyperuricemia, hypocalcemia, ototoxicity, sulfonamide allergy, hypomagnesemia, hypochloremic alkalosis, hypovolemia Amiloride Spironolactone (Aldactone) Triamteren Antagonist of aldosterone (aldosterone causes Na+ retention). Directly increases Na+ excretion and decreases K+ secretion in distal convoluted tubule Used with other diuretics because K+-sparing effects lessen hypokalemic effects. May correct metabolic alkaosis. Also used to treat or diagnose hyperaldosteronism. (NOT triamteren) Hyperkalemia, sodium or water depletion. Patients with diabetes mellitus may develop glucose intolerance. Spironolactone causes endocrine imbalances (acne, oily skin, hirsutism, gynecomastia) 17 5 Table 4 continuation 2 3 4 5 Acetazolamide Carbonic anhydrase inhibitors potently inhibit carbonic anhydrase, resulting in nearly complete abolition of NaHCO3 reabsorption in the proximal tubule Although acetazolamide is used for treatment of edema. The major indication for carbonic anhydrase inhibitors is open-angle glaucoma May cause bone marrow depression, skin toxicity, sulfonamidelike renal lesions, and allergic reactions in patients hypersensitive to sulfonamides Mannitol Urea Osmotically inhibits sodium and water reabsorption. Initially increases plasma volume and blood pressure Acute renal failure, acute closed angle glaucoma, brain edema, to remove overdoses of some drugs Headache, nausea, vomiting, chills, dizziness, polydipsia, lethargy, confusion, and chest pain Osmotic diuretics Carbonicanhydrase inhibitors 1 2.3.2. INHIBITORS OF THE RENIN-ANGIOTENSIN SYSTEM A major role in controlling blood pressure for both short and long time periods is played by the renin-angiotensin system (RAS). Apart from that it also plays a significant role in the pathogenesis of hypertension, acute myocardial infarction, diabetic retinopathy and congestive heart failure. This has lead to significant increase of research and exploration of the RAS and methods of its inactivation and reduction of action. In some individuals, renin, angiotensin and aldosterone play a significant role when it comes to development of 18 essential hypertension in these individuals. Almost 20% of such patients have either pathologically high or low plasma renin activity. Blood pressures of patients having high level of renin responds well to drugs like β-adrenoceptor blockers whereas angiotensin inhibitors work well for both excess renin and angiotensin levels in the body. Kidney cortex releases renin under stimulation of reduced renal arterial pressure, sympathetic neural stimulation and reduced sodium delivery or increased sodium concentration at the distal renal tubule. Angiotensinogen is acted upon by renin by splitting off the inactive precursor of angiotensin I. Angiotensin I is then converted into angiotensin II, which is an arterial vasoconstrictor primarily, by the endothelial ACE; finally it is converted into Angiotensin III, in the adrenal glands. Angiotensin II has vasoconstrictor and sodiumretention activity. Angiotensin II inhibitors block the formation of angiotensin II and inhibit its action, lower blood pressure principally by decreasing peripheral vascular resistance, improving tissue perfusion, and reducing cardiac afterload. Cardiac output and heart rate are not significantly changed. Unlike direct vasodilators, these agents do not result in reflex sympathetic activation and can be used safely in persons with ischemic heart disease. The absence of reflex tachycardia may be due to downward resetting of the baroreceptors or to enhanced parasympathetic activity. They also cause natriuresis by inhibiting secretion of aldosterone and by reducing the direct stimulatory effect of angiotensin II on reabsorption of Na+ and HCO3- in the early part of the proximal convoluted tubule. These drugs can be classified into three broad groups based on chemical structure: 1) Sulfhydryl-containing ACE inhibitors structurally related to captopril (e.g., fentiapril, pivalopril, zofenopril, and alacepril); 2) Dicarboxyl-containing ACE inhibitors structurally related to enalapril (e.g., lisinopril, benazepril, quinapril, moexipril, ramipril, trandolapril, spirapril, perindopril, pentopril, and cilazapril); 3) phosphorus-containing ACE inhibitors structurally related to fosinopril. 19 Many ACE inhibitors are ester-containing prodrugs that are 100 to 1000 times less potent but have a much better oral bioavailability than the active molecules. In general, ACE inhibitors differ with regard to three properties: potency, whether ACE inhibition is primarily a direct effect of the drug itself or the effect of an active metabolite, and pharmacokinetics (i.e., extent of absorption, effect of food on absorption, plasma halflife, and tissue captopril). Drugs Captopril, the first ACE inhibitor to be marketed, is a potent ACE inhibitor. Given orally, captopril is absorbed rapidly and has a bioavailability of about 75%. Peak concentrations in plasma occur within an hour, and the drug is cleared rapidly with a half-life of approximately 2 hours. Most of the drug is eliminated in urine: 40–50% as captopril, and the rest as dimer captopril disulfide and captopril-cysteine disulfide. The oral dose of captopril ranges from 6.25–150 mg two to three times daily, with 6.25 mg three times daily or 25 mg twice daily being appropriate for the initiation of therapy for heart failure or hypertension, respectively. Most patients should not receive daily doses in excess of 150 mg. Since food reduces the oral bioavailability of captopril by 25–30%, the drug should be given 1 hour before meals. Enalapril maleate is a prodrug that is hydrolyzed by esterases in the liver to produce the active dicarboxylic acid, enalaprilat – a highly potent inhibitor of ACE. Enalapril is absorbed rapidly when given orally and has an oral bioavailability of about 60% (not reduced by food). Although peak concentrations of enalapril in plasma occur within an hour, enalaprilat concentrations peak only after 3–4 hours. Enalapril has a half-life of only 1.3 hours, but enalaprilat, because of tight binding to ACE, has a plasma half-life of about 11 hours. Nearly all the drug is eliminated by the kidneys as either intact enalapril or enalaprilat. The oral dosage of enalapril ranges from 2.5–40 mg daily (single or divided dosage), with 2.5 and 5 mg daily being appropriate for the initiation of therapy for heart failure and hypertension, respectively. The initial dose for 20 hypertensive patients who are taking diuretics, are water- or Na+depleted, or have heart failure is 2.5 mg daily. Enalaprilat is not absorbed orally but is available for intravenous administration when oral therapy is not appropriate. For hypertensive patients, the dosage is 0.625–1.25 mg given intravenously over 5 minutes. This dosage may be repeated every 6 hours. Lisinopril is the lysine analogue of enalaprilat; unlike enalapril, lisinopril itself is active. In vitro, lisinopril is a slightly more potent ACE inhibitor than enalaprilat is. Lisinopril is absorbed slowly, variably, and incompletely (about 30%) after oral administration (not reduced by food); peak concentrations in plasma are achieved in about 7 hours. It is cleared as the intact compound by the kidney, and its half-life in plasma is about 12 hours. Lisinopril does not accumulate in tissues. The oral dosage of lisinopril ranges from 5 to 40 mg daily (single or divided dosage), with 5 and 10 mg daily being appropriate for the initiation of therapy for heart failure and hypertension, respectively. A daily dose of 2.5 mg is recommended for patients with heart failure who are hyponatremic or have renal impairment. Fosinopril contains a phosphinate group that binds to the active site of ACE. Cleavage of the ester moiety by hepatic esterases transforms fosinopril, a prodrug, into fosinoprilat, an ACE inhibitor that in vitro is more potent than captopril yet less potent than enalaprilat. Fosinopril is absorbed slowly and incompletely (36%) after oral administration (rate, but not extent, is reduced by food). Fosinopril is largely metabolized to fosinoprilat (75%) and to the glucuronide conjugate of fosinoprilat. These are excreted both in the urine and bile; peak concentrations of fosinoprilat in plasma are achieved in about 3 hours. Fosinoprilat has an effective half-life in plasma of about 11.5 hours, and its clearance is not significantly altered by renal impairment. The oral dosage of fosinopril ranges from 10 to 80 mg daily (single or divided dosage). The dose is reduced to 5 mg daily in patients with Na+ or water depletion or renal failure. Quinapril: Cleavage of the ester moiety by hepatic esterases transforms quinapril, a prodrug, into quinaprilat, an ACE inhibitor 21 that is in vitro about as potent as benazeprilat. Quinapril is absorbed rapidly (peak concentrations are achieved in 1 hour, but the peak may be delayed after food), and the rate but not extent of oral absorption (60%), may be reduced by food. Quinapril is metabolized to quinaprilat and to other minor metabolites, and quinaprilat is excreted in the urine (61%) and feces (37%). Peak concentrations of quinaprilat in plasma are achieved in about 2 hours. Conversion of quinapril to quinaprilat is reduced in patients with diminished liver function. The initial half-life of quinaprilat is about 2 hours; a prolonged terminal half-life of about 25 hours may be due to highaffinity binding of the drug to tissue ACE. The oral dosage of quinapril ranges from 5 to 80 mg daily (single or divided dosage). Ramipril: Cleavage of the ester moiety by hepatic esterases transforms ramipril into ramiprilat; an ACE inhibitor that in vitro is about as potent as benazeprilat and quinaprilat. Ramipril is absorbed rapidly (peak concentrations of ramipril are achieved in 1 hour), and the rate, but not extent of its oral absorption (50–60%) is reduced by food. Ramipril is metabolized to ramiprilat and to inactive metabolites (glucuronides of ramipril and ramiprilat and the diketopiperazine ester and acid) that are excreted predominantly by the kidneys. Peak concentrations of ramiprilat in plasma are achieved in about 3 hours. Ramiprilat displays triphasic elimination kinetics with half-lives of 2–4 hours, 9–18 hours, and greater than 50 hours. This triphasic elimination is due to extensive distribution to all tissues (initial half-life), clearance of free ramiprilat from plasma (intermediate half-life), and dissociation of ramiprilat from tissue ACE (terminal half-life). The oral dosage of ramipril ranges from 1.25 to 20 mg daily (single or divided dosage). Moexipril is another prodrug whose antihypertensive activity is almost entirely due to its de-esterified metabolite, moexiprilat. Moexipril is absorbed incompletely, with bioavailability as moexiprilat of about 13%. Bioavailability is markedly decreased by food; therefore, the drug should be taken 1 hour before meals. The time to peak plasma concentration of moexiprilat is almost 1.5 hours, and the elimination half-life varies between 2 and 12 hours. The recommended dosage range is 7.5 to 30 mg daily in one or two 22 divided doses. The dosage range is halved in patients who are taking diuretics or who have renal impairment. Perindopril is a prodrug, and 30–50% of systemically available perindopril is transformed to perindoprilat by hepatic esterases. Although the oral bioavailability of perindopril (75%) is not affected by food, the bioavailability of perindoprilat is reduced by approximately 35%. Perindopril is metabolized to perindoprilat and to inactive metabolites (glucuronides of perindopril and perindoprilat, dehydrated perindopril, and diastereomers of dehydrated perindoprilat) that are excreted predominantly by the kidneys. Peak concentrations of perindoprilat in plasma are achieved in 3–7 hours. Perindoprilat displays biphasic elimination kinetics with half-lives of 3 – 10 hours (the major component of elimination) and 30–120 hours (owing to slow dissociation of perindoprilat from tissue ACE). The oral dosage ranges from 2 to 16 mg daily (single or divided dosage). Table 5 - Comparison of currently available ACE-inhibitors Agent Captopril Enalapril Lisinopril Ramipril Quinilapril Moexipril Onset (min) 15–30 60 60 60–120 60 90 Duration (hr) 10-12 24 24 24 24 24 T 1\2 (hr) 2 11 12 13–17 2 2–9 Elimination Renal Renal Renal Renal Renal Renal+hepatic Adverse Effects In general ACE inhibitors are well tolerated and serious adverse effects to their use are rare. Metabolic side effects are not generally seen after prolonged therapy with ACE inhibitors. The drug does not alter plasma concentration of uric acid or calcium, and have been seen, to even prevent insulin sensitivity, in patients with resistance towards insulin and effects like decrease of cholesterol and lipoprotein levels in renal diseases pertaining to proteinuria. 23 Hypotension: A steep fall in blood pressure may occur following the first dose of an ACE inhibitor in patients with elevated PRA. In this regard, care should be exercised in patients who are saltdepleted, in patients being treated with multiple antihypertensive drugs, and in patients who have congestive heart failure. In such situations, treatment should be initiated with very small doses of ACE inhibitors, or salt intake should be increased and diuretics withdrawn before beginning therapy. Cough: In 5% to 20% of patients, ACE inhibitors induce a bothersome, dry cough; it usually is not dose-related, occurs more frequently in women than in men, usually develops between 1 week and 6 months after initiation of therapy, and sometimes requires cessation of therapy. This adverse effect may be mediated by the accumulation in the lungs of bradykinin, substance P, and/or prostaglandins. Thromboxane antagonist - aspirin, and iron supplementation reduce coughing induced by ACE inhibitors. Once ACE inhibitors are stopped, the cough disappears usually within 4 days. Hyperkalemia: Despite some reduction in the concentration of aldosterone, significant K+ retention is rarely encountered in patients with normal renal function who are not taking other drugs that cause K+ retention. However, ACE inhibitors may cause hyperkalemia in patients with renal insufficiency or in patients taking K+-sparing diuretics, K+ supplements, adrenergic receptor blockers, or NSAIDs. Acute Renal Failure: Angiotensin II, by constricting the efferent arteriole, helps to maintain adequate glomerular filtration when renal perfusion pressure is low. Consequently, inhibition of ACE can induce acute renal insufficiency in patients with bilateral renal artery stenosis, stenosis of the artery to a single remaining kidney, heart failure, or volume depletion owing to diarrhea or diuretics. Older patients with congestive heart failure are particularly susceptible to ACE inhibitor–induced acute renal failure. However, in nearly all patients who receive appropriate treatment, recovery of renal function occurs without sequelae. Fetopathic Potential: Although ACE inhibitors are not teratogenic during the early period of organogenesis (first trimester), 24 continued administration of ACE inhibitors during the second and third trimesters can cause oligohydramnios, fetal calvarial hypoplasia, fetal pulmonary hypoplasia, fetal growth retardation, fetal death, neonatal anuria, and neonatal death. These fetopathic effects may be due in part to fetal hypotension. While ACE inhibitors are not contraindicated in women of reproductive age, once pregnancy is diagnosed, it is imperative that ACE inhibitors should be discontinued as soon as possible. If necessary, an alternative antihypertensive regimen should be instituted. The fetus is not at risk of ACE inhibitor-induced pathology if ACE inhibitors are discontinued during the first trimester of pregnancy. Skin rash: ACE inhibitors occasionally cause a maculopapular rash that may or may not itch. The rash may resolve spontaneously or may respond to a reduced dosage or a brief course of antihistamines. Although initially attributed to the presence of the sulfhydryl group in captopril, a rash also may occur with other ACE inhibitors, albeit less frequently. Proteinuria: ACE inhibitors have been associated with proteinuria (more than 1 g/day); however, a causal relationship has been difficult to establish. In general, proteinuria is not a contraindication for ACE inhibitors because ACE inhibitors are renoprotective in certain renal diseases associated with proteinuria, e.g., diabetic nephropathy. Angioedema: In 0.1% to 0.5% of patients, ACE inhibitors induce a rapid swelling in the nose, throat, mouth, glottis, larynx, lips, and/or tongue. This untoward effect, called angioedema, apparently is not dose-related, and if it occurs, it does so within the first week of therapy, usually within the first few hours after the initial dose. Airway obstruction and respiratory distress may lead to death. Most cases of visceral angioedema occur in the absence of oropharyngeal edema, and because the symptoms are nonspecific, diagnosis can be elusive. Dysgeusia: An alteration in or loss of taste can occur in patients receiving ACE inhibitors. This adverse effect, which may occur more frequently with captopril, is reversible. Neutropenia is a rare but serious side effect of ACE inhibitors. Although the frequency of neutropenia is low, it occurs 25 predominantly in hypertensive patients with collagen-vascular or renal parenchymal disease. Glycosuria: An exceedingly rare and reversible side effect of ACE inhibitors is spillage of glucose into the urine in the absence of hyperglycemia (Cressman et al., 1982). The mechanism is unknown. Hepatotoxicity: Also exceedingly rare and reversible is hepatotoxicity, usually of the cholestatic variety. The mechanism is unknown. Drug Interactions Antacids may reduce the bioavailability of ACE inhibitors; capsaicin may worsen ACE inhibitor-induced cough; NSAIDs, including aspirin, may reduce the antihypertensive response to ACE inhibitors; and K+-sparing diuretics and K+ supplements may exacerbate ACE inhibitor–induced hyperkalemia. ACE inhibitors may increase plasma levels of digoxin and lithium and may increase hypersensitivity reactions to allopurinol. 2.3.3. ANGIOTENSIN II RECEPTOR ANTAGONISTS As discussed earlier, angiotensin II has significant effect of vasoconstriction, contraction of vascular tone of vessels rapid pressor responses, slow pressor responses, thirst, vasopressin release, aldosterone secretion, release of adrenal catecholamines, enhancement of noradrenergic neurotransmission, increases in sympathetic tone, changes in renal function, and cellular hypertrophy and hyperplasia. ARBs selectively and potently inhibit most of the above effects in vitro or in vivo of angiotensin II. Even though both ACE inhibitors and ARBs block the RAS, these two classes of drugs have important and significant differences which also change their therapeutic value and use: 1. ARBs reduce activation of AT1 receptors more effectively than do ACE inhibitors. ACE inhibitors reduce the biosynthesis of angiotensin II produced by the action of ACE on angiotensin I but do not inhibit alternative non-ACE angiotensin II – generating pathways. Because ARBs block the AT1 receptor, the actions of 26 angiotensin II via the AT1 receptor are inhibited regardless of the biochemical pathway leading to angiotensin II formation. 2. In contrast to ACE inhibitors, ARBs permit activation of AT2 receptors. ACE inhibitors increase renin release; however, because ACE inhibitors block the conversion of angiotensin I to angiotensin II, ACE inhibition is not associated with increased levels of angiotensin II. ARBs also stimulate renin release; however, with ARBs, this translates into a several-fold increase in circulating levels of angiotensin II. Because AT2 receptors are not blocked by clinically available ARBs, this increased level of angiotensin II is available to activate AT2 receptors. 3. ACE inhibitors may increase angiotensin levels more than do ARBs. ACE is involved in the clearance of angiotensin, so inhibition of ACE may increase angiotensin levels more than do ARBs. 4. ACE inhibitors increase the levels of a number of ACE substrates, including bradykinin. Table 6 Comparisons of currently available receptor blockers Agent Losartan Valsartan Ibesartan Candesartan Telmisartan Onset (min) 60–90 120 60–120 120-240 60–180 Duration (hr) 24 24 24 24 24 T 1\2 (hr) 2–9 6 11–15 9 24 Elimination Hepatic+Renal Hepatic Hepatic Hepatic+Renal Hepatic Oral bioavailability of ARBs is generally low (<50%, except for irbesartan, with 70% available), and protein binding is high (>90%). All ARBs are approved for the treatment of hypertension. In addition, irbesartan and losartan are approved for diabetic nephropathy, losartan is approved for stroke prophylaxis, and valsartan is approved for patients with heart failure who are intolerant of ACE inhibitors. The efficacy of ARBs in lowering blood pressure is comparable with that of other established antihypertensive drugs, with an adverse-effect profile similar to that 27 of placebo. ARBs also are available as fixed-dose combinations with hydrochlorothiazide. Losartan is well tolerated in patients with heart failure and is comparable to enalapril with regard to improving exercise and is as effective as captopril in improving symptoms and reduced mortality more than has captopril. In part via blood pressure-independent mechanisms, ARBs are renoprotective in type 2 diabetes mellitus. Based on these results, many experts now consider them the drugs of choice for renoprotection in diabetic patients. Also, irebesartan appears to maintain sinus rhythm in patients with persistent, long-standing atrial fibrillation. Losartan is reported to be safe and highly effective in the treatment of portal hypertension in patients with cirrhosis and portal hypertension without compromising renal function. Drugs Candesartan cilexetil is an inactive ester prodrug that is completely hydrolyzed to the active form, candesartan, during absorption from the gastrointestinal tract. Peak plasma levels are obtained 3 – 4 hours after oral administration, and the plasma halflife is about 9 hours. Plasma clearance of candesartan is due to renal elimination (33%) and biliary excretion (67%). The plasma clearance of candesartan is affected by renal insufficiency but not by mild to moderate hepatic insufficiency. Candesartan cilexetil should be administered orally once or twice daily for a total daily dosage of 4 – 32 mg. Irbesartan: Peak plasma levels are obtained approximately 1.5–2 hours after oral administration, and the plasma half-life ranges from 11 to 15 hours. Irbesartan is metabolized in part to the glucuronide conjugate, and the parent compound and its glucuronide conjugate are cleared by renal elimination (20%) and biliary excretion (80%). The plasma clearance of irbesartan is unaffected by either renal or mild to moderate hepatic insufficiency. The oral dosage of irbesartan is 150–300 mg once daily. Losartan: Approximately 14% of an oral dose of losartan is converted to the 5-carboxylic acid metabolite EXP3174, which is 28 more potent than losartan as an AT1-receptor antagonist. The metabolism of losartan to EXP3174 and to inactive metabolites is mediated by CYP2C9 and CYP3A4. Peak plasma levels of losartan and EXP3174 occur approximately 1–3 hours after oral administration, respectively, and the plasma half-lives are 2.5 and 6–9 hours, respectively. Losartan should be administered orally once or twice daily for a total daily dose of 25–100 mg. In addition to being an ARB, losartan is a competitive antagonist of the thromboxane A2-receptor and attenuates platelet aggregation. Telmisartan: Peak plasma levels are obtained approximately 0.5–1 hour after oral administration, and the plasma half-life is about 24 hours. Telmisartan is cleared from the circulation mainly by biliary secretion of intact drug. The plasma clearance of telmisartan is affected by hepatic but not renal insufficiency. The recommended oral dosage of telmisartan is 40 to 80 mg once daily. Valsartan: Peak plasma levels occur approximately 2 – 4 hours after oral administration, and the plasma half-life is about 9 hours. Food markedly decreases absorption. Valsartan is cleared from the circulation by the liver (about 70% of total clearance). The plasma clearance of valsartan is affected by hepatic but not renal insufficiency. The oral dosage of valsartan is 80–320 mg once daily. Adverse Effects The incidence of discontinuation of ARBs owing to adverse reactions is comparable with that of placebo. Unlike ACE inhibitors, ARBs do not cause cough, and the incidence of angioedema with ARBs is much less than with ACE inhibitors. As with ACE inhibitors, ARBs have teratogenic potential and should be discontinued before the second trimester of pregnancy. ARBs should be used cautiously in patients whose arterial blood pressure or renal function is highly dependent on the renin–angiotensin system (e.g., renal artery stenosis). In such patients, ARBs can cause hypotension, oliguria, progressive azotemia, or acute renal failure. ARBs may cause hyperkalemia in patients with renal disease or in patients taking K+ supplements or K+-sparing diuretics. ARBs enhance the 29 blood pressure–lowering effect of other antihypertensive drugs, a desirable effect but one that may necessitate dosage adjustment. 2.3.4. ANTIADRENERGIC DRUGS Adrenergic agonists increase blood pressure by stimulating the heart (β1 receptors) and/or constricting peripheral blood vessels (α1 receptors). In hypertensive patients, adrenergic effects can be suppressed by inhibiting release of adrenergic agonists or by antagonizing adrenergic receptors. Presynaptic adrenergic release inhibitors are divided into "central" and "peripheral" antiadrenergics. Central antiadrenergics prevent sympathetic (adrenergic) outflow from the brain by activating inhibitory α2 receptors. By reducing sympathetic outflow, these agents encourage "parasympathetic redominance"and prevent norepinefrime release from peripheral nerve (e.g., those which terminate on the heart). These agents deplete norepinephrine stores in nerve terminals. Alpha and beta blockers compete with endogenous agonists for adrenergic receptors. Blockage of (α1-adrenergic receptors inhibits vasoconstriction and occupation of β1 receptors prevents adrenergic stimulation of the heart. Selective α1 or β1 blockers replace nonspecific β blockers, because they produce fewer undesirable effects. Beta receptor antagonists are predominantly effective on the cardiovascular system because of their therapeutic efficacy. These antagonist preparations are widely used to treat hypertension, angina, and acute coronary syndromes. Their potent use lies in the treatment of congestive heart failure, supraventricular and ventricular arrhythmias. Due to positive chronotropic and ionotropic effects of catecholamines, β-receptor antagonists are capable of slowing down heart rate and myocardial contractility. This effect is modest when β receptors have a low tonic stimulation predisposed by stress, anxiety, physical exercise or motion. But when the sympathetic nervous system activity has been sufficiently activated, β-receptor antagonists counteract the stimulatory effect and decrease the 30 anticipated rise in heart rate. Short term administration of β-receptor antagonists, like propranolol, includes decrease in stroke volume and cardiac output. Rise in peripheral resistance is seen as a compensatory mechanism to normalize blood pressure due to vascular response effect and receptor blockade. Evident rise in sympathetic activity leads to activation of the vascular receptors. But after prolonged use of β-receptor antagonists total peripheral resistance tend to normalize and returns to normal values or decreases in case of patients with hypertension. Drugs, like labetolol and carvedilol which are simultaneously α-receptor blockers, show higher efficacy with a greater decrease of peripheral resistance. Similar effects are seen with other receptor antagonists wich are direct vasodilators as well as hydralazine. The β-receptor antagonists have significant effects on cardiac rhythm and automaticity. Although these effects were considered to be due exclusively to blockade of β1-receptors, β2-receptors likely also regulate heart rate in humans. Beta-3 receptors also have been identified in normal myocardial tissue in some species, including humans. The β-receptor antagonists reduce sinus rate, decrease the spontaneous rate of depolarization of ectopic pacemakers, slow conduction in the atria and in the AV node, and increase the functional refractory period of the AV node. Several β1 blockers have intrinsic sympathomimetic activity (act as weak agonists at some adrenergic receptors). These drugs stimulate β2 receptors, which reduces the likelihood that rebound hypertension (sympathetic reflex fall in blood pressure) will develop. Activated α2 receptors dilate large central arteries which provide a reservoir for blood. Drugs without intrinsic sympathomimetic activity produce an initial reduction in cardiac output and a reflexinduced rise in peripheral resistance, generally without net change in arterial pressure. In patients who respond with a reduction in blood pressure, peripheral resistance gradually returns to pretreatment values or less. Generally, persistently reduced cardiac output and possibly decreased peripheral resistance accounts for the reduction in arterial pressure. Drugs with intrinsic sympathomimetic activity produce lesser decreases in resting heart rate and cardiac output; the 31 fall in arterial pressure correlates with the fall in vascular resistance below pretreatment levels, possibly because of stimulation of vascular α2-adrenergic receptors that mediate vasodilation. The clinical significance, if any, of these differences is unknown. Drugs Metoprolol is approximately equipotent to propranolol in inhibiting stimulation of β1 adrenoceptors, such as those in the heart but 50- to 100-fold less potent than propranolol in blocking β2 receptors. Although metoprolol is in other respects very similar to propranolol, its relative cardioselectivity may be advantageous in treating hypertensive patients who also suffer from asthma, diabetes, or peripheral vascular disease. Studies of small numbers of asthmatic patients have shown that metoprolol causes less bronchial constriction than propranolol at doses that produce equal inhibition of β1-adrenoceptor responses. The cardioselectivity is not complete, however, and asthmatic symptoms have been exacerbated by metoprolol. For the treatment of hypertension, the usual initial dose is 100 mg per day. The drug sometimes is effective when given once daily, although it frequently is used in two divided doses. Dosage may be increased at weekly intervals until optimal reduction of blood pressure is achieved. If the drug is taken only once daily, it is important to confirm that blood pressure is controlled for the entire 24-hour period. Metoprolol generally is used in two divided doses for the treatment of stable angina. For the initial treatment of patients with acute myocardial infarction, an intravenous formulation of metoprolol tartrate is available. Oral dosing is initiated as soon as the clinical situation permits. Metoprolol generally is contraindicated for the treatment of acute myocardial infarction in patients with heart rates of less than 45 beats per minute, heart block greater than first-degree (PR interval 0.24 second), systolic blood pressure <100 mm Hg, or moderate-to-severe heart failure. Metoprolol also has been proven to be effective in chronic heart failure. Nadolol and carteolol, nonselective β-receptor antagonists, and atenolol, a β1-selective blocker, are not appreciably metabolized and are excreted to a considerable extent in the urine. Betaxolol and 32 bisoprolol are β1-selective blockers that are primarily metabolized in the liver but have long half-lives. Because of these relatively long half-lives, these drugs can be administered once daily. The usual starting dosage of nadolol is 40 mg/d, atenolol – 50 mg/d, carteolol – 2.5 mg/d, betaxolol –10 mg/d, and bisoprolol – 5 mg/d. Increases in dosage to obtain a satisfactory therapeutic effect should take place no more often than every 4 or 5 days. Patients with reduced renal function should receive correspondingly reduced doses of nadolol, carteolol, and atenolol. It is claimed that atenolol produces fewer central nervous system-related effects than other, more lipid-soluble β antagonists. Pindolol, acebutolol, and penbutolol are partial agonists, i.e., β blockers with some intrinsic sympathomimetic activity. They lower blood pressure by decreasing vascular resistance and appear to depress cardiac output or heart rate less than other β blockers, perhaps because of significantly greater agonist than antagonist effects at β2 receptors. This may be particularly beneficial for patients with bradyarrhythmias or peripheral vascular disease. Daily initial doses of pindolol are 10 mg; of acebutolol – 400 mg; and of penbutolol – 20 mg. Labetalol is formulated as a racemic mixture of four isomers (it has two centers of asymmetry). Labetalol has a 3:1 ratio of β:α antagonism after oral dosing. Blood pressure is lowered by reduction of systemic vascular resistance without significant alteration in heart rate or cardiac output. Because of its combined β- and α-blocking activity, labetalol is useful in treating the hypertension of pheochromocytoma and hypertensive emergencies. Oral daily doses of labetalol range from 200 to 2400 mg/d. Labetalol is given as repeated intravenous bolus injections of 20–80 mg to treat hypertensive emergencies. Carvedilol, like labetalol, is administered as a racemic mixture. The average half-life is 7–10 hours. The usual starting dosage of carvedilol for ordinary hypertension is 6.25 mg twice daily. Esmolol is a β1-selective blocker that is rapidly metabolized via hydrolysis by red blood cell esterases. It has a short half-life (9–10 minutes) and is administered by constant intravenous infusion. 33 Esmolol is generally administered as a loading dose (0.5–1 mg/kg), followed by a constant infusion. The infusion is typically started at 50–150 mcg/kg/min, and the dose is increased every 5 minutes up to 300 mcg/kg/min as needed to achieve the desired therapeutic effect. Esmolol is used for management of intraoperative and postoperative hypertension and sometimes for hypertensive emergencies, particularly when hypertension is associated with tachycardia. Table 7 - Pharmacological parameters of β blockers Agent Selectivity Lipid solubility T 1\2 (hr) Metabolism Notes Acebtalol β1 Moderate 2–3 Hepatic + Renal Partial agonist Atenolol β1 Low 6–7 Renal Betaxolol β1 Low 14–22 Hepatic + Renal Used in glaucoma Bisoprolol β1 Low 9–12 Hepatic + Renal Carvediol β1+β2 and α1 High 6–10 Hepatic Labetalol β1+β2 and α1 Moderate 6–8 Hepatic + Renal Βeta blockade Used mostly for CHF Nadolol β1+β2 Low Pindolol β1+β2 Moderate 3–4 Hepatic + Renal Partial agonist Prpranolol β1+β2 High 4–6 Hepatic Timolol β1+β2 Lowmoderate 4–5 Hepatic+ Renal Used in glaucoma 20–24 Renal Long-acting Provocation of bronchospasm Adverse Effects The most common adverse effects of receptor antagonists arise as pharmacological consequences of receptor blockade; serious adverse effects unrelated to receptor blockade are rare. 34 Cardiovascular system: Because the sympathetic nervous system provides critical support for cardiac performance in many individuals with impaired myocardial function, receptor antagonists may induce congestive heart failure in susceptible patients. Thus, receptor blockade may cause or exacerbate heart failure in patients with compensated heart failure, acute myocardial infarction, or cardiomegaly. It is not known whether receptor antagonists that possess intrinsic sympathomimetic activity or peripheral vasodilating properties are safer in these settings. Nonetheless, there is convincing evidence that chronic administration of receptor antagonists is efficacious in prolonging life in the therapy of heart failure in selected patients Bradycardia is a normal response to receptor blockade; however, in patients with partial or complete atrioventricular conduction defects, antagonists may cause life-threatening bradyarrhythmias. Particular caution is indicated in patients who are taking other drugs, such as verapamil or various antiarrhythmic agents, which may impair sinus-node function or AV conduction. It is not recommended to cease the use of receptor antagonists abruptly during a long-term treatment due to the potential risks of exacerbation of conditions like angina and increases the risk of mortality by sudden death. The mechanism of such morbidity has remained unclear even though it has been well established that patients who have undergone long term treatment with any specific kind of receptor antagonists has developed enhanced sensitivity to adrenergic receptor antagonists after the therapy has been abruptly ceased. For example, chronotropic responses to isoproterenol are blunted in patients who are receiving receptor antagonists; however, abrupt discontinuation of propranolol leads to greater-than-normal sensitivity to isoproterenol. This increased sensitivity is evident for several days after stopping propranolol and may persist for at least 1 week. The increased sensitivity can be reduced by gradual tapering the dose before discontinuation. Supersensitivity to isoproterenol also has been observed after abrupt discontinuation of metoprolol, but not of pindolol. It has been hypothesized that this increased sensitivity perhaps are caused due to up-regulation of receptors. The 35 number of receptors on circulating lymphocytes is increased in subjects who have received propranolol for long periods; pindolol has the opposite effect. Optimal strategies for discontinuation of blockers are not known, but it is prudent to decrease the dose gradually and to restrict exercise during this period. Bronchospasm: A major adverse effect of receptor antagonists is caused by blockade of β2 receptors in bronchial smooth muscle. These receptors are particularly important for promoting bronchodilation in patients with bronchospastic disease, and blockers may cause a life-threatening increase in airway resistance in such patients. Drugs with one adrenergic receptors selectivity or those with intrinsic sympathomimetic activity at β2-adrenergic receptors may be somewhat less likely to induce bronchospasm. Since the selectivity of current blockers for β1 receptors is modest, these drugs should be avoided if at all possible in patients with asthma. However, in some patients with chronic obstructive pulmonary disease, the potential advantage of using receptor antagonists after myocardial infarction may outweigh the risk of worsening pulmonary function. Central nervous system: The adverse effects of receptor antagonists that are referable to the CNS may include fatigue, sleep disturbances (including insomnia and nightmares), and depression. The previously ascribed association between these drugs and depression may not be substantiated by more recent clinical studies. An interest has been focused on the relationship between the incidence of the adverse effects of receptor antagonists and their lipophilicity; however, no clear correlation has emerged. Metabolism: As described above, adrenergic blockade may blunt recognition of hypoglycemia by patients; it also may delay recovery from insulin-induced hypoglycemia. Receptor antagonists should be used with great caution in patients with diabetes who are prone to hypoglycemic reactions; 1-selective agents may be preferable for these patients. The benefits of receptor antagonists in type 1 diabetes with myocardial infarction may outweigh the risk in selected patients. Miscellaneous: The incidence of sexual dysfunction in men with hypertension who are treated with receptor antagonists is not clearly 36 defined. Although experience with the use of adrenergic receptor antagonists in pregnancy is increasing, information about the safety of these drugs during pregnancy is still limited. Overdosage: The manifestations of poisoning with receptor antagonists depend on the pharmacological properties of the ingested drug, particularly its one selectivity, intrinsic sympathomimetic activity, and membrane-stabilizing properties. Hypotension, bradycardia, prolonged AV conduction times, and widened QRS complexes are common manifestations of overdosage. Seizures and depression may occur. Hypoglycemia is rare, and bronchospasm is uncommon in the absence of pulmonary disease. Significant bradycardia should be treated initially with atropine, but a cardiac pacemaker often is required. Large doses of isoproterenol or receptor agonist may be necessary to treat hypotension. Glucagon has positive chronotropic and inotropic effects on the heart that are independent of interactions with adrenergic receptors, and the drug has been useful in some patients. Drug Interactions Both pharmacokinetic and pharmacodynamic interactions have been noted between receptor antagonists and other drugs. Aluminum salts, cholestyramine, and colestipol may decrease the absorption of blockers. Drugs, such as phenytoin, rifampin, and phenobarbital, as well as smoking, induce hepatic biotransformation of enzymes and may decrease plasma concentrations of receptor antagonists that are metabolized extensively (e.g., propranolol). Cimetidine and hydralazine may increase the bioavailability of agents, such as propranolol and metoprolol, by affecting hepatic blood flow. Receptor antagonists can impair the clearance of lidocaine. Other drug interactions have pharmacodynamic explanations. For example, antagonists and Ca2+ channel blockers have additive effects on the cardiac conducting system. Additive effects on blood pressure between blockers and other antihypertensive agents often are employed to clinical advantage. However, the antihypertensive effects of receptor antagonists can be opposed by indomethacin and other nonsteroidal anti-inflammatory drugs. 37 2.3.5. CALCIUM CHANNEL BLOCKERS (THE CALCIUM SLOW CHANNEL BLOCKING AGENTS) Calcium channel blockers (CCB) are recommended for patients when the preferred first-line treatment (please reconsider this line) against hypertension has been proved to be inefficient or ineffective. These drugs are effective in treating hypertensive disorder in patients with diabetes or angina as an accompanying disorder. High doses of short-acting CCB are not recommended owing to increased risk towards precipitation of an attack of myocardial infarction due to excessive vasodilation and marked reflex tachycardia. The muscular tonicity of vessels and contractile function of myocardium is inherently dependent on the intracellular concentration of calcium. Calcium influxes in the cell through special voltage-sensitive calcium channels, or gates, which triggers the release of calcium ions from the sarcoplasmic reticulum and mitochondria which, in turn, increases further intracellular concentration of calcium. CCBs block this influx of calcium into the cells by binding with the L-type (slow type) calcium channels in the heart muscles and peripheral vasculature. This causes relaxation of the smooth muscle of the vessels and myocardium and reduction of tonus. Calcium channel blockers have an intrinsic natriuretic effect and, therefore, do not usually require the addition of a diuretic. These agents are useful in the treatment of hypertensive patients who also have asthma, diabetes, angina, and/or peripheral vascular disease. Black hypertensives respond well to calcium channel blockers. Classification of Calcium Channel Blockers The calcium channel blockers are divided into three chemical classes, each with different pharmacokinetic properties and clinical indications. Diphenylalkylamines: Verapamil is the only member of this class that is currently approved. Verapamil is the least selective of any calcium-channel blocker and has significant effects on both cardiac and vascular smooth muscle cells. It is used to treat angina, supraventricular tachyarrhythmias, and migraine headache. 38 Dihydropyridines: This rapidly expanding class of calcium channel blockers includes the first-generation nifedipine and five second-generation agents for treating cardiovascular disease: amlodipine, felodipine, isradipine, nicardipine, and nisoldipine. These second-generation calcium channel blockers differ in pharmacokinetics, approved uses, and drug interactions. All dihydropyridines have a much greater affinity for vascular calcium channels than for calcium channels in the heart. They are therefore particularly attractive in treating hypertension. Some of the newer agents, such as amlodipine and nicardipine, have the advantage that they show little interaction with other cardiovascular drugs, such as digoxin or warfarin, which are often used concomitantly with calcium channel blockers. Benzothiazepines: Diltiazem is the only member of this class that is currently approved. Like verapamil, diltiazem affects both cardiac and vascular smooth muscle cells; however, it has a less pronounced negative inotropic effect on the heart compared to that of verapamil. Diltiazem has a favorable side-effect profile. Table 8 - Cardivascular effects of calcium channel blockers Parameter Nifidipine Dilteazem Verapamil - - - Vasodilation +++ ++ ++ Heart rate ++ - +- Contractility 0\+ 0 0\ - Coronary vascular resistance - - - Blood flow +++ +++ ++ Blood pressure 39 Table 9 – Clinical properties of some calcium channel blocking drugs Drug Amlodipine Felodipine Isradipine Nicardipine Nifedipine Nimodipine Nisoldipine Diltiazem Verapamil Indication Angina, hypertension Hypertension, Raynaud's phenomenon, congestive heart failure Hypertension Usual Dosage 5–10 mg orally once daily 5–10 mg orally once daily Toxicity Headache, peripheral edema Dizziness, headache 2.5–10 mg orally Headache, fatigue every12 hours Angina, 20–40 mg orally Peripheral edema, hypertension every 8 hours dizziness, congestive heart headache, flushing failure Angina, 3–10 g/kg IV; 20– Hypotension, hypertension, 40 mg orally every dizziness, migraine, 8 hours flushing, nausea, cardiomyopathy, constipation, Raynaud's dependent edema phenomenon Subarachnoid 60 mg orally every Headache, hemorrhage, 4 hours diarrhea migraine Hypertension 20–40 mg orally Probably similar once daily to nifedipine Angina, 75–150 g/kg IV; Hypotension, hypertension, 30–80 mgorally dizziness, Raynaud's every 6 hours flushing, phenomenon bradycardia Angina, 75–150 g/kg IV; Hypotension, hypertension, 80–160 mg orally myocardial arrhythmias, every 8 hours depression, migraine, constipation, cardiomyopathy dependent edema 40 Adverse Effects Constipation occurs in 10% of patients treated with verapamil. Dizziness, headache, and a feeling of fatigue caused by a decrease in blood pressure are more frequent with dihydropyridines. Verapamil should be avoided in patients with congestive heart failure or with atrioventricular block due to its negative inotropic (force of cardiac muscle contraction) and dromotropic (velocity of conduction) effects. Table 10 - Adverse effects of calcium channel blockers Tachycardia Decreased heart rate Decreased A-V nodal conduction Negative inotropy Vasodilatation (flushing, edema, hypotension, headaches) Constipation, nausea 2.4. Nifidipine 0 + +++ Dilteazem 0 + ++ Verapamil + 0 0 ++ + + +\0 0 +++ ++ + +\0 SECOND-LINE THERAPY Sometimes effectivness of first-line therapy is not satisfectory or patients have contraindications. We may use drugs from the second group in these cases. 2.4.1. GANGLIONIC BLOCKING AGENTS Ganglion blockers, such as pirylen and benzoxexonium, competitively block nicotinic cholinoceptors on postganglionic neurons in both sympathetic and parasympathetic ganglia. In 41 addition, these drugs may directly block the nicotinic acetylcholine channel, in the same fashion as neuromuscular nicotinic blockers. Ganglion blockers are used for controlled hypotension; for treatment of pulmonary oedema and brain oedema; for interruption of hypertensive crisis. Nowadays, ganglion blockers are used seldom for treatment of hypertensive disease, because drugs administration results in large number of side effects: decrease of tone and motility of gastrointestinal tract and bladder, constipation, disturbances of accomodation, dry mouth. Serious complication of ganglion blockers administration is postural hypotension. Tolerance develops in case of regular administration of ganglion blockers Adverse Effects Ganglion blockers exert their side effects as a direct extension of their pharmacological effects. Sympathoplegia (excessive orthostatic hypotension and sexual dysfunction) and parasympathoplegia (constipation, urinary retention, precipitation of glaucoma, blurred vision, dry mouth, etc.) are the most commonly observed side effects in this class of drugs. The high drug toxicity and the severe drug side effects are the main reasons as for why these are not considered as the first-line treatment of hypertension anymore. 2.4.2. ALPHA 1-BLOCKERS Nonselective α-adrenoceptor antagonists relax vessels owing to blockage of both α1- and α2-adrenoceptors. But these drugs aren’t used for systemic treatment of hypertensive disease, because they don’t promote stable hypotensive effect. Shortness of effect is the result of blockage of presynaptic α2-adrenoceptors which regulate negative feedback. Blockage of these receptors results in excessive noradrenaline Prazosin, terazosin, and doxazosin produce most of their antihypertensive effect by selectively blocking α1 receptors in arterioles and venules. These agents produce less reflex tachycardia when lowering blood pressure than do non-selective α antagonists, such as phentolamine. Alpha 1-receptor selectivity allows 42 norepinephrine to exert unopposed negative feedback (mediated by presynaptic α2 receptors) on its own release in contrast, phentolamine blocks both presynaptic and postsynaptic α receptors, with the result that reflex activation of sympathetic neurons produces greater release of transmitter onto α- receptors and correspondingly greater cardioacceleration. Alpha blockers reduce arterial pressure by dilating both resistance and capacitance vessels. As expected, blood pressure is reduced more in the upright than in the supine position. Retention of salt and water occurs when these drugs are administered without a diuretic. The drugs are more effective when used in combination with other agents, such as a β blocker and a diuretic, than when used alone. 2.4.3. VASODILATORS Within this class of drugs are the oral vasodilators, hydralazine and minoxidil, which are used for long-term outpatient therapy of hypertension; the parenteral vasodilators, nitroprusside, diazoxide, and fenoldopam, which are used to treat hypertensive emergencies; and the calcium channel blockers, which are used in both circumstances. Drugs Hydralazine, a hydrazine derivative, dilates arterioles but not veins. It has been available for many years, although it was initially thought not to be particularly effective because tachyphylaxis to its antihypertensive effects developed rapidly. The benefits of combination therapy are now recognized, and hydralazine may be used more effectively, particularly in severe hypertension. Usual dosage ranges from 40 mg/d to 200 mg/d. The higher dosage was selected as the dose at which there is a small possibility of developing the lupus erythematosus-like syndrome described in the next section. However, higher dosages result in greater vasodilation and may be used if necessary. Dosing two or three times daily provides smooth control of blood pressure. 43 The most common adverse effects of hydralazine are headache, nausea, anorexia, palpitations, sweating, and flushing. In patients with ischemic heart disease, reflex tachycardia and sympathetic stimulation may provoke angina or ischemic arrhythmias. Minoxidil is a very efficacious orally active vasodilator. The effect results from the opening of potassium channels in smooth muscle membranes by minoxidil sulfate, the active metabolite. Increased potassium permeability stabilizes the membrane at its resting potential and makes contraction less likely. Like hydralazine, minoxidil dilates arterioles but not veins. Because of its greater potential antihypertensive effect, minoxidil should replace hydralazine when maximal doses of the latter are not effective or in patients with renal failure and severe hypertension, who do not respond well to hydralazine. Adverse Effects Tachycardia, palpitations, angina and edema are observed when doses of α blockers and diuretics are inadequate. Headache, sweating and hirsutism which is particularly bothersome in women, are relatively common. Minoxidil illustrates how one person's toxicity may become another person's therapy. Topical minoxidil is used as a stimulant to hair growth for correction of baldness. Sodium nitroprusside is a powerful parenterally administered vasodilator that is used in treating hypertensive emergencies as well as severe heart failure. Nitroprusside dilates both arterial and venous vessels, resulting in reduced peripheral vascular resistance and venous return. The action occurs as a result of activation of guanylyl cyclase, either via release of nitric oxide or by direct stimulation of the enzyme. The result is increased by intracellular cGMP, which relaxes vascular smooth muscle In the absence of heart failure, blood pressure decreases, owing to decreased vascular resistance, while cardiac output does not change or decreases slightly. In patients with heart failure and low cardiac output, output often increases owing to afterload reduction. Infusion solutions should be changed after several hours. Dosage typically begins at 0.5 mcg/kg/min and may be increased up to 44 10 mcg/kg/min as necessary to control blood pressure. Higher rates of infusion, if continued for more than an hour, may result in toxicity. Because of its efficacy and rapid onset of effect, the drug should be administered by infusion pump and arterial blood pressure continuously monitored via intra-arterial recording. Diazoxide is similar chemically to the thiazide diuretics but has no diuretic activity. It is bound extensively to serum albumin and to vascular tissue. Drug is an effective and relatively long-acting parenterally administered arteriolar dilator that is occasionally used to treat hypertensive emergencies. Injection of diazoxide results in a rapid fall in systemic vascular resistance and mean arterial blood pressure associated with substantial tachycardia and increase in cardiac output. Studies of its mechanism suggest that it prevents vascular smooth muscle contraction by opening potassium channels and stabilizing the membrane potential at the resting level. The most significant toxicity from diazoxide has been excessive hypotension, resulting from the recommendation to use a fixed dose of 300 mg in all patients. Such hypotension has resulted in stroke and myocardial infarction. The reflex sympathetic response can provoke angina, electrocardiographic evidence of ischemia, and cardiac failure in patients with ischemic heart disease, and diazoxide should be avoided in this situation. Diazoxide inhibits insulin release from the pancreas (probably by opening potassium channels in the cell membrane) and is used to treat hypoglycemia secondary to insulinoma. Occasionally, hyperglycemia complicates diazoxide use, particularly in persons with renal insufficiency. In contrast to the structurally related thiazide diuretics, diazoxide causes renal salt and water retention. However, because the drug is used for short periods only, this is rarely a problem. 2.4.4. CENTRALLY ACTING ADRENERGIC DRUGS These agents reduce sympathetic outflow from vasopressor centers in the brainstem but allow these centers to retain or even increase their sensitivity to baroreceptor control. Accordingly, the 45 antihypertensive and toxic actions of these drugs are generally less dependent on posture than are the effects of drugs that act directly on peripheral sympathetic neurons. Methyldopa is useful in the treatment of mild to moderate severe hypertension. It lowers blood pressure chiefly by reducing peripheral vascular resistance, with a variable reduction in heart rate and cardiac output. Most cardiovascular reflexes remain intact after administration of methyldopa, and blood pressure reduction is not markedly dependent on maintenance of upright posture. Postural (orthostatic) hypotension sometimes occurs, particularly in volume-depleted patients. One potential advantage of methyldopa is that it causes reduction in renal vascular resistance. The most frequent undesirable effect of methyldopa is overt sedation, particularly at the onset of treatment. With long-term therapy, patients may complain of persistent mental lassitude and impaired mental concentration. Nightmares, mental depression, vertigo, and extrapyramidal signs may occur but are relatively infrequent. Lactation, associated with increased prolactin secretion, can occur both in men and in women treated with methyldopa. This toxicity is probably mediated by inhibition of dopaminergic mechanisms in the hypothalamus. Clonidine: Hemodynamic studies indicate that blood pressure lowering by clonidine results from reduction of cardiac output due to decreased heart rate and relaxation of capacitance vessels, with a reduction in peripheral vascular resistance, particularly when patients are upright (when sympathetic tone is normally increased). Reduction in arterial blood pressure by clonidine is accompanied by decreased renal vascular resistance and maintenance of renal blood flow. As with methyldopa, clonidine reduces blood pressure in the supine position and only rarely causes postural hypotension. Pressor effects of clonidine are not observed after ingestion of therapeutic doses of clonidine, but severe hypertension can complicate a massive overdose. 46 Adverse Effects Dry mouth and sedation are frequent and may be severe. Both effects are centrally mediated and dose-dependent and coincide temporally with the drug's antihypertensive effect. The drug should not be given to patients who are at risk for mental depression and should be withdrawn if depression occurs during therapy. Concomitant treatment with tricyclic antidepressants may block the antihypertensive effect of clonidine. Patients exhibit nervousness, tachycardia, headache, and sweating after omitting one or two doses of the drug. Although the incidence of severe hypertensive crisis is unknown, it is high enough to require that all patients who take clonidine be carefully warned of the possibility. If the drug must be stopped, this should be done gradually while other antihypertensive agents are being substituted. Treatment of the hypertensive crisis consists of reinstitution of clonidine therapy or administration of α- and β-adrenoceptor-blocking agents. 2.4.5. HYPERTENSIVE EMERGENCY Hypertensive emergency is a rare, but life-threatening situation in which the diastolic blood pressure is either over 150 mm Hg (with systolic blood pressure greater than 210 mm Hg) in an otherwise healthy person, or 130 mm Hg in an individual with preexisting complications, such as encephalopathy, cerebral hemorrhage, left ventricular failure, or aortic stenosis. The therapeutic goal is to reduce rapidly blood pressure. Sodium Nitroprusside: Nitroprusside is administered intravenously, and it causes prompt vasodilation with reflex tachycardia. It is capable of reducing blood pressure in all patients, regardless of the cause of hypertension. The drug has little effect outside the vascular system, acting equally on arterial and venous smooth muscle. Because nitroprusside also acts on the veins, it can reduce cardiac preload. Nitroprusside is metabolized rapidly (Tl/2 of minutes) and requires continuous infusion to maintain its hypotensive action. 47 Sodium nitroprusside exerts few adverse effects except for those of hypotension caused by overdose. Nitroprusside metabolism results in cyanide ion production, although cyanide toxicity is rare and can be effectively treated with an infusion of sodium thiosulfate to produce thiocyanate, which is less toxic and is eliminated by the kidneys Nitroprusside is poisonous if given orally because of its hydrolysis to cyanide. Diazoxide: Diazoxide is a direct-acting arteriolar vasodilator. It has vascular effects like those of hydralazine. For patients with coronary insufficiency, diazoxide is administered intravenously with a p-blocker, which diminishes reflex activation of the heart. Diazoxide is useful in the treatment of hypertensive emergencies, hypertensive encephalopathy, and eclampsia. Excessive hypotension is the most serious toxicity. Labetalol: Labetalol is both an α- and β-blocker that has been successfully used in hypertensive emergencies. Labetalol does not cause the reflex tachycardia that may be associated with diazoxide. Labetalol carries the contraindications of a nonselective α-blocker. 3. ANTIANGINAL DRUGS 3.1. GENERAL PRINCIPELS IN THE TREATMENT OF ISCHEMIC HEART DISEASE (IHD) Angina pectoris is a symptom of ischemic heart disease that is frequently characterized by typical chest pain usually located substernally but sometimes perceived in the neck, shoulder, or epigastrium. There are three basic categories of angina: – Stable angina: Temporary myocardial ischemia and hypoxia that do not lead to detectable damage. Transient chest pain is induced by exertion or stress and ceases at rest. It is associated with atheromatous plaques that partially occlude one or more coronaries. When cardiac work increases (e.g., in exercise), the obstruction of flow results in the accumulation of 48 acidic metabolites and ischemic changes that stimulate myocardial pain endings. A rest usually leads to prompt relief of the pain within a few minutes. Atherosclerotic angina constitutes about 90% of angina cases and, depending on the rate of progression of the atheromas, may persist for years with little change. However, effort angina may deteriorate into unstable angina. – Unstable angina: Also known as acute coronary syndrome, is characterized by increased frequency and severity of attacks caused by repeated episodes of diminished coronary flow that result from a combination of atherosclerotic plaques, platelet aggregation at fractured plaques, and vasospasm. Unstable angina is thought to be the immediate precursor of a myocardial infarction and is treated as a medical emergency. It may develop at rest. Episodes are more severe than those of stable angina. Occasionally it leads to permanent myocardial damage, causes elevation or depression of the S-T segment and inversion of the T wave on ECG traces. – Variant (Prinzmetal's) angina: Hypoxia and ischemia to myocardium is caused by vasospasm (rather than progressive narrowing of coronary arteries). It involves reversible spasm of coronaries, usually at the site of an atherosclerotic plaque. Episodes of spasm may occur at any time, at rest, even during sleep. Vasospastic angina may deteriorate into unstable angina. Determinants of Cardiac Oxygen Requirement The pharmacologic treatment of coronary insufficiency is based on physiological factors that control the myocardial oxygen requirement. A major determinant is myocardial fiber tension, i.e., the higher the tension, the greater the oxygen requirement. Several variables contribute to fiber tension: 1. Preload: Preload (diastolic filling pressure) is a function of blood volume and venous tone. Because venous tone is mainly controlled by sympathetic outflow, activities that increase sympathetic activity usually increase preload. 2. Afterload: Afterload or arterial blood pressure is one of the systolic determinants of oxygen requirement. Arterial blood pressure 49 depends on peripheral vascular resistance, which is determined by sympathetic outflow to the arteriolar vessels. 3. Heart rate: Heart rate contributes to time-integrated fiber tension because at fast heart rates, fibers spend more time at systolic tension levels. Furthermore, at faster rates, diastole is abbreviated, and diastole constitutes the time available for coronary flow (coronary blood flow is low or nil during systole). Systolic blood pressure and heart rate may be multiplied to yield the double product, a measure of cardiac work and therefore of oxygen requirement. In patients with atherosclerotic angina, effective drugs reduce the double product. 4. Cardiac contractility: Force of cardiac contraction is another systolic factor controlled mainly by sympathetic outflow to the heart. Ejection time for ventricular contraction is inversely related to force of contraction but is also influenced by impedance to outflow. Increased ejection time increases oxygen requirement. Therapeutic Strategies: Anginal pain is primarily caused to inadequate perfusion of blood in the coronary vessels leading to a transient oxygen deficiency relative to the myocardial oxygen demand. This situation can be corrected in 2 different ways: 1. An increase in coronary oxygen supply 2. A reduction in myocardial load or oxygen demand. Pharmacological therapies include the nitrates, the calcium channel blockers, and the beta-blockers. All three groups reduce the oxygen requirement in atherosclerotic angina: nitrates and calcium channel blockers (but not beta-blockers) can also increase oxygen delivery by reducing vasospasm, but only in vasospastic angina. Myocardial revascularization corrects coronary obstruction either by bypass grafting or by angioplasty (enlargement of the lumen by means of a special catheter). Therapy of unstable angina differs from that of stable angina because urgent angioplasty is the treatment of choice in most patients and platelet clotting is the major target of drug therapy. The platelet glycoprotein IIb/IIIa inhibitors (eptifibatide and tirofiban) are used in this condition. Intravenous 50 nitroglycerin is sometimes of value. The drugs used in angina are diagrammed in Table 11. Table 11 Drugs used in the treatment of IHD Drug Organic nitrates Calcium channel blockers Βeta-adrenergic blockers Most important mechanism of action Decrease preload by vasodilatation Decrease resistance of peripheral and coronary arterioles Decrease oxygen demand by lowering heart contraction Additional effects Decrease blood pressure Negative inotropic effect Contraindicated in cases of asthma, diabetes, severe bradycardia, peripheral vascular disease and COPD Nitroglycerin is the cornerstone of angina therapy. Nitroglycerin, placed under the tongue, rapidly penetrates sublingual capillaries and induces vasodilation within minutes. Nitroglycerin is taken at the onset of anginal pain or prior to exertion to prevent anginal episodes. Calcium entry blockers reduce the frequency of anginal episodes and now play an important role in the management of patients’ prone to anginal episodes. Beta-adrenergic blockers suppress heart activity, thus lowering the oxygen requirements of myocardial cells; muscle is also responsible for propulsion in the GI tract. Inhibition of propulsion by calcium channel blockers causes constipation, a prevalent side effect of calcium channel blocker therapy. Cardiac muscle and conducting tissue rely on rapid influx of sodium and slow influx of calcium through separate channels for contraction. The slow calcium channel is particularly important in the SA and AV nodes. Blockade of these channels slows the heart. Skeletal muscle contraction is induced by rapid influx of sodium, which triggers the 51 release of calcium from the sarcoplasmic reticulum. Because these cells do not require extracellular calcium for contraction, calcium channel blockers fail to affect skeletal muscle. Direct vasodilators relax smooth muscle cells which surround blood vessels by a mechanism which is not yet clear, but likely involves production of nitric oxide by vascular endothelium. 3.2. ORGANIC NITRATES Nitrates are the drugs of choice for relieving angina because they decrease preload and myocardial oxygen demand by venous dilatation. In addition, nitrates dilate coronary arteries even in the setting of atherosclerosis. Mechanism of Action The two proposed mechanisms by which nitrates promote venodilatation are stimulation of cyclic guanosine monophosphate (GMP) production and inhibition of thromboxane synthetase. Nitrites, organic nitrates, nitroso compounds, and a variety of other nitrogen oxide-containing substances (including nitroprusside) lead to the formation of the reactive free radical NO. The exact mechanism(s) of denitration of the organic nitrates to liberate NO remains an active area of investigation. NO can activate guanylyl cyclase, increase the cellular level of cyclic GMP, activate PKG (the cyclic GMP-dependent protein kinase), and modulate the activities of cyclic nucleotide phosphodiesterases in a variety of cell types. In smooth muscle, the net result is reduced phosphorylation of myosin light chain, reduced Ca2+ concentration in the cytosol, and relaxation. NOTE: Effects of cGMP are terminated by phosphodiesterase enzymes. Sildenafil, vardenafil, and tadalafil are inhibitors of phosphodiesterase type 5 that are used to treat erectile dysfunction, because they potentiate NO actions in the corpora cavernosa of the penis by this mechanism. The combination of sildenafil and other phosphodiesterase type 5 (PDE5) inhibitors with organic nitrate vasodilators can cause extreme hypotension. 52 Short-acting nitrates, such as sublingual (SL) tablets or translingual sprays, are the preparation of choice for quick relief, especially in the setting of exertional angina. Long-acting nitrates (e.g., isosorbide dinitrate and isosorbide mononitrate) become useful when the number, severity, and duration of anginal attacks increase. Classification Nitroglycerin is the most important of the nitrates and is available in forms that provide a range of durations of action from 10–20 minutes (sublingual) to 8–10 hours (transdermal). Because treatment of acute attacks and prevention of attacks are both important aspects of therapy, the pharmacokinetics of these different dosage forms are clinically significant. Pharmacokinetics The time to onset of action varies from one minute for nitroglycerin to more than one hour for isosorbide mononitrate. Significant first-pass metabolism of nitroglycerin occurs in the liver. Therefore, it is common to give the drug either sublingually or via a transdermal patch. Mechanisms of Action The organic nitrates, such as nitroglycerin, are thought to relax vascular smooth muscle by their intracellular conversion to nitrite ions and then to nitric oxide (NO), which, in turn, activates guanylate cyclase and increases the cells' cyclic GMP. Elevated cGMP ultimately leads to dephosphorylation of the myosin light chain, resulting in vascular smooth muscle relaxation. Organ System Effects Effects on cardiovascular system: Smooth muscle relaxation leads to peripheral venodilation, which results in reduced cardiac size and cardiac output through reduced preload. Reduced after load, from arteriolar dilation, it may contribute to an increase in ejection and a further decrease in cardiac size. Some studies suggest that of the vascular beds; the veins are the most sensitive, arteries less so, and 53 arterioles least sensitive. Venodilation leads to decreased diastolic heart size and fiber tension. Arteriolar dilation leads to reduced peripheral resistance and blood pressure. These changes contribute to an overall reduction in myocardial fiber tension, oxygen consumption, and the double product. Thus, the primary therapy in atherosclerotic angina is reduction of the oxygen requirement. A secondary therapy – namely, an increase in coronary flow via collateral vessels in ischemic areas – has also been proposed in vasospastic angina; a reversal of coronary spasm and increased flow can be demonstrated. Nitrates have no direct effects on myocardium, but a significant reflex tachycardia and increased force of contraction are predictable when nitroglycerin reduces the blood pressure. Other Smooth Muscle Organs Relaxation of smooth muscle of the bronchi, gastrointestinal tract (including biliary system), and genitourinary tract has been demonstrated experimentally. Because of their brief duration, these actions of the nitrates are rarely of any clinical value. During recent years, the use of amyl nitrite and isobutyl nitrite by inhalation as purported recreational (sex-enhancing) drugs has become popular with some segments of the population. Nitrites release nitric oxide in erectile tissue as well as vascular smooth muscle and activate guanylyl cyclase. The resulting increase in cGMP causes dephosphorylation of myosin light chains and relaxation, which enhances erection. Clinical Uses As previously noted, nitroglycerin is available in several formulations. The standard form for treatment of acute anginal pain is the sublingual tablet, which has duration of action of 10-20 minutes. Oral (swallowed) normal-release nitroglycerin has duration of action of 4 – 6 hours. Sustained-release oral forms have a somewhat longer duration of action. Transdermal formulations (ointment or patch) can maintain blood levels. 54 Table 12 -Nitrate and nitrite drugs used in the angina treatment Drug Short-acting Nitroglycerin, sublingual Isosorbide dinitrate, sublingual Amyl nitrite, inhalant Long-acting Nitroglycerin, oral, sustained action Nitroglycerin, 2% ointment, transdermal Nitroglycerin, slowrelease, buccal Nitroglycerin, slowrelease patch, transdermal Dose Duration of action 0.15–1.2 mg 2.5–5 mg 10–30 minutes 10–60 minutes 0.18–0.3 mL 3–5 minutes 6.5–13 mg per6–8 hours 1–1.5 inches per 4 hours 1–2 mg per 4 hours 10–25 mg per 24 hours (one patch per day) Isosorbide dinitrate, 2.5–10 mg sublingual per 2 hours Isosorbide dinitrate, oral 10–60 mg per 4–6 hours Isosorbide dinitrate, 5–10 mg chewable oral per 2–4 hours Isosorbide mononitrate 20 mg oral per 12 hours 6–8 hours 3–6 hours 3–6 hours 8–10 hours 1.5–2 hours 4–6 hours 2–3 hours 6–10 hours Adverse Effects The most common adverse effect of nitroglycerin, as well as of the other nitrates, is a headache. Thirty to sixty percent of patients receiving intermittent nitrate therapy with long-acting agents develop headaches. High doses of organic nitrates can also cause postural hypotension, facial flushing, and refectory tachycardia. 55 Methemoglobinemia: Nitrite ion reacts with hemoglobin (which contains ferrous iron) to produce methemoglobin (which contains ferric iron). Because methemoglobin has a very low affinity for oxygen, large doses of nitrites can result in pseudocyanosis, tissue hypoxia, and death. Fortunately, the plasma level of nitrite, resulting from even larger doses of organic and inorganic nitrates, is too low to cause significant methemoglobinemia in adults. However, sodium nitrite is used as a curing agent for meats. In nursing infants, the intestinal flora is capable of converting significant amounts of inorganic nitrate, e.g., from well water, to nitrite ion. Thus, inadvertent exposure to large amounts of nitrite ion can occur and may produce serious toxicity. Methemoglobinemia, if excessive, can be treated by giving methylene blue intravenously. Glaucoma, once thought to be a contraindication, does not worsen, and nitrates can be used safely in the presence of increased intraocular pressure. Nitrates are contraindicated, however, if intracranial pressure is elevated. Tolerance: Tolerance to the actions of nitrates develops rapidly. It can be overcome by provision of a daily "nitrate-free interval" to restore sensitivity to the drug. This interval is typically 6 – 8 hours, usually at night because there is decreased demand on the heart at that time. Nitroglycerin patches are worn for 12 hours and removed for 12 hours. However, Prinzimetal's or variant angina worsens early in the morning, perhaps due to circadian catecholamine surges. These patients' nitrate-free interval should be late afternoon. With continuous exposure to nitrates, tolerance or the loss of antianginal and hemodynamic effects occurs. When exposure is discontinued, symptoms of withdrawal (severe headache, chest pain, or sudden cardiac death) can occur. Short-acting nitrates are not likely to lead to tolerance due to their rapid onset of action and short duration. Isosorbide dinitrate is an orally active nitrate. The drug is not readily metabolized by the liver or smooth muscle and has a lower potency than nitroglycerin in relaxing vascular smooth muscle. Nitric oxide released from nitroglycerin stimulates guanylyl cyclase in platelets as in smooth muscle. The increase in cGMP that 56 results is responsible for a decrease in platelet aggregation. Unfortunately, recent prospective trials have established no survival benefit when nitroglycerin is used in acute myocardial infarction. 3.3. MYOCARDIAL INFARCTION Myocardial infarction occurs when a coronary artery has been blocked by thrombus. This may be fatal and is a common cause of death, usually as a result of mechanical failure of the ventricle or from dysrhythmia. Cardiac myocytes rely on aerobic metabolism. If the supply of oxygen remains below a critical value, a sequence of events leading to cell death (by necrosis or apoptosis) ensues. The relative importance of necrosis and apoptosis in myocardial cell death in clinically distinct settings is unknown, but it has been suggested that apoptosis may be an adaptive process in hypoperfused regions, sacrificing some jeopardised myocytes but thereby avoiding the disturbance of membrane function and risk of dysrhythmia inherent in necrosis. Consequently, it is currently unknown if pharmacological approaches to promote or inhibit this pathway could be clinically beneficial. Prevention of irreversible ischaemic damage following an episode of coronary thrombosis is an important therapeutic aim. The main possibilities among existing therapeutic groops are: – thrombolytic and antiplatelet drugs (aspirin and clopidogrel) to open the blocked artery and prevent their reocclusion; – oxygen; – opioids to prevent pain and reduce excessive sympathetic activity; – β-adrenoceptor antagonists; – angiotensin-converting enzyme (ACE) inhibitors; The latter two classes of drugs reduce cardiac work and thereby the metabolic needs of the heart. The β-adrenoceptor antagonists have an important benefit during chronic treatment in reducing dysrhythmic deaths, and are widely used in patients with unstable angina; they increase the risk of cardiogenic shock if given during 57 acute infarction to patients with signs of heart failure, but are started as soon as is haemodynamically prudent. Several clinical trials have demonstrated that ACE inhibitors improve survival if given to patients shortly after myocardial infarction, especially if there is even a modest degree of myocardial dysfunction. It is possible that sartans could prove similarly beneficial. Despite several encouraging small trials of organic nitrates, a large randomised controlled trial (the Fourth International Study of Infarct Survival, ISIS-4, 1994) showed that these drugs do not improve outcome in patients with myocardial infarction, although they are useful in preventing or treating anginal pain. Calcium antagonists, which reduce cardiac work (via arteriolar vasodilatation and afterload reduction) and block Ca2+ entry into cardiac myocytes, have been disappointing, and several clinical trials of short-acting dihydropyridines (e.g., nifedipine ) were halted when adverse trends were evident. Trimetazidine, a 3-ketoacyl-CoA thiolase inhibitor, is believed to protect the heart from ischaemia by switching cardiac metabolism from fatty acid to glucose oxidation, but its place (if any) in therapeutics is yet to be established. 4. ANTIHYPERLIPEDEMIC DRUGS Coronary artery disease (CAD) is the cause of about half of all deaths in the world. CAD has been shown to be correlated with the levels of plasma cholesterol- and/or triacylglycerol-containing lipoprotein particles. These particles, which are the key to the development of atherogenesis, are initially synthesized by the intestinal mucosa and the liver, and undergo extensive metabolism in the plasma. They also play an essential role in the transport of lipids between tissues. Because lipids are insoluble in aqueous solutions, they must be transported in the plasma from tissue to tissue, bound to proteins, hence the name, lipoprotein. Their levels can be elevated by environmental causes, such as diet, or by inherited genetic defects in the appropriate synthesis or degradation of these compounds. Drugs used in the treatment of elevated serum lipids (hyperlipidemias) 58 generally are targeted to (1) decrease production of a lipoprotein by the tissues, (2) increase catabolism of a lipoprotein in the plasma, or (3) increase removal of cholesterol from the body. Such treatments lead to a decline in the progression of coronary plaque and a possible regression of pre-existing lesions. The main agents used clinically are: Statins: 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase inhibitors inhibit synthesis of cholesterol, increasing expression of low-density lipoprotein (LDL) receptors on hepatocytes and hence LDL cholesterol (LDL-C) uptake. Fibrates activate PPARα receptors, increase activity of lipoprotein lipase, decrease hepatic very low-density lipoprotein production, and enhance clearance of LDL-C by the liver. They markedly lower serum triglycerides and modestly increase high-density lipoprotein cholesterol. Adverse effects include muscle damage. Inhibitors of cholesterol absorption: Agents that interfere with cholesterol absorption, usually as an adjunct to diet plus statin: – ezetimibe; – stanol-enriched foods; – bile acid-binding resins (e.g., colestyramine). Nicotinic acid or its derivatives: Flushing is the main adverse effect. Essential phospholipids (Essenciale). Fish oil derivatives: Omega-3-acid ethyl esters. 4.1. PRINCIPLES OF TREATMENT IN ACCORDANCE WITH THE TYPES OF DYSLIPIDEMIA Before the start of correction of dyslipidemia, levels of different types of lipoproteins, chylomicrons, triacylglycerols and total cholesterol in patient’s blood must be examined. The doctor detects the type of dyslipidemia and only after that begins the treatment. The classification by Fredricsson is used more often in the word. Type I [familial hyperchylomicronemia]: 59 – Massive fasting hyperchylomicronemia even following normal dietary fat intake, resulting in greatly elevated serum triacylglycerol. – Deficiency of Ilpoprotein lipase or deficiency of normal apolipoprotein CII (rare). – Type I is not associated with an increase in coronary heart disease. – Treatment: Low fat diet. No drug therapy is effective for Type I hyperlipidemia. Type IIA [familial hypercholesterolemia]: – Elevated LDL with normal VLDL levels due to block in LDL degradation, therefore increased serum cholesterol but normal triacylglycerol. – Caused by decreased numbers of normal LDL receptors. – Ischemic heart disease is greatly accelerated. – Treatment: Low cholesterol and low saturated fat in the diet. Heterozygotes: Cholestyramine or colestipol, and/or, Iovastatin or mevastatin. Homozygofes: As above, plus niacin. Type IIb [familial combined (mixed) hyperlipidemia]: – Similar to IIA except VLDL are also increased, resulting in elevated serum triacylglycerol as well as cholesterol. – Caused by overproduction of VLDL by the liver. – Relatively common. – Treatment: dietary restriction of cholesterol and saturated fat and alcohol. Drug therapies similar to IIA except heterozygotes also to receive niacin. Type III [familial dysbetalipoproteinemia]: – Serum concentrations of IDL are increased resulting in increased triacylglycerol and cholesterol levels. – The cause is either overproduction or underutilization of IDL, due to mutant apelipeprotein E. 60 – Xanthomas and accelerated coronary and peripheral vascular disease develop in patients by middle age. – Treatment: weight reduction (if necessary). Dietary restriction of cholesterol and alcohol. Drug therapy includes niacin and clofibrate (or gemfibrozil), or lovastatin (or mevastatin). Type IV [familial hypertriglyceridemia]: – VLDL levels are increased, while LDL levels are normal or decreased, resulting in normal to elevated cholesterol and greatly elevated circulating triacylglycerol levels. – The cause is an overproduction and/or decreased removal of VLDL triacylglycerol in serum. – This is a relatively common disease. It has few clinical manifestations other than accelerated ischemic heart disease. Patients with this disorder are frequently obese, diabetic, and hyperuricemic. Also seen in individuals undergoing estrogen therapy, or are in their third trimester of pregnancy, or are alcoholic. – Treatment: weight reduction (if necessary) is of primary importance. Dietary restriction of controlled carbohydrate, modified fat, low alcohol consumption. If necessary, drug therapy includes niacin and/or gemfibrozil (or clofibrate), or lovastatin (or mevastatin). Type V [familial mixed hypertriglyceridemia]: – Serum VLDL and chylomicrons are elevated. LDL is normal or decreased. This results in elevated cholesterol and greatly elevated triacylglycerol levels. – The cause is either increased production or decreased clearance of VLDL and chylomicrons. Usually a genetic defect. – Occurs most commonly in adults who are obese and/or diabetic. – Treatment: weight reduction (if necessary) is important. Diet should include protein, low fat and controlled carbohydrate, and no 61 alcohol. If necessary, drug therapy includes niacin, clofibrate and/or gemfibrozil, or lovastatin (or mevastatin). The hyperlipidemias form a complex group of diseases that can be designated either primary or secondary, depending on their causes. Primary hyperlipidemias can result from a single inherited gene defect, or more commonly, are caused by a combination of genetic and environmental factors. Secondary, hyperlipidemias are the result of more generalized metabolic disorders, such as diabetes mellitus, excessive alcohol intake, hypothyroidism, or primary biliary cirrhosis. Therapeutic strategies for treating secondary hyperlipidemia caused by one of these disorders include dietary intervention plus a regimen of drugs used to treat the primary cause of the hyperlipidemia. 4.2. HMG CoA REDUCTASE INHIBITORS 3-Hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (commonly known as statins) lower elevated LDL cholesterol levels resulting in a substantial reduction in coronary events and death from CHD. This group of antihyperlipidemic agents inhibits the first committed enzymatic step of cholesterol synthesis, and they are the first-line and more effective treatment for patients with elevated LDL cholesterol. Therapeutic benefits include plaque stabilization, improvement of coronary endothelial function, inhibition of platelet thrombus formation, and anti-inflammatory activity. The value of lowering the level of cholesterol with statin drugs has now been demonstrated in 1) patients with CHD with or without hyperlipidemia, 2) men with hyperlipidemia but no known CHD, and 3) men and women with average total and LDL cholesterol levels and no known CHD. Inhibition of HMG-CoA reductase: lovastatin, simvastatin, pravastatin, atorvastatin, fluvastatin, and rosuvastatin are analogs of HMG, the precursor of cholesterol. Lovastatin and simvastatin are lactones that are hydrolyzed to the active drug. Pravastatin and fluvastatin are active as such. Because of their strong affinity for the enzyme, all compete effectively to inhibit HMG-CoA reductase, the 62 rate-limiting step in cholesterol synthesis. By inhibiting de novo cholesterol synthesis, they deplete the intracellular supply of cholesterol. Rosuvastatin and atorvastatin are the most potent LDL cholesterol lowering statin drugs, followed by simvastatin, pravastatin and then lovastatin and fluvastatin. Increase in LDL receptors: Depletion of intracellular cholesterol causes the cell to increase the number of specific cell-surface LDL receptors that can bind and internalize circulating LDLs. Thus, the end result is a reduction in plasma cholesterol, both by lowered cholesterol synthesis and by increased catabolism of LDL. Because these agents undergo a marked first-pass extraction by the liver, their dominant effect is on that organ. The HMG-CoA reductase inhibitors, like the bile acid sequestrant cholestyramine, can increase plasma HDL levels in some patients, resulting in an additional lowering of risk for CHD. Decreases in triglyceride also occur. Therapeutic uses: These drugs are effective in lowering plasma cholesterol levels in all types of hyperlipidemias. Indications are: – Primary prevention of arterial disease in patients who are at high risk because of elevated serum cholesterol concentration, especially if there are other risk factors for atherosclerosis. Tables (available for example in the British National Formulary) are used to target treatment to those at greatest risk. – Secondary prevention of myocardial infarction and stroke in patients who have symptomatic atherosclerotic disease (e.g., angina, transient ischaemic attacks, or following myocardial infarction or stroke). However, patients who are homozygous for familial hypercholesterolemia lack LDL receptors and, therefore, benefit much less from treatment with atorvastatin. Sometimes these drugs are often given in combination with other antihyperlipidemic drugs. It should be noted that in spite of the protection afforded by cholesterol lowering, about one-fourth of the patients treated with these drugs still present with coronary events. Thus, additional strategies, such as diet, exercise, or additional agents, may be warranted. 63 Pharmacokinetics: Pravastatin and fluvastatin are almost completely absorbed after oral administration; oral doses of lovastatin and simvastatin are from 30% to 50% absorbed. Similarly, pravastatin and fluvastatin are active as such, whereas lovastatin and simvastatin must be hydrolyzed to their acid forms. Due to first-pass extraction, the primary action of these drugs is on the liver. All are biotransformed, with some of the products retaining activity. Excretion takes place principally through the bile and feces, but some urinary elimination also occurs. Their half-lives range from 1.5 to 2 hours. Adverse Effects Statins are well tolerated; mild unwanted effects include myalgia, gastrointestinal disturbance, and raised concentrations of liver enzymes in plasma, insomnia and rash. Therefore, it is prudent to evaluate liver function and measure serum transaminase levels periodically. These return to normal on suspension of the drug. Hepatic insufficiency can cause drug accumulation. More serious adverse effects are rare but include severe myositis (rhabdomyolysis – disintegration or dissolution of muscle) and angio-oedema. Myositis is a class effect of statins, occurs also with other lipid-lowering drugs (especially fibrates) and is dose-related. It is more common in patients with small lean body mass or uncorrected hypothyroidism. It s very important to measure regularly serum creatine kinase levels. HGM-CoA reductase inhibitors are metabolized by the cytochrome P450 system; drugs or foods (e.g., grapefruit juice) that inhibit cytochrome P450 activity may increase the risk of epatotoxicity and myopathy. Because of evidence that the HMGCoA reductase inhibitors are teratogenic, these drugs should be avoided in pregnancy. Drug interactions: The HMG CoA reductase inhibitors may also increase warfarin levels. Thus, it is important to monitor INR times frequently. 64 Contraindications: These drugs are contraindicated during pregnancy and in nursing mothers. They should not be used in children or teenagers. 4.3. NIACIN (NICOTINIC ACID) Niacin is a water-soluble B-complex vitamin that functions as a vitamin only after its conversion to NAD or NADP, in which it occurs as an amide. Both niacin and its amide may be given orally as a source of niacin for its functions as a vitamin, but only niacin affects lipid levels. The hypolipidemic effects of niacin require larger doses than are required for its vitamin effects. Niacin can reduce LDL levels by 10–20% and is the most effective agent for increasing HDL levels. Niacin can be used in combination with statins, and a fixed-dose combination of lovastatin and long-acting niacin is available. Mechanism of Action Niacin inhibits VLDL secretion, in turn decreasing production of LDL. Increased clearance of VLDL via the LPL pathway contributes to triglyceride reduction. Niacin has no effect on bile acid production. Excretion of neutral sterols in the stool is increased acutely as cholesterol is mobilized from tissue pools and a new steady state is reached. The catabolic rate for HDL is decreased. Fibrinogen levels are reduced, and levels of tissue plasminogen activator appear to increase. Niacin inhibits the intracellular lipase of adipose tissue via receptor-mediated signaling, possibly reducing VLDL production by decreasing the flux of free fatty acids to liver. Sustained inhibition of lipolysis has not been established, however. Therapeutic uses: Niacin lowers plasma levels of both cholesterol and triacylglycerol. Therefore, it is particularly useful in the treatment of familial hyperlipidemias. Niacin is also used to treat other severe hypercholesterolemias, often in combination with other antihyperlipidemic agents. In addition, it is the most potent antihyperlipidemic agent for raising plasma HDL levels, which is the most common indication for its clinical use. 65 Pharmacokinetics: Niacin is administered orally. It is converted in the body to nicotinamide, which is incorporated into the cofactor nicotinamide-adenine dinucleotide (NAD+). Niacin, its nicotinamide derivative, and other metabolites are excreted in the urine. [Note: Nicotinamide alone does not decrease plasma lipid levels.] Adverse Effects Cutaneous flushing (accompanied by an uncomfortable feeling of warmth) and pruritus are common adverse effects. NSAIDs (aspirin) reduces the intensity of this flushing, suggesting that it is mediated by prostaglandin. Tolerance to the flushing reaction usually develops within a few days. Some patients also experience nausea and abdominal pain. It is a dose-dependent reaction. NA inhibits tubular secretion of uric acid and, thus, predisposes to hyperuricemia and gout. Hyperuricemia occurs in about 20% of patients, and carbohydrate tolerance may be moderately impaired. Impaired glucose tolerance and hepatotoxicity have also been repor. Moderate elevations of liver enzymes and even severe hepatotoxicity may occur. 4.4. FIBRIC ACID DERIVATIVES (FIBRATES) Fenofibrate and gemfibrozil are derivatives of fibric acid that lower serum triacylglycerols and increase HDL levels. Both have the same mechanism of action. However, fenofibrate is more effective than gemfibrozil in lowering plasma LDL cholesterol and triglyceride levels. Mechanism of Action They are agonists for a subset of lipid-controlled gene regulatory elements (PPARs4), PPARα, which are members of the superfamily of nuclear receptors; in humans, the main effects are to increase transcription of the genes for lipoprotein lipase, apoA1 and apoA5. They increase hepatic LDL-C uptake. In addition to effects on lipoproteins, fibrates reduce plasma C-reactive protein and fibrinogen, improve glucose tolerance, and inhibit vascular smooth 66 muscle inflammation by inhibiting the expression of the transcription factor NF-κB. As with the pleiotropic effects of statins (see above), there is great interest in these actions, although again it is unknown if they are clinically important. These drugs are useful in hypertriglyceridemias, in which VLDL predominate and in dysbetalipoproteinemia. They also may be of benefit in treating the hypertriglyceridemia that results from treatment with viral protease inhibitors. The dosage of fenofibrate is one to three 54 mg tablets (or a single 160 mg tablet) daily. Absorption of both drugs is improved when they are taken with food. Clinical Uses of Fibrates: – Mixed dyslipidaemia (i.e., raised serum triglyceride as well as cholesterol), provided this is not caused by excessive alcohol consumption. Fenofibrate is uricosuric, which may be useful where hyperuricaemia coexists with mixed dyslipidaemia. – In patients with low high-density lipoprotein and high risk of atheromatous disease (often type 2 diabetic patients). – Combined with other lipid-lowering drugs in patients with severe treatment-resistant dyslipidaemia. This may, however, increase the risk of rhabdomyolysis. Pharmacokinetics: Both drugs are completely absorbed after an oral dose. Gemfibrozil and fenofibrate distribute widely, bound to albumin. Both drugs undergo extensive biotransformation and are excreted in the urine as their glucuronide conjugates. Adverse Effects Gastrointestinal effects: The most common adverse effects are mild gastrointestinal disturbances. Gastrointestinal symptoms, pruritus and rash are more common than with statins. All of these lessen as the therapy progresses. Lithiasis: Because these drugs increase biliary cholesterol excretion, there is a predisposition to the formation of gallstones. Muscle: Myositis (inflammation of a voluntary muscle) can occur with both drugs; thus, muscle weakness or tenderness should be 67 evaluated. Myositis is unusual but can be severe (rhabdomyolysis) with myoglobinuria and acute renal failure. Myopathy and rhabdomyolysis have been reported in a few patients taking gemfibrozil and lovastatin together. Drug interactions: Both fibrates compete with the coumarin anticoagulants for binding sites on plasma proteins, thus transiently potentiating anticoagulant activity. INR times should therefore be monitored when a patient is taking both drugs. Similarly, these drugs may transiently elevate the levels of sulfonylureas. Contraindications: The safety of these agents in women during pregnancy or lactation has not been established. They should not be used in patients with severe hepatic and renal dysfunction or in patients with preexisting gallbladder disease. 4.5. BILE ACID BINDING RESINS Bile acid sequestrants (resins) have significant LDL cholesterol lowering effects, although the benefits are less than those observed with statins. Mechanism of Action Cholestyramine, colestipol, and colesevelam are anion-exchange resins that bind negatively charged bile acids and bile salts in the small intestine. The resin/bile acid complex is excreted in the feces, thus preventing the bile acids from returning to the liver by the enterohepatic circulation. Lowering the bile acid concentration causes hepatocytes to increase conversion of cholesterol to bile acids, resulting in a replenished supply of these compounds, which are essential components of the bile. Consequently, the intracellular cholesterol concentration decreases, which activates an increased hepatic uptake of cholesterol-containing LDL particles leading to a fall in plasma LDL. This increased uptake is mediated by an upregulation of cell-surface LDL receptors. In some patients, a modest rise in plasma HDL levels is also observed. The final outcome of this sequence of events is a decreased total plasma cholesterol concentration. 68 Pharmacokinetics: Cholestyramine, colestipol, and colesevelam are taken orally. Because they are insoluble in water and are very large (molecular weights are greater than 106), they are neither absorbed nor metabolically altered by the intestine. Instead, they are totally excreted in the feces. Therapeutic uses: The bile acid binding resins are the drugs of choice (often in combination with diet or niacin) in treating Type IIa and Type IIb hyperlipidemias. Cholestyramine can also relieve pruritus caused by accumulation of bile acids in patients with biliary obstruction. Adverse Effects The most common side effects are gastrointestinal disturbances, such as constipation, nausea, and flatulence. Colesevelam has fewer gastrointestinal side effects than other bile acid sequestrants. Impaired absorptions: At high doses, cholestyramine and colestipol (but not colesevelam) impair the absorption of the fatsoluble vitamins (A, D, E, and K). Drug interactions: Cholestyramine and colestipol interfere with the intestinal absorption of many drugs, for example, tetracycline, phenobarbital, digoxin, warfarin, pravastatin, fluvastatin, aspirin, and thiazide diuretics. Therefore, drugs should be taken at least 1-2 hours before, or 4-6 hours after the bile acid binding resins. 4.6. CHOLESTEROL ABSORPTION INHIBITORS Ezetimibe selectively inhibits intestinal absorption of dietary and biliary cholesterol in the small intestine, leading to a decrease in the delivery of intestinal cholesterol to the liver. This causes a reduction of hepatic cholesterol stores and an increase in clearance of cholesterol from the blood. Ezetimibe lowers LDL cholesterol by 17% and triacylglycerols by 6 %, and it increases HDL cholesterol by 1.3%. Ezetimibe is primarily metabolized in the small intestine and the liver via glucuronide conjugation (a Phase II reaction), with subsequent biliary and renal excretion. Both ezetimibe and ezetimibe-glucuronide are slowly eliminated from plasma, with a 69 half-life of approximately 22 hours. Ezetimibe has no clinically meaningful effect on the plasma concentrations of the fat-soluble vitamins A, D, and E. Patients with moderate to severe hepatic insufficiency should not be treated with ezetimibe. Adverse Effects GIT effects: The most common side effects are gastrointestinal disturbances, such as constipation, nausea, and flatulence. Impaired absorptions: Absorption of the fat-soluble vitamins, A, D, E, and K can be impaired if high doses of the resin are present. Folic acid and ascorbic acid absorption may also be reduced. Drug interactions: Cholestyramine and colestipol interfere with the intestinal absorption of many drugs, for example, tetracycline, phenobarbital digoxin, warfarin, pravastatin, fluvastatin, aspirin, and thiazide diuretics. Therefore, drugs should be taken at least 1–2 hours before, or 4–6 hours after the bile acid binding resins. 4.7. COMBINATION DRUG THERAPY It is often necessary to employ two antihyperlipidemic drugs to achieve treatment goals in plasma lipid levels. For example, in Type II hyperlipidemias, patients are commonly treated with a combination of niacin plus a bile acidв binding agent, such as cholestyramine. Table 12 - Principles of correction of hyperlipedemias . Drugs Therapy level I Lovastatin Simvastatin Fenofibrate Cyprofibrate Cholesteramine + + + + + II + + Primary Severe ↓Choleste- ↓Cholestehyperlipi- hyperlipirol rol demia demia absorption synthesis + + + + + + + + + + + + 70 Cholestyramine causes an increase in LDL receptors that clears the plasma of circulating LDL, whereas niacin decreases synthesis of VLDL and, therefore, also the synthesis of LDL. The combination of an HMG-CoA reductase inhibitor with a bile acid binding agent has also been shown to be very useful in lowering LDL cholesterol levels. A low-dose statin in combination with ezetimibe achieves comparable or even greater LDL cholesterol reduction than a veryhigh-dose statin. Simvastatin and ezetimibe are currently available combined in one pill to treat elevated LDL cholesterol. 5. DRUGS FOR ASTHMA OR COPD TREATMENT Asthma is the commonest chronic disease characterized by hyperresponsive airways. It is increasing in prevalence and severity. It is a specific (allergic) inflammatory condition in which there is recurrent reversible airway obstruction in response to irritant stimuli that are too weak to affect non-asthmatic subjects. The obstruction usually causes wheeze and merits drug treatment, although the natural history of asthma includes spontaneous remissions. Reversibility of airways obstruction in asthma contrasts with COPD, where the obstruction is either not reversible or at best incompletely reversible, by bronchodilators. Bronchoconstriction, inflammation (increasing mucous secretion) and loss of lung elasticity are the three most common processes that result in bronchial obstruction. Therapy for obstructive lung disease is aimed at preventing or reversing these processes. Bronchoconstriction is the result of the effects of acetylcholine, histamine, and inflammatory mediators released within the bronchial walls. The vagus nerve releases acetylcholine in response to stimulation of upper airway mucosa by irritants. As a result, acetylcholine also triggers release of pulmonary secretions which further reduce air flow by plugging airways. Adrenergic agonists, cholinergic antagonists, methylxanthines and corticosteroids relax smooth muscles of small bronchi. Spasmolitics can be given for this indication too. Chronic inflammation is caused by prolonged 71 exposure to airway irritants such as pollution and cigarette smoke. Bronchiolar inflammation results in narrowed airways, increased secretions, epithelial proliferation, loss of ciliated epithelium and fibrosis. Corticosteroids inhibit the inflammatory response and decrease immunological system, but their use is at the expense of systemic side effects. Loss of lung elasticity results in terminal bronchiole enlargement, changes in lung compliance and the collapse of airways which are normally tethered open by surrounding lung tissue. Specific therapy to reverse or prevent proteolytic destruction of lungs is not readily available. For diagnostic and treatment purposes, obstructive lung disease is subclassified as either reactive airway disease or chronic obstructive lung disease (COPD). In practice, it is often difficult to distinguish these two diseases on the basis of pathophysiology or clinical course. Reactive airway disease (RAD, asthma): The trachea and bronchi of patients with reactive airway disease are particularly sensitive to stimulants, such as cigarette smoke, dust, cold air, and allergens. Patients present with wheezing, coughing and chest tightness. Decreased oxygenation of the lungs secondary to tracheobronchial constriction, mucus production, inflammation and edema cause these symptoms. 5.1. GENERAL PRINCIPLES IN THE TREATMENT OF BRONCHIAL OBSTRUCTIVE SYNDROME There are two categories of antiasthma drugs: bronchodilators and anti-inflammatory agents. The main drugs used as bronchodilators are β2-adrenoceptor agonists; others include xanthines, cysteinyl leukotriene receptor antagonists and muscarinic receptor antagonists. The method of treatment depends on the severity of the attack and the patient's response to previous therapy. Selective agents are preferred to nonselective β-blockers because they are less likely to cause tachycardia (mediated by βl-receptors). – Methylxanthines increase cAMP and inhibit adenosine-induced bronchoconstriction. Oral theophylline is used for outpatient management of asthma. 72 – An intravenous bolus of aminophylline, the watersoluble salt of theophylline, produces therapeutic serum levels faster than oral theophylline. Aminophyline is therefore used in acute management. – Cholinergic antagonists block bronchoconstriction caused by parasympathetic transmission. Ipratroprium bromide is a drug of choice for the treatment of non-asthmatic COPD in adults and is a secondary drug in the treatment of asthma. – Corticosteroids decrease peribronchial inflammation. Corticosteroids «bursts» (high doses for a few days) are sometimes used when adrenergic antagonists and theophylline fail to control asthma. The benefits of steroids must be balanced against their considerable toxicity if they are to be administered chronically at high doses. – Cromolyn is a prophylactic agent. It inhibits the release of mediators from inflammatory cells, such as mast cells. It is used exclusively in asthma. Most of these agents are administered by inhalation. With thoughtful teaching, asthmatic patients become proficient at delivering their own medication. Consider improper administration of bronchodilators as an explanation for therapeutic failure. 5.2. ADRENOMIMETICS Beta-adrenergiс agonists bind to β2 receptors on bronchial smooth muscle, causing an increase in the biochemical messenger, cyclic AMP (cAMP). Increased levels of cAMP cause relaxation of bronchial muscle cells, resulting in bronchodilation. They also inhibit mediator release from mast cells and TNF-α release from monocytes and increase mucus clearance by an action on cilia. These drugs are usually given by inhalation of aerosol (metered-dose inhaler), powder or nebulised solution, but some may be given orally or by injection. Classification: Two categories of β2-adrenoceptor agonists are used in asthma: 73 Short-acting agents: salbutamol and terbutaline. These drugs are given by inhalation; the maximum effect occurs within 30 minutes and the duration of action is 3–5 hours; they are usually used on an 'as needed' basis to control symptoms. Longer-acting agents, e.g., salmeterol and formoterol are given by inhalation, and the duration of action is 8–12 hours. They are not used “as needed” but are given regularly, twice daily, as adjunctive therapy in patients whose asthma is inadequately controlled by glucocorticoids. They act as physiological antagonists of the spasmogenic mediators but have little or no effect on the bronchial hyperreactivity. Adverse Effects At higher doses, therefore, these drugs may lead to increased heart rate, cardiac arrhythmias, and central nervous system (CNS) effects associated with adrenergic receptor activation such as tachycardia, hyperglycemia, hypokalemia, and hypomagnesemia are minimized with dosing via inhalation versus systemic routes. Although tolerance to the effects of β2 agonists on non-airway tissues occurs, it is uncommon with normal dosages. All patients with asthma should be prescribed a quick-relief inhaler and regularly assessed for appropriate inhaler technique. 5.3. ANTIMUSCARINIC AGENTS Interest in the potential value of antimuscarinic agents increased with demonstration of the importance of the vagus nerves in bronchospastic responses of laboratory animals and by the development of a potent atropine analog that is poorly absorbed after aerosol administration and that is therefore relatively free of systemic atropine-like effects. Its effectivness is less than that of adrenergic agents. 74 Mechanism of Action In the airways, acetylcholine is released from efferent endings of the vagus nerves, and muscarinic antagonists block the contraction of airway smooth muscle and the increase in secretion of mucus that occurs in response to vagal activity. Very high concentrations well above those achieved even with maximal therapy are required to inhibit the response of airway smooth muscle to nonmuscarinic stimulation. This selectivity of muscarinic antagonists accounts for their usefulness as investigative tools in examining the role of parasympathetic pathways in bronchomotor responses but limits their usefulness in preventing bronchospasm. In the doses given, antimuscarinic agents inhibit only that portion of the response mediated by muscarinic receptors, which varies by stimulus, and which further appears to vary among individuals in responses to the same stimulus. Antimuscarinic agents are effective bronchodilators. When given intravenously, atropine, the prototypical muscarinic antagonist, causes bronchodilation at a lower dose than that needed to cause an increase in heart rate. The selectivity of atropine's effect can be increased further by administering the drug by inhalation or by use of a more selective quaternary ammonium derivative of atropine, ipratropium bromide. Ipratropium can be delivered in high doses by this route because it is poorly absorbed into the circulation and does not readily enter the central nervous system. Studies with this agent have shown that the degree of involvement of parasympathetic pathways in bronchomotor responses varies among subjects. In some, bronchoconstriction is inhibited effectively; in others - only modestly. The failure of higher doses of the muscarinic antagonist to further inhibit the response in these individuals indicates that mechanisms other than parasympathetic reflex pathways must be involved. Ipratropium appears to be at least as effective in patients with COPD that includes a partially reversible component. A longeracting, selective antimuscarinic agent, tiotropium, is approved as a treatment for COPD. This drug is also taken by inhalation, and a single dose of 18 mcg has 24-hour duration of action. Daily 75 inhalation of tiotropium has been shown not only to improve functional capacity of patients with COPD, but also to reduce the frequency of exacerbations of their condition. Adverse Effects Ipratropium is virtually devoid of the CNS side effects associated with atropine.The most prevalent peripheral side effects are dry mouth, headache, nervousness, dizziness, nausea, and cough. Unlike atropine, ipratropiumdoes does not inhibit mucociliary clearance and thus does not promote the accumulation of secretions in the lower airways. 5.4. CORTICOSTEROIDS Mechanism of Action There are many effects of corticosteroids than have been used to treat asthma. More important are its anti-inflammatory efficacy, mediated in part by inhibition of production of inflammatory cytokines and bronchodilatating action. They do not relax airway smooth muscle directly but reduce bronchial reactivity and reduce the frequency of asthma exacerbations if taken regularly. Their effect on airway obstruction may be due in part to their contraction of engorged vessels in the bronchial mucosa and their potentiation of the effects of β-receptor agonists, but their most important action is inhibition of the lymphocytic eosinophilic mucosal inflammation of asthmatic airways. Clinical studies of corticosteroids consistently show them to be effective in improving all indices of asthma control severity of symptoms, tests of airway caliber and bronchial reactivity, frequency of exacerbations, and quality of life. Urgent treatment is often begun with an oral dose of 30–60 mg prednisone per day or an intravenous dose of 1 mg/kg methylprednisolone every 6 hours; the daily dose is decreased after airway obstruction has improved. In most patients, systemic corticosteroid therapy can be discontinued in a week or 10 days, but in other patients symptoms may worsen as the dose is decreased to lower levels. Because adrenal suppression by 76 corticosteroids is related to dose and because secretion of endogenous corticosteroids has a diurnal variation, it is customary to administer corticosteroids early in the morning after endogenous ACTH secretion has peaked. For prevention of nocturnal asthma, however, oral or inhaled corticosteroids are most effective when given in the late afternoon. Because of severe adverse effects when given chronically, oral and parenteral corticosteroids are reserved for patients who require urgent treatment, ie, those who have not improved adequately with bronchodilators or who experience worsening symptoms despite maintenance therapy. Regular or "controller" therapy is maintained with aerosol corticosteroids. Adverse Effects Aerosol treatment is the most effective way to avoid the systemic adverse effects of corticosteroid therapy. The introduction of corticosteroids such as beclomethasone, budesonide, flunisolide, fluticasone, mometasone, and triamcinolone has made it possible to deliver corticosteroids to the airways with minimal systemic absorption. Although these high doses of inhaled steroids may cause adrenal suppression, the risks of systemic toxicity from chronic use appear negligible compared with those of the oral corticosteroid therapy they replace. A special problem caused by inhaled topical corticosteroids is the occurrence of oropharyngeal candidiasis. The risk of this complication can be reduced by having patients gargle water and spit after each inhaled treatment. A novel approach to minimizing the risk of toxicity from systemic absorption of an inhaled corticosteroid underlays the development of ciclesonide. This investigational corticosteroid is inhaled as a prodrug activated by cleavage by esterases in bronchial epithelial cells. When absorbed into the circulation, the active product is tightly bound to serum proteins, and so has little access to glucocorticoid receptors in skin, eye, and bone, minimizing its risk of causing cutaneous thinning, cataracts, osteoporosis, or temporary slowing of growth. 77 Chronic use of inhaled corticosteroids effectively reduces symptoms and improves pulmonary function in patients with mild asthma. Such use also reduces or eliminates the need for oral corticosteroids in patients with more severe disease. In contrast to β-stimulant agents and theophylline, chronic use of inhaled corticosteroids reduces bronchial reactivity. Because of the efficacy and safety of inhaled corticosteroids, they are now routinely prescribed for patients who require more than occasional inhalations of a β agonist for relief of symptoms. This therapy is continued for 10-12 weeks and then withdrawn to determine whether more prolonged therapy is needed. Inhaled corticosteroids are not curative. In most patients, the manifestations of asthma return within a few weeks after stopping therapy even if they have been taken in high doses for 2 years or longer. 5.5. MAST CELL STABILIZERS As other anti-inflammatory agents, the cell membrane stabilizers can be used. Cromolyn sodium (disodium cromoglycate) and nedocromil sodium are stable but extremely insoluble salts. When used as aerosols (by nebulizer or metered-dose inhaler), they effectively inhibit both antigen- and exercise-induced asthma, and chronic use (four times daily) slightly reduces the overall level of bronchial reactivity. However, these drugs have no effect on airway smooth muscle tone and are ineffective in reversing asthmatic bronchospasm; they are only of value when taken prophylactically. Cromolyn sodium and nedocromil sodium are used almost exclusively for the prophylactic treatment of mild to moderate asthma and should not be used to control acute bronchospasm. Adverse Effects Cromolyn sodium and nedocromil sodium are the least toxic of available therapies for asthma. Adverse reactions are rare and generally minor and include transient bronchospasm, cough or wheezing, dryness of throat, laryngeal edema, swollen parotid gland, 78 angioedema, joint swelling and pain, dizziness, dysuria, nausea, headache, nasal congestion, rash, and urticaria. 5.6. LEUKOTRIENE MODULATORS Zafirlukast and montelukast are cysteinyl leukotriene (CysLT) receptor antagonists, and zileuton is a leukotriene synthesis inhibitor. CysLTs include leukotrienes C4, D4, and E4. These mediators are products of arachidonic acid metabolism and make up the components of slow reacting substance of anaphylaxis. Montelukast and zafirlukast are competitive antagonists of these receptors. In contrast, zileuton suppresses synthesis of the leukotrienes by inhibiting 5-lipoxygenase, a key enzyme in the bioconversion of arachidonic acid to the leukotrienes. Zileuton also blocks the production of leukotriene B4, another arachidonic acid metabolite with proinflammatory activity. Montelukast, zafirlukast, and zileuton are prescribed for the prophylaxis and treatment of chronic asthma, but not in treating attacks of asthma. All these drugs are administered orally. Adverce Effects Liver transaminase levels may be elevated sometimes. Zileuton inhibits the metabolism of theophylline. Dyspepsia is the most common side effect of zileuton. Zafirlukast and montelukast are well tolerated. 5.7. METHYLXANTINE DRUGS Methylxanthines increase cAMP and inhibit adenosine-induced bronchoconstriction. Oral theophylline is used for outpatient management of asthma. An intravenous bolus of aminophylline, the watersoluble salt of theophylline, produces therapeutic serum levels faster than oral theophylline. Aminophyline is therefore used in acute management. The three important methylxanthines are theophylline, theobromine, and caffeine. Their major source is beverages (tea, 79 cocoa, and coffee, respectively). The importance of theophylline as a therapeutic agent in the treatment of asthma has waned as the greater effectiveness of inhaled adrenoceptor agents for acute asthma and of inhaled anti-inflammatory agents for chronic asthma has been established, but theophylline's very low cost is an important advantage for economically disadvantaged patients in societies in which health care resources are limited. 6. GENERAL THERAPY PRINCIPLES OF ANTIMICROBIAL Antibacterial drugs can either kill infecting organism (bacteriacidal) or slow their growth (bacteriostatic), depending on many factors, including the specific drugs and dosage, the particular microorganism, and tissue location of the infection. Classification and Mechanism of Action Antimicrobial agents are classified based on chemical structure and proposed mechanism of action as follows: 1) agents that inhibit synthesis of bacterial cell walls, including the β-lactam class (e.g., penicillins, cephalosporins, and carbapenems) and dissimilar agents, such as cycloserine, vancomycin, and bacitracin; 2) agents that act directly on the cell membrane of the microorganism, increasing permeability and leading to leakage of intracellular compounds, including detergents, such as polymyxin, polyene antifungal agents (e.g., nystatin and amphotericin B) which bind to cell-wall sterols, and the lipopeptide daptomycin; 3) agents that disrupt function of 30S or 50S ribosomal subunits to reversibly inhibit protein synthesis, which generally are bacteriostatic (e.g., chloramphenicol, tetracyclines, erythromycin, clindamycin, streptogramins, and linezolid); 4) agents that bind to the 30S ribosomal subunit and alter protein synthesis, which generally are bactericidal (e.g., the aminoglycosides); 80 5) agents that affect bacterial nucleic acid metabolism, such as the rifamycins (e.g., rifampin and rifabutin), which inhibit RNA polymerase, and the quinolones, which inhibit topoisomerases; 6) the antimetabolites, including trimethoprim and the sulfonamides, which block essential enzymes of folate metabolism. 6.1. BETA-LACTAM COMPOUNDS AND OTHER CELL WALL INHIBITORS PENICILLINS The penicillins are classified as β-lactam drugs because of their unique four-membered lactam ring. They share features of chemistry, mechanism of action, pharmacological and clinical effects, and immunologic characteristics with cephalosporins, monobactams, carbapenems, and β-lactamase inhibitors, which also are β-lactam compounds. These drugs have the greatest activity against gram-positive organisms, Gram-negative cocci, and non-β-lactamase-producing anaerobes. However, they have little activity against Gram-negative rods. They are susceptible to hydrolysis by β lactamases. Antistaphylococcal penicillins: These penicillins are resistant to staphylococcal β-lactamases. They are active against staphylococci and streptococci but inactive against enterococci, anaerobic bacteria, and Gram-negative cocci and rods. These drugs retain the antibacterial spectrum of penicillin and have improved activity against Gram-negative organisms, but they are destroyed by β lactamases. Methicillin, nafcillin, oxacillin and dicloxacillin are penicillinase-resistant penicillins. Their use is restricted to the treatment of infections caused by penicillinase-producing staphylococci. Methicillin resistant Staphyilococcus aureus (MRSA) is currently a serious source of nosocomial (hospital-acquired) infections. This organism is usually susceptible to vancomycin and, rarely, to ciprofloxacin or rifampin. Extended-spectrum penicillins: Ampicillin and amoxicillin have an antibacterial spectrum similar to that of penicillin G, but are more effective against Gram-negative bacilli. They are therefore referred 81 to as extended-spectrum penicillins. Ampicillin is the drug of choice for the Gram-positive bacillus Listeria monocytogenes. These agents are also widely used in the treatment of respiratory infections, and amoxicillin is employed prophylactically by dentists for patients with abnormal heart valves who are to undergo extensive oral surgery. Resistance to these antibiotics is now a major clinical problem because of inactivation by plasmid-mediated penicillinase. Formulation with a β-lactamase inhibitor, such as clavulanic acid or sulbactam, protects amoxicillin or ampicillin, respectively, from enzymatic hydrolysis and extends their antimicrobial spectrum. Antipseudomonal penicillins: Carbenicillin, ticarcillin, and piperacillin are called antipseudomonal penicillins because of their activity against Pseudomonas aeruginosa. Piperacillin is the most potent. These antibiotics are effective against many Gram-negative bacilli but not against Klebsiella, because of its constitutive penicillinase. Formulation of ticarcillin or piperacillin with clavulanic acid or tazobactam, respectively, extends the antimicrobial spectrum of these antibiotics to include penicillinase-producing organisms. Mezlocillin and azlocillin (sometimes referred to as acylureido penicillins) are also effective against Pseudomonas aeruginosa, and a large number of Gram-negative organisms. They are susceptible to β-lactamase breakdown. Penicillins, like all β-lactam antibiotics, inhibit bacterial growth by interfering with a specific step in bacterial cell wall synthesis. Adverse Reactions Penicillins are among the safest drugs, and blood levels are not monitored, although adverse reactions do occur. 1. Hypersensitivity: This is the most important adverse effect of the penicillins. The major antigenic determinant of penicillin hypersensitivity is its metabolite, penicilloic acid, which reacts with proteins and serves as a hapten to cause an immune reaction. Approximately 5% of patients have some kind of reaction, ranging from maculopapular rash to angioedema (marked swelling of lips, tongue, and periorbital area) and anaphylaxis. Cross-allergic reactions do occur among the 13-1actam antibiotics. Although rashes 82 can develop with all the penicillins, maculopapular rashes are most common with ampicillin. Among patients with mononucleosis who are treated with ampicillin, the incidence of maculopapular rash approaches 100%. 2. Diarrhea: This effect, which is caused by a disruption of the normal balance of intestinal microorganisms, is a common problem. It occurs to a greater extent with those agents that are incompletely absorbed and have an extended antibacterial spectrum. 3. Nephritis: All penicillins, but particularly methicillin, have the potential to cause acute interstitial nephritis. 4. Neurotoxicity: The penicillins are irritating to neuronal tissue and can provoke seizures if injected intrathecally or if very high blood levels are reached. Epileptic patients are especially at risk. 5. Platelet dysfunction: This side effect, which involves decreased agglutination, is observed with the antipseudomonal penicillins (carbenicillin and ticarcillin) and, to some extent, with penicillin G. It is generally a concern when treating patients predisposed to hemorrhage or those receiving anticoagulants. 6. Cation toxicity: Penicillins are generally administered as the sodium or potassium salt. Toxicities may be caused by the large quantities of sodium or potassium that accompany the penicillin. Sodium excess may result in hypokalemia. This can be avoided by using the most potent antibiotic, which permits lower doses of drug and accompanying cations. CEPHALOSPORINS AND CEPHAMYCINS Cephalosporins and cephamycins are similar to penicillins chemically, in mechanism of action, and in toxicity. Cephalosporins are more stable than penicillins to produced by some bacteria βlactamases and therefore usually have a broader spectrum of activity. Cephalosporins are not active against enterococci and Listeria monocytogenes. Cephalosporins can be classified into four major groups or generations, depending mainly on the spectrum of antimicrobial activity. As a general rule, first-generation compounds have better 83 activity against Gram-positive organisms, and the later compounds exhibit improved activity against Gram-negative aerobic organisms. Classification First generation – narrow spectrum, sensitive to β-lactamases: cephalexin (Keflex), cefazolin (Kefzol), cephalothin (Keflin), cephradine (Anspor), cephadroxil (Duricef), cephaprin (Cephadyl). Cephalexin, cephradine and cefadroxil are administered orally, others IV/IM. Oral drugs reach therapeutic levels in urine but not serum. They all fail to penetrate into the CNS. They all are destroyed by β-lactamases, but may be administered with clavulinate to circumvent this problem: metabolized by liver, excreted by kidney. E Effective against most Staphylococcal and Streptococcal species that do not produce β-lactamases, they cover most strains of enteric Gram-negatives (E. coil, Proteus, Klebsiella) and some anaerobes perioperatively to reduce risk of surgical infections. Cephalexin and cefadroxil are often used for urinary tract infections. Second generation - increased activity against Gram-negatives: cefaclor (Ceclor), cefuroxime (Zinacef), cephamandole (Mandol), efoxitin (Mefoxin), cefotetan (Cefotan), cefonicid (Monocid), ceforanide (Precef), cefmetazole (Zefazone). Cefaclor and cefuroxime are administered orally; cefuroxime is administered also IV/IM. Others are administered IV/IM only. Cefuroxime enters CSF in concentrations suitable for the treatment of meningitis, others do not. Cefuroxime is also used as monotherapy for Gram-positive cocci and H. influenzae infections in infants and small children. It has increased activity against Gram-negatives (including H. influenza) but not effective for Pseudomonas aeruginosa or B. fragilis (except cefoxitin, which has good activity against B. fragilis), slightly less effective for treating Gram-positive infections than first generation agents, not drugs of choice for any infections. Cefoxitin, cefotetan, and cefmetazole are used primarily for abdominal and pelvic infections. Third generation - broad spectrum, resistant to most cephalosporins: cefotaxime (Claforan), ceftriaxone (Rocephin), 84 cefixime (Suprax), ocftizoxime (Cefizox), cefoperazone (Cefobid), moxalactam (Moxam), ceftazidime (Fortaz). Cefixime is precribed PO, others – IV/IM. Good CNS penetration (except cefoperazone). Ceftriaxone has the longest half-life. This generation is the most effective against Gram-negatives but is less effective against S. aureus than first or second generation drugs. They are not well suited for pseudomonal infections, although ceftazidime may be effective. Moxolactam is used less frequently than the others because it is associated with hemorrhagic side effects and is less effective against Gram-positive cocci. Fourth generation - Cefepime (Maxipim), cefirom (Keyten), cefelidine, and Cefoselis. Cefepime is the most clinically useful fourth generation cephalosporin and must be administered parenterally. Cefepime has a wide antibacterial spectrum being active against Streptococci and Staphylococci (only those that are methicillin susceptible). It is also effective against aerobic Gramnegative organisms, such as Enterobacter, Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis. Adverse Effects The cephalosporins produce a number of adverse affects, some of which are unique to particular members of the group. Allergic manifestations: The cephalosporins should be avoided or used with caution in individuals allergic to penicillins (about 5–15% show cross-sensitivity). In contrast, the incidence of allergic reactions to cephalosporins is 1–2% in patients without a history of allergy to penicillins. A Disulfiram-like effect: When cefamandole or cefoperazone is ingested with alcohol or alcohol-containing medications, a disulfiram-like effect is seen, because these cephalosporins block the second step in alcohol oxidation, which results in the accumulation of acetaldehyde 1. Bleeding: Bleeding can occur with cefamandole or cefoperazone, because of antivitamin K effects; administration of the vitamin corrects the problem. 85 MONOBACTAMS These are drugs with a monocyclic β-lactam ring. They are relatively resistant to lactamases and active against Gram-negative rods (including pseudomonas and serratia). They are not active against Gram-positive bacteria or anaerobes. Aztreonam resembles aminoglycosides in its spectrum of activity. Aztreonam is given intravenously every 8 hours in a dose of 1–2 g, providing peak serum levels of 100 g/mL. The half-life is 1–2 hours and is greatly prolonged in renal failure. Adverse Effects Aztreonam is relatively nontoxic, but it may cause phlebitis, skin rash, and occasionally, abnormal liver function tests. Aztreonam has a low immunogenic potential and shows little cross-reactivity with antibodies induced by other β-lactams. Thus, aztreonam may offer a safe alternative for treating patients allergic to penicillins and/or cephalosporins. BETA-LACTAMASE INHIBITORS (Clavulanic Acid, Sulbactam, and Tazobactam) These substances resemble β-lactam molecules but have very weak antibacterial action. They are potent inhibitors of many but not all bacterial lactamases and can protect hydrolyzable penicillins from inactivation by these enzymes. Beta-lactamase inhibitors are most active against the Ambler class A β-lactamases, such as those produced by staphylococci, H. influenzae, N. gonorrhoeae, salmonella, shigella, E. coli, and K pneumoniae. They are not good inhibitors of class C β-lactamases, which typically are chromosomally encoded and inducible, produced by enterobacter, citrobacter, serratia, and pseudomonas, but they do inhibit chromosomal β-lactamases of legionella, bacteroides, and branhamella. The indications for penicillin-β-lactamase inhibitor combinations are empirical therapy for infections caused by a wide range of potential pathogens in both immunocompromised and immunocompetent patients and treatment of mixed aerobic and 86 anaerobic infections, such as intra-abdominal infections. Doses are the same as those used for the single agents except that the recommended dosage of piperacillin in the piperacillin-tazobactam combination is 3 g every 6 hours. This is less than the recommended 3–4 g every 4–6 hours for piperacillin alone, raising concerns about the use of the combination for treatment of suspected pseudomonal infection. Adjustments for renal insufficiency are made based on the penicillin component. A) CARBAPENEMS The carbapenems (ertapenem, imipenem, and meropenem) are structurally related to β-lactam antibiotics. Imipenem has a wide spectrum with good activity against many Gram-negative rods, including Pseudomonas aeruginosa, Gram-positive organisms, and anaerobes. It is resistant to most β-lactamases but not metallo-βlactamases. Enterococcus faecium, methicillin-resistant strains of staphylococci, Clostridium difficile, Burkholderia cepacia, and Stenotrophomonas maltophilia are resistant. Imipenem is inactivated by dehydropeptidases in renal tubules, resulting in low urinary concentrations. Consequently, it is administered together with an inhibitor of renal dehydropeptidase, cilastatin, for clinical use. Meropenem is similar to imipenem but has slightly greater activity against Gram-negative aerobes and slightly less activity against Gram-positives. It is not significantly degraded by renal dehydropeptidase and does not require an inhibitor. Ertapenem is less active than meropenem or imipenem against Pseudomonas aeruginosa and acinetobacter species. It is not degraded by renal dehydropeptidase. Carbapenems penetrate body tissues and fluids well, including the cerebrospinal fluid. All are cleared renally, and the dose must be reduced in patients with renal insufficiency. The usual dose of imipenem is 0.25–0.5 g given intravenously every 6–8 hours (halflife 1 hour). The usual adult dose of meropenem is 1 g intravenously every 8 hours. Ertapenem has the longest half-life (4 hours) and is administered as a once-daily dose of 1 g intravenously or 87 intramuscularly. Intramuscular ertapenem is irritating, and for that reason the drug is formulated with 1% lidocaine for administration by this route. A carbapenem is indicated for infections caused by susceptible organisms that are resistant to other available drugs and for treatment of mixed aerobic and anaerobic infections. Carbapenems are active against many highly penicillin-resistant strains of pneumococci. A carbapenem is the β-lactam antibiotic of choice for treatment of enterobacter infections, since it is resistant to destruction by the lactamase produced by these organisms. Strains of Pseudomonas aeruginosa may rapidly develop resistance to imipenem or meropenem, so simultaneous use of an aminoglycoside is recommended for infections caused by those organisms. Ertapenem is insufficiently active against P aeruginosa and should not be used to treat infections caused by that organism. Imipenem or meropenem with or without an aminoglycoside may be effective treatment for febrile neutropenic patients. Adverse effects are nausea, vomiting, diarrhea, skin rashes, and reactions at the infusion sites. Excessive levels of imipenem in patients with renal failure may lead to seizures. Meropenem and ertapenem are less likely to cause seizures than imipenem. Patients allergic to penicillins may be allergic to carbapenems as well. B) VANCOMYCIN Vancomycin is an antibiotic produced by Streptococcus orientalis. With the single exception of flavobacterium, it is active only against Gram-positive bacteria, particularly staphylococci. Vancomycin inhibits cell wall synthesis by binding firmly to the D-Ala-D-Ala terminus of nascent peptidoglycan pentapeptide. Vancomycin is bactericidal for Gram-positive bacteria in concentrations of 0.5– 10 g/mL. Most pathogenic staphylococci, including those producing lactamase and those resistant to nafcillin and methicillin, are killed by 4 g/mL or less. Vancomycin kills staphylococci relatively slowly and only if cells are actively dividing; the rate is less than that of the penicillins both in vitro and in vivo. Vancomycin is synergistic with 88 gentamicin and streptomycin against E. faecium and E. faecalis strains that do not exhibit high levels of aminoglycoside resistance. Vancomycin is poorly absorbed from the intestinal tract and is administered orally only for the treatment of antibiotic-associated enterocolitis caused by Clostridium difficile. Parenteral doses must be administered intravenously. A 1 hour intravenous infusion of 1 g produces blood levels of 15–30 g/mL for 1–2 hours. The drug is widely distributed in the body. Cerebrospinal fluid levels 7–30% of simultaneous serum concentrations are achieved if there is meningeal inflammation. Ninety percent of the drug is excreted by glomerular filtration. The main indication for parenteral vancomycin is sepsis or endocarditis caused by methicillin-resistant staphylococci. However, vancomycin is not as effective as antistaphylococcal penicillin for treatment of serious infections, such as endocarditis, caused by methicillin-susceptible strains. Vancomycin in combination with gentamicin is an alternative regimen for treatment of enterococcal endocarditis in a patient with serious penicillin allergy. Vancomycin (in combination with cefotaxime, ceftriaxone, or rifampin) is also recommended for treatment of meningitis suspected or known to be caused by a highly penicillin-resistant strain of pneumococcus (i.e., MIC > 1 g/mL). The recommended dosage is 30 mg/kg/d in two or three divided doses. A typical dosing regimen for most infections in adults with normal renal function is 1 g every 12 hours. The dosage in children is 40 mg/kg/d in three or four divided doses. Oral vancomycin, 0.125–0.25 g every 6 hours, is used to treat antibiotic-associated enterocolitis caused by Clostridium difficile. However, because of the emergence of vancomycin-resistant enterococci and the strong selective pressure of oral vancomycin for these resistant organisms, metronidazole is strongly preferred as initial therapy and vancomycin should be reserved for treatment of refractory cases. Adverse effects are encountered in about 10% of cases. Most reactions are minor. Vancomycin is irritating to tissue, resulting in phlebitis at the site of injection. Chills and fever may occur. 89 Ototoxicity is rare and nephrotoxicity uncommon with current preparations. However, administration with another ototoxic or nephrotoxic drug, such as an aminoglycoside, increases the risk of these toxicities. Among the more common reactions is the so-called "red man" or "red neck" syndrome. This infusion-related flushing is caused by release of histamine. It can be largely prevented by prolonging the infusion period to 1–2 hours or increasing the dosing interval. 6.2. PROTEIN SYNTHESIS INHIBITORS (Tetracyclines, Macrolides, Aminoglycosides, Chloramphenicol, Clindamycin) A) TETRACYCLINES Tetracyclines are broad-spectrum bacteriostatic antibiotics that inhibit protein synthesis.. The group includes tetracycline, oxytetracycline, demeclocycline, lymecycline, doxycycline and minocycline They are active against many Gram-positive and Gramnegative bacteria, including anaerobes, rickettsiae, chlamydiae, mycoplasmas, and L. forms; and against some protozoa, e.g., amebas. The antibacterial activities of most tetracyclines are similar except that tetracycline-resistant strains may be susceptible to doxycycline, minocycline, and tigecycline, all of which are poor substrates for the efflux pump that mediates resistance. Differences in clinical efficacy for susceptible organisms are minor and attributable largely to features of absorption, distribution, and excretion of individual drugs. The oral dosage for rapidly excreted tetracyclines, equivalent to tetracycline hydrochloride, is 0.25–0.5 g four times daily for adults and 20–40 mg/kg/d for children (8 years of age and older). For severe systemic infections, the higher dosage is indicated, at least for the first few days. The daily dose is 600 mg for demeclocycline or methacycline, 100 mg once or twice daily for doxycycline, and 100 mg twice daily for minocycline. Doxycycline is the oral tetracycline of choice because it can be given as a once-daily dose and its absorption is not significantly affected by food. All tetracyclines 90 chelate with metals, and none should be orally administered with milk, antacids, or ferrous sulfate. To avoid deposition in growing bones or teeth, tetracyclines should be avoided in pregnant women and children under 8 years of age. Several tetracyclines are available for intravenous injection in doses of 0.1–0.5 g every 6–12 hours (similar to oral doses) but doxycycline is the usual preferred agent, at a dosage of 100 mg every 12–24 hours. Intramuscular injection is not recommended because of pain and inflammation at the injection site. Adverse Effects Gastric discomfort: Epigastric distress commonly results from irritation of the gastric mucosa and is often responsible for noncompliance in patients treated with these drugs. The discomfort can be controlled if the drug is taken with foods other than dairy products. Effects on calcified tissues: Deposition in the bone and primary dentition occurs during calcification in growing children; this causes discoloration and hypoplasia of the teeth and a temporary stunting of growth. Fatal hepatotoxicity: This side effect has been known to occur in pregnant women who received high doses of tetracyclines, especially if they are experiencing pyelonephritis. Phototoxicity: Phototoxicity, for example, a severe sunburn, occurs when the patient receiving a tetracycline is exposed to sun or ultraviolet rays. This toxicity is encountered most frequently with tetracycline, doxycycline, and demeclocycline. Vestibular problems: These side effects (for example, dizziness, nausea, vomiting) occur with minocycline, which concentrates in the endolymph of the ear and affects function. Pseudotumor cerebri: Benign intracranial hypertension characterized by headache and blurred vision, may occur in adults. Though discontinuation of the drug reverses the condition; it is not clear whether permanent sequelae may occur. Organs and tissue toxicity: Tetracyclines can probably impair hepatic function, especially during pregnancy, in patients with 91 preexisting hepatic insufficiency and when high doses are given intravenously. Hepatic necrosis has been reported with daily doses of 4 g or more intravenously. Renal tubular acidosis and other renal injury resulting in nitrogen retention have been attributed to the administration of outdated tetracycline preparations. Tetracyclines, given along with diuretics, may produce nitrogen retention. Tetracyclines, other than oxycycline, may accumulate to toxic levels in patients with impaired kidney function. Intravenous injection can lead to venous thrombosis. Intramuscular injection produces painful local irritation and should be avoided. Superinfections: Candida overgrowths (for example in the vagina) or increase in resistant staphylococci (in the intestine) may occur. Contraindications: Renally-impaired patients should not be treated with any of the tetracyclines except doxycycline and minocycline. Accumulation of tetracyclines may aggravate preexisting azotemia by interfering with protein synthesis, thus promoting amino acid degradation The tetracyclines should not be employed in pregnant or breast-feeding women, or in children under 8 years of age. B) MACROLIDES The macrolides are a group of closely related compounds characterized by a macrocyclic lactone ring (usually containing 14 or 16 atoms) to which deoxy sugars are attached. The prototype drug, erythromycin, which consists of two sugar moieties attached to a 14-atom lactone ring, was obtained in 1952 from Streptomyces erythreus. The newer members of this family, clarithromycin (a methylated form of erythromycin) and azithromycin (having a larger lactone ring), have some features in common with, and others that improve on, erythromycin. Recently, dirithromycin, a macrolide similar to erythromycin in antibacterial spectrum but with the advantage of one-daily dosage, has been approved. Erythromycin has activity against many species of campylobacter, chlamydia, mycoplasma, legionella, Gram-positive 92 cocci, and some Gram-negative organisms. The spectrums of activity of azithromycin and clarithromycin are similar but include greater activity against Chlamydia, M avium complex (MAC), Haemophilus influenzae and Moraxella catarrhalis and toxoplasma. Azithromycin: Except for its cost, it is now the preferred therapy for urethritis caused by Chlamydia trachomatis. Its activity against Mycobacterium avium intracellulare complex has not proven to be clinically important except in AIDS patients with disseminated infections. Resistance to the macrolides in Gram-positive organisms involves production of a methylase that adds a methyl group to the ribosomal binding site. Resistance in enterobacteria is the result of formation of drug-metabolizing esterases. Cross-resistance between the individual macrolides is complete. Adverse Effects Epigastric Distress: This side effect is common and can lead to poor patient compliance for erythromycin. The new macrolides seem to be better tolerated by the patient; gastrointestinal problems are their most common side effects. Cholestatic Hepatitis: This side effect occurs, especially with the estolate form of erythromycin, presumably as the result of a hypersensitivity reaction to the estolate form (the lauryl salt of the propionyl ester of erythromycin). It has also been reported for other forms of the drug. Ototoxicity: Transient deafness has been associated with erythromycin, especially at high dosages. Skin Rashes, and Eosinophilia, Cardiac Arrhythmias. Erythromycin inhibits several forms of hepatic cytochrome P450 and can increase the plasma levels of anticoagulants, carbamazepine, cisapride, digoxin, and theophylline. Contraindications: Patients with hepatic dysfunction should not be treated with erythromycin since the drug accumulates in the liver. 93 C) CLYNDAMICINE The lincosamides lincomycin and clindamycin inhibit bacterial protein synthesis via a mechanism similar to that of the macrolides, though they are not chemically related. Mechanisms of resistance include methylation of the binding site on the 50S ribosomal subunit and enzymatic inactivation. Cross-resistance between lincosamides and macrolides is common. Good tissue penetration occurs after oral absorption. The fincosamides are eliminated partly by metabolism and partly by biliary and renal excretion. The main use of clindamycin is in the treatment of severe infections due to certain anaerobes such as bacteroides. Clindamycin has been used as a backup drug against Gram-positive cocci and is currently recommended for prophylaxis of endocarditis in valvular disease patients who are penicillin-allergic. The drug is also active against Mocystis carinii pneumonia and Toxoplasmjsis. The toxicity of clindamycin includes gastrointestinal irritation, skin rashes, neutropenia, hepatic dysfunction, and possible superinfections. D) CHLORAMPHENICOL Chloramphenicol is a bacteriostatic broad-spectrum antibiotic that is active against both aerobic and anaerobic Gram-positive and Gram-negative organisms. It is active also against rickettsiae but not chlamydiae. Most Gram-positive bacteria are inhibited at concentrations of 1–10 mcg/mL, and many Gram-negative bacteria are inhibited by concentrations of 0.2–5 mcg/mL. H. influenzae, N. meningitidis, and some strains of bacteroides are highly susceptible, and for them chloramphenicol may be bactericidal. However, because of its toxicity, its use is restricted to lifethreatening infections for which no alternatives exist. Adverse Effects Gastrointestinal disturbances: Adults occasionally develop nausea, vomiting, and diarrhea. This is rare in children. Oral or vaginal candidiasis may occur as a result of alteration of normal microbial flora. 94 Bone marrow disturbances: Chloramphenicol commonly causes a dose-related reversible suppression of red cell production at dosages exceeding 50 mg/kg/d after 1–2 weeks. Aplastic anemia, a rare consequence (1 in 24,000 to 40,000 courses of therapy) of chloramphenicol administration by any route, is an idiosyncratic reaction unrelated to dose, although it occurs more frequently with prolonged use. It tends to be irreversible and can be fatal. Toxicity for newborn infants: The drug may accumulate, resulting in the Gray Baby Syndrome with vomiting, flaccidity, hypothermia, gray color, shock, and collapse. To avoid this toxic effect, chloramphenicol should be used with caution in infants and the dosage limited to 50 mg/kg/d or less (during the first week of life) in full-term infants more than 1 week old and 25 mg/kg/d in premature infants. Interaction with other drugs: Chloramphenicol inhibits hepatic microsomal enzymes that metabolize several drugs. Half-lives are prolonged, and the serum concentrations of phenytoin, tolbutamide, chlorpropamide, and warfarin are increased. Like other bacteriostatic inhibitors of microbial protein synthesis, chloramphenicol can antagonize bactericidal drugs, such as penicillins or aminoglycosides. E) AMINOGLICOSIDES The aminoglycosides are a group of antibiotics of complex chemical structure resembling each other in antimicrobial activity, pharmacokinetic characteristics and toxicity. The main agents are gentamicin, streptomycin, amikacin, tobramycin, netilmicin and neomycin. Aminoglycoside antibiotics had been the mainstays for treatment of serious infections due to aerobic Gram-negative bacilli. They are most widely used against Gram-negative enteric organisms and in sepsis. However, because their use is associated with serious toxicities, they have been replaced to some extent by safer antibiotics, such as the third- and fourth-generation cephalosporins, the fluoroquinolones, and the carbapenems. They may be given together with penicillin in streptococcocal infections caused by Listeria spp. and P. aeruginosa. Gentamicin is the aminoglycoside most commonly used, although tobramycin is the preferred member 95 of this group for P. aeruginosa infections. Amikacin has the widest antimicrobial spectrum and, along with netilmicin, can be effective in infections with organisms resistant to gentamicin and tobramycin. The aminoglycoside antibiotics are rapidly bactericidal. Bacteria may be resistant to aminoglycosides because of failure of the antibiotic to penetrate intracellularly, low affinity of the drug for the bacterial ribosome, or inactivation of the drug by microbial enzymes. Clinically, drug inactivation is the most common mechanism for acquired microbial resistance to aminoglycosides. The genes encoding aminoglycoside-modifying enzymes are acquired primarily by conjugation and transfer of resistance plasmids. Adverse Effects It is important to monitor plasma levels of gentamicin, tobramycin, and amikacin to avoid concentrations that cause doserelated toxicities Ototoxicity: Ototoxicity (vestibular and cochlear) is directly related to high peak plasma levels and the duration of treatment. Vertigo and loss of balance (especially in patients receiving streptomycin) may also occur, because these drugs affect the vestibular apparatus. The nephrotoxicity consists of damage to the kidney tubules and can be reversed if the use of the drugs is stopped. Nephrotoxicity is more likely to occur in patients with pre-existing renal disease or in conditions in which urine volume is reduced, and concomitant use of other nephrotoxic agents (e.g., cephalosporins) increases the risk. Nephrotoxicity: Retention of the aminoglycosides by the proximal tubular cells disrupts calcium-mediated transport processes, and this results in kidney damage ranging from mild, reversible renal impairment to severe, acute tubular necrosis, which can be irreversible. Neuromuscular paralysis: This side effect most often occurs after direct intraperitoneal or intrapleural application of large doses of aminoglycosides. The mechanism is responsible in a decrease in both the release of acetylcholine from prejunctional nerve endings and the 96 sensitivity of the postsynaptic site. Patients with myasthenia gravis are particularly at risk. Prompt administration of calcium gluconate or neostigmine can reverse the block. Allergic reactions: Contact dermatitis is a common reaction to topically applied neomycin. 6.3. MISCELLANEOUS ANTIBACTERIAL AGENTS Vancomycin is a glycopeptide antibiotic, and teicoplanin is similar but longer lasting. Vancomycin is bactericidal (except against streptococci) and acts by inhibiting cell wall synthesis. It is effective mainly against Gram-positive bacteria and has been used against methicillin-resistant staphylococci. Vancomycin is not absorbed from the gut and is only given by the oral route for treatment of gastrointestinal infection with C. difficile. For parenteral use, it is given intravenously and has a plasma half-life of about 8 hours. Adverse effects include fever, rashes and local phlebitis at the site of injection. Ototoxicity and nephrotoxicity can occur, and hypersensitivity reactions are occasionally seen. Nitrofurantoin is a synthetic compound active against a range of Gram-positive and Gram-negative organisms. The development of resistance in susceptible organisms is rare, and there is no crossresistance. Its mechanism of action is not known. It is given orally and is rapidly and totally absorbed from the gastrointestinal tract and just as rapidly excreted by the kidney. The clinical use of nitrofurantoin is confined to the treatment of urinary tract infections. The polymixin antibiotics in use are polymixin B and colistin (polymixin E). They have cationic detergent properties and exert their antibacterial action by disrupting the cell membrane phospholipids. They have a selective, rapidly bactericidal action on Gram-negative bacilli, especially pseudomonads and coliform organisms. They are not absorbed from the gastrointestinal tract. Clinical use of these drugs is limited by their toxicity (see below) and is confined largely to gut sterilisation and topical treatment of ear, eye or skin infections caused by susceptible organisms. 97 Adverse effects may be serious and include neurotoxicity and nephrotoxicity. Metronidazole was introduced as an antiprotozoal agent, but it is also active against anaerobic bacteria such as Bacteroides, Clostridia sp. and some streptococci. It is effective in the therapy of pseudomembranous colitis, a clostridial infection sometimes associated with antibiotic therapy (see above), and is important in the treatment of serious anaerobic infections (e.g. sepsis secondary to bowel disease). 6.4. ANTIMICROBIAL TOPOISOMERASE AGENTS AFFECTING A) FLUOROQUINOLONES The fluoroquinolones include the broad-spectrum agents ciprofloxacin, levofloxacin, ofloxacin, norfloxacin and moxifloxacin, as well as a narrow-spectrum drug used in urinary tract infections,– nalidixic acid (the first quinolone and not fluorinated). These agents inhibit topoisomerase II (a bacterial DNA gyrase), the enzyme that produces a negative supercoil in DNA and thus permits transcription or replication. Ciprofloxacin is the most commonly used fluoroquinolone and will be described as the type agent. It is a broadspectrum antibiotic effective against both Gram-positive and Gramnegative organisms. It has excellent activity against the Enterobacteriaceae (the enteric Gram-negative bacilli), including many organisms resistant to penicillins, cephalosporins and aminoglycosides, and it is also effective against H. influenzae, penicillinase-producing N. gonorrhoeae, Campylobacter spp. and pseudomonads. Amongst the Gram-positive organisms, streptococci and pneumococci are only weakly inhibited, and there is a high incidence of staphylococcal resistance. Ciprofloxacin should be avoided in methicillin-resistant staphylococcal infections. Clinically, the fluoroquinolones are best used for infections with facultative and aerobic Gram-negative rods and cocci. Resistant strains of Staphylococous aureus and Pseudomonas aeruginosa have emerged. 98 Given orally, the fluoroquinolones are well absorbed. The half-life of ciprofloxacin and norfloxacin is 3 hours, and that of ofloxacin is 5 hours. The drugs accumulate in several tissues, particularly in the kidney, prostate and lung. All quinolones are concentrated in phagocytes. Most fail to cross the blood-brain barrier, but ofloxacin penetrates the CSF and attains 40% of its serum concentrations. Aluminium and magnesium antacids interfere with the absorption of the quinolones. Elimination of ciprofloxacin and norfloxacin occurs partly by hepatic metabolism by P450 enzymes (which they can inhibit, giving rise to interactions with other drugs) and partly by renal excretion. Ofloxacin is excreted in the urine. Adverse Effects Unwanted effects are infrequent, usually mild and disappear when the drugs are withdrawn. The most frequent manifestations are gastrointestinal disorders and skin rashes. Arthropathy has been reported in young individuals. Central nervous system symptomsheadache and dizziness have occurred as well as, less frequently, convulsions associated with central nervous system pathology or concurrent use of theophylline or a NSADs. There is a clinically important interaction between ciprofloxacin and this drug (through inhibition of P450 enzymes), which can lead to theophylline toxicity in asthmatics treated with the fluoroquinolones. Gastrointestinal: The most common adverse effects of the fluoroquinolones are nausea, vomiting, and diarrhea, which occur in 3–6% of patients. Central nervous system problems: The most prominent central nervous system (CNS) effects of fluoroquinolone treatment are headache and dizziness or lightheadedness. Thus, patients with CNS disorders, such as epilepsy, should be treated cautiously with these drugs. Phototoxicity: Patients taking fluoroquinolones are advised to avoid excessive sunlight and to apply sunscreens. However, the latter may not protect completely. Thus, it is advisable that the drug intake should be discontinued at the first sign of phototoxicity. 99 Connective tissue problems: Fluoroquinolones should be avoided in pregnancy, in nursing mothers, and in children under 18 years of age, because articular cartilage erosion (arthropathy) occurs in immature experimental animals. Children with cystic fibrosis who receive ciprofloxacin have had few problems, but careful monitoring is indicated. In adults, fluoroquinolones can infrequently cause ruptured tendons. Contraindications: Moxifloxacin may prolong the QTc interval and, thus, should not be used in patients who are predisposed to arrhythmias or are taking antiarrhythmic medications. Drug interactions: The effect of antacids and cations on the absorption of these agents was considered above. Ciprofloxacin and ofloxacin can increase the serum levels of theophylline by inhibiting its metabolism. This is not the case with the third- and fourthgeneration fluoroquinolones, which may raise the serum levels of warfarin, caffeine, and cyclosporine. 6.5. ANTIFOLATE DRUGS SULFONAMIDES The sulfonamides are weakly acidic compounds that have a common chemical nucleus resembling p-aminobenzoic acid (PABA). Members of this group differ mainly in their pharmacokinetic properties and clinical uses. Pharmacokinetic features include modest tissue penetration, hepatic metabolism, and excretion of both intact drug and acetylated metabofites in the urine. Solubility may be decreased in acidic urine, resulting in precipitation of the drug or its metabolites. Because of the solubility limitation, a combination of three separate sulfonamides (triple sulfa) has been used to reduce the likelihood that any one drug will precipitate. The sulfonamides may be classified as short-acting (e.g., sulfisoxazole), intermediate-acting (e.g., sulfamethoxazole), and long-acting (e.g., sulfadoxine). Sulfonamides bind to plasma proteins at sites shared by bilirubin and by other drugs. The sulfonamides may be classified into three groups on the basis of the rapidity with which they are absorbed and excreted: 100 1) agents that are absorbed and excreted rapidly, such as sulfisoxazole and sulfadiazine; 2) agents that are absorbed very poorly when administered orally and hence are active in the bowel lumen, such as sulfasalazine; 3) agents that are used mainly topically, such as sulfacetamide, mafenide, and silver sulfadiazine; 4) long-acting sulfonamides, such as sulfadoxine, that are absorbed rapidly but slowly excreted. Sulfonamides are infrequently used as single agents. Many strains of formerly susceptible species, including meningococci, pneumococci, streptococci, staphylococci, and gonococci, are now resistant. The fixed-drug combination of trimethoprimsulfamethoxazole is the drug of choice for infections, such as Pneumocystis jiroveci (formerly P carinii) pneumonia, toxoplasmosis, nocardiosis, and occasionally other bacterial infections. ORAL ABSORBABLE AGENTS Sulfisoxazole and sulfamethoxazole are short- to medium-acting agents used almost exclusively to treat urinary tract infections. The usual adult dosage is 1 g of sulfisoxazole four times daily or 1 g of sulfamethoxazole two or three times daily. Sulfadiazine in combination with pyrimethamine is first-line therapy for treatment of acute toxoplasmosis. The combination of sulfadiazine with pyrimethamine, a potent inhibitor of dihydrofolate reductase, is synergistic because these drugs block sequential steps in the folate synthetic pathway blockade. The dosage of sulfadiazine is 1 g four times daily, with pyrimethamine given as a 75-mg loading dose followed by a 25-mg once-daily dose. Folinic acid, 10 mg orally each day, should also be administered to minimize bone marrow suppression. Sulfadoxine is the only long-acting sulfonamide currently available in the United States and only as a combination formulation with pyrimethamine, a second-line agent in treatment for malaria 101 Oral nonabsorbable agents: Sulfasalazine (salicylazosulfapyridine) is widely used in ulcerative colitis, enteritis, and other inflammatory bowel diseases. TOPICAL AGENTS Sodium sulfacetamide ophthalmic solution or ointment is effective treatment for bacterial conjunctivitis and as adjunctive therapy for trachoma. Another sulfonamide, mafenide acetate, is used topically but can be absorbed from burn sites. The drug and its primary metabolite inhibit carbonic anhydrase and can cause metabolic acidosis, a side effect that limits its usefulness. Silver sulfadiazine is a much less toxic topical sulfonamide and is preferred to mafenide for prevention of infection of burn wounds. Trimethoprim: This drug is structurally similar to folic acid. It is a weak base and is trapped in acidic environments, reaching high concentrations in prostatic and vaginal fluids. A large fraction of trimethoprim is excreted unchanged in the urine. The half-life of this drug is similar to that of sulfamethoxazole (10–12 hours). Adverse Effects Crystalluria: Nephrotoxicity develops as a result of crystalluria. Adequate hydration and alkalinization of urine prevent the problem by reducing the concentration of drug and promoting its ionization. Agents, such as sulfisoxazole and sulfamethoxazole, are more soluble at urinary pH than the older sulfonamides (for example, sulfadiazine) and less liable to cause crystalluria. Hypersensitivity: Hypersensitivity reactions, such as rashes, angioedema, and Stevens-Johnson syndrome, are fairly common. The latter occurs more frequently with the longer-acting agents. Hemopoietic Disturbances: Hemolytic anemia is encountered in patients with glucose 6-phosphate dehydrogenase deficiency. Granulocytopenia and thrombocytopenia can also occur. Miscellaneous Reactions Anorexia, nausea, and vomiting occur in 1-2% of persons receiving sulfonamides, and these manifestations probably are central in origin. The administration of sulfonamides to 102 newborn infants, especially if premature, may lead to the displacement of bilirubin from plasma albumin. Kernicterus: This disorder may occur in newborns, because sulfa drugs displace bilirubin from binding sites on serum albumin. The bilirubin is then free to pass into the CNS, because the baby's bloodbrain barrier is not fully developed. 7. DRUGS USED IN THE TREATMENT OF GIT DISORDERS The gastrointestinal tract serves several functions: digestive, excretory, endocrine, exocrine, etc. These functions provide numerous important drug targets, and many of the drugs used in gastrointestinal disease have been discussed in earlier chapters of this book. However, several important drugs used in common gastrointestinal diseases do not fall into the drug groups discussed earlier; these agents are described in this chapter. Acid-peptic diseases include gastroesophageal reflux, peptic ulcer (gastric and duodenal), and stress-related mucosal injury. In all these conditions, mucosal erosions or ulceration arise when the caustic effects of aggressive factors (acid, pepsin, bile) overwhelm the defensive factors of the gastrointestinal mucosa (mucus and bicarbonate secretion, prostaglandins, blood flow, and the processes of restitution and regeneration after cellular injury). Over 99% of peptic ulcers are caused by infection with the bacterium Helicobacter pylori or by use of nonsteroidal anti-inflammatory drugs (NSAIDs). Drugs used in the treatment of acid-peptic disorders may be divided into two classes: agents that reduce intragastric acidity and agents that promote mucosal defense. 7.1. GENERAL PRINCIPLES IN THE TREATMENT OF PEPTIC ULCER DISEASE Although the pathogenesis of peptic ulcer disease is not fully understood, several major causative factors are recognized: 103 nonsteroidal anti-inflammatory drug (NSAID) use, infection with Gram-negative Helicobacter pylori, increased hydrochloric acid secretion, and inadequate mucosal defense against gastric acid. Chronic infection with Helicobacter pylori is present in the great majority of patients with recurrent non-NSAID-induced peptic ulcers, and eradication of this organism greatly reduces the rate of recurrence of ulcer in these patients. The regimens of choice consist of a proton pump inhibitor plus a course of bismuth, tetracycline, and metronidazole or a course of amoxicillin plus clarithromycin. Compared with H2 antagonists, proton pump inhibitors afford more rapid symptom relief and faster ulcer healing for duodenal ulcers and, to a lesser extent, gastric ulcers. All of the pump inhibitors heal more than 90% of duodenal ulcers within 4 weeks and a similar percentage of gastric ulcers within 6–8 weeks. 1. H. pylori-associated ulcers: For H. pylori-associated ulcers, there are two therapeutic goals: to heal the ulcer and eradicate the organism. The most effective regimens for H. pylori eradication are combinations of two antibiotics and a proton pump inhibitor. PPIs promote eradication of H. pylori through several mechanisms: direct antimicrobial properties (minor); raising intragastric pH and lowering the minimal inhibitory concentrations of antibiotics against H. pylori. The best treatment regimen consists of a 10-14 day regimen of "Triple therapy": a proton pump inhibitor twice daily; clarithromycin, 500 mg twice daily; and amoxicillin, 1 g twice daily. For patients who are allergic to penicillin, metronidazole, 500 mg twice daily, should be substituted for amoxicillin. After completion of triple therapy, the proton pump inhibitor should be continued once daily for a total of 4-6 weeks to ensure complete ulcer healing. 2. NSAID-associated ulcers: For patients with ulcers caused by aspirin or other NSAIDs, either H2 antagonists or proton pump inhibitors provide rapid ulcer healing so long as the NSAID is discontinued; continued use of the NSAID impairs ulcer healing. Treatment with a once-daily proton pump inhibitor promotes ulcer healing despite continued NSAID therapy. PPIs are also given to prevent ulcer complications from NSAIDs. Asymptomatic peptic ulceration develops in 10–20% of people 104 taking frequent NSAIDs, and ulcer-related complications (bleeding, perforation) develop in 1–2% of persons per year. Proton pump inhibitors taken once daily are effective in reducing the incidence of ulcers and ulcer complications in patients taking aspirin or other NSAIDs. 3. Prevention of rebleeding from peptic ulcers: In patients with acute gastrointestinal bleeding due to peptic ulcers, the risk of rebleeding from ulcers that have a visible vessel or adherent clot is increased. Rebleeding in this subset of high-risk ulcers is reduced significantly with use of proton pump inhibitors administered for 3–5 days either as high-dose oral therapy (eg, omeprazole, 40 mg orally twice daily) or as a continuous intravenous infusion. It is believed that an intragastric pH higher than 6 may enhance coagulation and platelet aggregation. The optimal dose of intravenous proton pump inhibitor needed to achieve and maintain this level of near-complete acid inhibition is unknown; however, initial bolus administration (60–80 mg) followed by constant infusion (8 mg/h) commonly is recommended. Pharmacological Therapeutic Classification of Drugs Treatment approaches are: 1) drugs to eradicate the H. pylori infection; 2) agents to reduce secretion of gastric acid with the use of H2receptor antagonists or proton pump ingibitors; 3) provision of agents that protect the gastric mucosa from damage, such as misoprostol and sucralfate. Gastric acid secretion by parietal cells of the gastric mucosa is stimulated by – gastrin (a stimulatory hormone); – acetylcholine (a stimulatory neurotransmitter); – histamine (a stimulatory local hormone); – prostaglandins E2 and I2 (local hormones that inhibit acid secretion). The receptor-mediated binding of acetylcholine, histamine or gastrin results in the activation of protein kinases which, in turn, stimulate the H+/K+ adenosine triphosphatase (ATPase) proton pump 105 to secrete hydrogen ions in exchange for K+ into the lumen of the stomach. A Cl- channel couples chloride efflux to the release of H+. In contrast, receptor binding of prostaglandin E2 and somatostatin diminish gastric acid production. Histamine binding causes activation of adenylyl cyclase, whereas binding of prostaglandin E2 inhibits this enzyme. Gastrin and acetylcholine act by inducing an increase in intracellular calcium levels. 7.1.1. INHIBITORS OF THE H+/K+-ATPase PROTON PUMP Omeprazole is the first of a class of drugs that bind to the H+/K+ATPase enzyme system (proton pump) of the parietal cell, thereby suppressing secretion of hydrogen ions into the gastric lumen. The membrane-bound proton pump is the final step in the secretion of gastric acid. Four additional PPIs are now available: lansoprazole, rabeprazole, pantoprazole, and esomeprazole. These agents are prodrugs with an acid-resistant enteric coating to protect them from premature degradation by gastric acid. The coating is removed in the alkaline duodenum, and the prodrug, a weak base, is absorbed and transported to the parietal cell canaliculus. There, it is converted to the active form, which reacts with a cysteine residue of the H+/K+-ATPase, forming a stable covalent bond. It takes about 18 hours for the enzyme to be resynthesized. At standard doses, all PPIs inhibit both basal and stimulated gastric acid secretion by more than 90%. Acid suppression begins within 1-2 hours after the first dose of lansoprazole and slightly earlier with omeprazole. There is also an oral product containing omeprazole combined with sodium bicarbonate for faster absorption. It is available in powder to be dissolved in water and taken orally as well as in capsule form. Therapeutic uses: The superiority of the PPIs over the H2 blockers for suppressing acid production and healing peptic ulcers has made them the preferred drugs for treating erosive esophagitis and active duodenal ulcer and for long-term treatment of pathologic hypersecretory conditions (for example, Zollinger-Ellison syndrome, in which a gastrin-producing tumor causes hypersecretion of HCl). They are approved for the treatment of GERD. Clinical studies have 106 shown that PPIs reduce the risk of bleeding from an ulcer caused by aspirin and other NSAIDs. They are also successfully used with antimicrobial regimens to eradicate H. pylori. For maximum effect, PPIs should be taken 30 minutes before breakfast or the largest meal of the day. If an H2-receptor antagonist is also needed, it should be taken well after the PPI for best effect. The H2 antagonists will reduce the activity of the proton pump, and PPIs require active pumps to be effective. In patients with GERD in whom once-daily PPI is partially effective, increasing to a twice-daily regimen or keeping the PPI in the morning and adding an H2 antagonist in the evening may improve symptom control. Pharmacokinetics: All these agents are delayed-release formulations and are effective orally. Some are also available for intravenous injection. Metabolites of these agents are excreted in urine and feces. Adverse Effects The PPIs are generally well tolerated, but concerns about longterm safety have been raised due to the increased secretion of gastrin. Omeprazole inhibits the metabolism of warfarin, phenytoin, diazepam, and cyclosporine. However, drug interactions are not a problem with the other PPIs. Prolonged therapy with agents that suppress gastric acid, such as the PPIs and H2 antagonists, may result in low vitamin B12, because acid is required for its absorption. Some studies have reported an increased risk of both community-acquired respiratory infections and nosocomial pneumonia among patients taking proton pump inhibitors. 7.1.2. H2-RECEPTOR ANTAGONISTS Although antagonists of the histamine H 2 receptor block electively the actions of histamine at all H 2 receptors in the stomach, blood vessels, and other sites, their chief clinical use is to inhibit gastric acid secretion, being particularly effective against nocturnal acid secretion. By competitively blocking the binding of histamine to H2 receptors, these agents reduce the intracellular 107 concentrations of cyclic adenosine monophosphate and, thereby, secretion of gastric acid. The four drugs used in Ukraine now: cimetidine, ranitidine, famotidine, and nizatidine potently inhibit (greater than 90 %) basal, food-stimulated, and nocturnal secretion of gastric acid after a single dose. Cimetidine is the prototype histamine H2-receptor antagonist; however, its utility is limited by its adverse effect profile and drug interactions. The common indications are gastroesophageal disease, peptic ulcer desease, nonulcer dyspepsia, prevention of bleeding from stress-related gastritis. H2 blockers are given orally, distribute widely throughout the body (including into breast milk and across the placenta), and are excreted mainly in the urine. Cimetidine normally has a short serum half-life, which is increased in renal failure. Approximately 30% of a dose of cimetidine is slowly inactivated by the liver's microsomal mixed-function oxygenase system and can interfere in the metabolism of many other drugs; the other 70% is excreted unchanged in the urine. The dosage of all these drugs must be decreased in patients with hepatic or renal failure. Cimetidine inhibits cytochrome P450 and can slow metabolism (and, thus, potentiate the action) of several drugs (for example, warfarin, diazepam, phenytoin, quinidine, carbamazepine, theophylline, and imipramine), sometimes resulting in serious adverse clinical effects. Therapeutic uses: Compared to cimetidine, ranitidine is longer acting and is five- to ten-fold more potent. Ranitidine has minimal side effects and does not produce the antiandrogenic or prolactinstimulating effects of cimetidine. Unlike cimetidine, it does not inhibit the mixed-function oxygenase system in the liver and, thus, does not affect the concentrations of other drugs. Famotidine is similar to ranitidine in its pharmacologic action, but it is 20–50 times more potent than cimetidine, and 3–20 times more potent than ranitidine. Nizatidine is similar to ranitidine in its pharmacologic action and potency. In contrast to cimetidine, ranitidine, and famotidine, which are metabolized by the liver, nizatidine is eliminated principally by the kidney. Because little first-pass 108 metabolism occurs with nizatidine, its bioavailability is nearly 100 %. No intravenous preparation is available. Adverse Effects The most common side effects are headache, dizziness, diarrhea, and muscular pain. Other central nervous system effects (confusion, hallucinations) occur primarily in elderly patients or after intravenous administration. Cimetidine can also have endocrine effects, because it acts as a nonsteroidal antiandrogen. These effects include gynecomastia, galactorrhea (continuous release/discharge of milk), and reduced sperm count. Except for famotidine, all these agents inhibit the gastric first-pass metabolism of ethanol. Drugs, such as ketoconazole, which depend on an acidic medium for gastric absorption, may not be efficiently absorbed if taken with one of these antagonists. 7.1.3. ANTACIDS Antacids are simple physical agents that react with protons in the lumen of the gut. Some antacids (aluminum-containing antacids) may also stimulate the protective functions of the gastric mucosa. The antacids effectively reduce the recurrence rate of peptic ulcers when used regularly in the large doses needed to significantly raise the stomach pH. The antacids differ mainly in their absorption and effect on stool consistency. The most popular antacids (Maalox, Almagel) consist of magnesium hydroxide (Mg[OH]2) and aluminum hydroxide (AI[OH]3), and Phosphalugel consists aluminum phosphate. Neither of these weak bases is significantly absorbed from the bowel. Magnesium hydroxide has a strong laxative effect, while aluminum hydroxide has a constipating action. These drugs are available as single-ingredient products and as combined preparations. Calcium carbonate and sodium bicarbonate are also weak bases, but they differ from aluminum and magnesium hydroxides in being absorbed from the gut. Because of their systemic effects, calcium and 109 bicarbonate salts are less popular as antacids than the magnesium and aluminum compounds listed. Adverse effects : Diarrhea, constipation, phosphate depletion resulting in muscular weakness, osteoporrosis, and renal dysfunction. 7.1.4. MUCOSAL PROTECTIVE AGENTS These compounds, known as cytoprotective compounds, have several actions that enhance mucosal protection mechanisms, thereby preventing mucosal injury, reducing inflammation, and healing existing ulcers. Sucralfate: This complex of aluminum hydroxide and sulfated sucrose binds to positively charged groups in proteins of both normal and necrotic mucosa. By forming complex gels with epithelial cells, sucralfate creates a physical barrier that impairs diffusion of HCl and prevents degradation of mucus by pepsin and acid. It also stimulates prostaglandin release as well as mucus and bicarbonate output, and it inhibits peptic digestion. By these and other mechanisms, sucralfate effectively heals duodenal ulcers and is used in long-term maintenance therapy to prevent their recurrence. Because it requires an acidic pH for activation, sucralfate should not be administered with H2 antagonists or antacids. Little of the drug is absorbed systemically. It is very well tolerated, but it can interfere with the absorption of other drugs by binding to them. This agent does not prevent NSAID-induced ulcers, nor does it heal gastric ulcers. Sucralfate must be taken four times daily. Adverse Effects Sucralfate is too insoluble to have significant systemic effects when taken by the oral route; toxicity is very low. Constipation occurs in 2% of patients due to the aluminum salt. Because a small amount of aluminum is absorbed, it should not be used for prolonged periods in patients with renal insufficiency. Patients complains dry mouth sometimes. 110 Sucralfate may bind to other medications, impairing their absorption. Bismuth subsalicylate: Preparations of this compound effectively heal peptic ulcers. In addition to their antimicrobial actions, they inhibit the activity of pepsin, increase secretion of mucus, and interact with glycoproteins in necrotic mucosal tissue to coat and protect the ulcer crater. Synthetic prostaglandins: Prostaglandin E2, produced by the gastric mucosa, inhibits secretion of HCl and stimulates secretion of mucus and bicarbonate (cytoprotective effect). A deficiency of prostaglandins is thought to be involved in the pathogenesis of peptic ulcers. Misoprostol, a stable analog of prostaglandin E1, as well as some PPIs, are approved for prevention of gastric ulcers induced by NSAIDs. It is less effective than H2 blockers and the PPIs for acute treatment of peptic ulcers. Although misoprostol has cytoprotective actions, it is clinically effective only at higher doses that diminish gastric acid secretion. Routine prophylactic use of misoprostol may not be justified except in patients who are taking NSAIDs and are at high risk of NSAID-induced ulcers, such as the elderly or patients with ulcer complications. Like other prostaglandins, misoprostol produces uterine contractions and is contraindicated during pregnancy. Dose-related diarrhea and nausea are the most common adverse effects and limit the use of this agent. 7.1.5. UPPER GASTROINTESTINAL PROMOTILITY DRUGS Some diseases (diabetes and others) that damage nerves to the viscera frequently cause a marked loss of motility in the esophagus and stomach, resulting in gastric paralysis (gastroparesis). Gastroparesis is associated with delayed stomach emptying, nausea, and severe bloating. Metoclopramide and cisapride are able to stimulate motility in gastroparesis. Metoclopramide probably acts as an acetylcholine facilitator and dopamine receptor antagonist in the enteric nervous system (ENS). Cisapride appears to act as a 5-HT 4 agonist in the ENS. The "prokinetic" action of metoclopramide is also of some value in preventing emesis following surgical 111 anesthesia and emesis induced by cancer chemotherapeutic drugs. Adverse effects of metoclopramide include induction of Parkinsonism and other extrapyramidal effects. Cisapride in high concentrations is associated with long-QT syndrome and has caused fatal arrhythmias. For this reason, cisapride is now available only on a limited basis. A variety of drugs have been found to be of some value in the prevention and treatment of vomiting, especially cancer chemotherapy-induced vomiting. In addition to metoclopramide, useful antiemetic drugs include dexamethasone; some HI antihistamines; several phenothiazines; the 5-HT 3 inhibitors; and a few neuroleptics. The 5-HT 3 inhibitors, ondansetron, granisetron, and dolasetron, are extremely useful in preventing nausea aud vomiting after general anesthesia and in patients receiving cancer chemotherapy. 7.2. DRUGS AFFECTING OTHER GIT ORGANS Pancreatic Enzyme Replacements: Steatorrhea, a condition of decreased fat absorption coupled with an increase in stool fat excretion, results from inadequate pancreatic secretion of lipase. The abnormality of fat absorption can be significantly relieved by oral administration of pancreatic lipase (pancrelipase) obtained from pigs. Pancreatic lipase is inactivated at a pH below 4.0; thus, up to 90% of an administered dose will be destroyed in the stomach, unless the pH is raised with antacids or drugs that reduce acid secretion. Laxatives: Laxatives increase the probability of a bowel movement by several mechanisms: an irritant or stimulant action on the bowel wall; a bulk-forming action on the stool that evokes reflex contraction of the bowel; a softening action on hard or impacted stool; and a lubricating action that eases passage of stool through the rectum. Antidiarrheal agents: The most effective antidiarrheal drugs are the opioids and derivatives of opioids that have been selected for maximal antidiarrheal and minimal CNS effect. Of the latter group, the most important are diphenoxylate and loperamide, meperidine 112 analogs with very weak analgesic effects. Difenoxin, the active metabolite of diphenoxylate, is also available as a prescription medication. Diphenoxylate is formulated with antimuscarinic alkaloids to reduce the already minimal likelihood of abuse; loperamide is formulated alone and sold over the counter as such. Drugs that inhibit the formation of gallstones: The formation of cholesterol gallstones cau be inhibited by several drugs, though none are dramatically effective. Such drugs include the bile acid derivatives (chenodiol and ursodiol). Chenodiol appears to reduce the secretion of bile acids by the liver, while the mechanism of action of ursodiol is unknown. Ursohol (ursodeoxycholic acid) is a naturally occurring bile acid that makes up less than 5% of the circulating bile salt pool in humans and a much higher percentage in bears. After oral administration, it is absorbed, conjugated in the liver with glycine or taurine, and excreted in the bile. Conjugated ursodiol undergoes extensive enterohepatic recirculation. The serum half-life is approximately 100 hours. With long-term daily administration, ursodiol constitutes 30– 50% of the circulating bile acid pool. A small amount of unabsorbed conjugated or unconjugated ursodiol passes into the colon where it is either excreted or undergoes dehydroxylation by colonic bacteria to lithocholic acid, a substance with potential hepatic toxicity. The solubility of cholesterol in bile is determined by the relative proportions of bile acids, lecithin, and cholesterol. Although prolonged ursodiol therapy expands the bile acid pool, this does not appear to be the principal mechanism of action for dissolution of gallstones. Ursodiol decreases the cholesterol content of bile by reducing hepatic cholesterol secretion. Ursodiol also appears to stabilize hepatocyte canalicular membranes, possibly through a reduction in the concentration of other endogenous bile acids or through inhibition of immune-mediated hepatocyte destruction. Ursodiol is used for dissolution of small cholesterol gallstones in patients with symptomatic gallbladder disease who refuse cholecystectomy or who are poor surgical candidates. At a dosage of 10 mg/kg/d for 12–24 months, dissolution occurs in up to half of patients with small (≈ 5–10 mm) noncalcified gallstones. It is also 113 effective for the prevention of gallstones in obese patients undergoing rapid weight loss therapy. Several trials demonstrate that ursodiol 13–15 mg/kg/d is helpful for patients with early-stage primary biliary cirrhosis, reducing liver function abnormalities Adverse Effects Ursodiol is practically free of serious adverse effects. Bile saltinduced diarrhea is uncommon. Unlike its predecessor, chenodeoxycholate, ursodiol has not been associated with hepatotoxicity. 8. NONSTEROIDAL ANTI-INFLAMMATORY DRUGS (NSAID) Inflammation is a normal, protective response to tissue injury caused by physical trauma, noxious chemicals, or microbiological agents. Inflammation is the body's effort to inactivate or destroy invading organisms, remove irritants, and set the stage for tissue reparation. Normally, our immune system can differentiate between self and non-self factors. Inflammatory responses occur in three distinct temporal phases, each apparently mediated by different mechanisms: 1. The acute phase is characterized by transient local vasodilation and increased capillary permeability. 2. The delayed, subacute phase is characterized by infiltration of leukocytes and phagocytic cells. 3. In the chronic proliferative phase, tissue degeneration and fibrosis occur. The NSAIDs including subclass of selective cyclooxygenase-2 (COX-2) inhibitors have anti-inflammatory (modifiers of the inflammatory reaction) analgesic (reduction of certain types of pain, especially inflammation induced) and antipyretic (lowering of body temperature in case of fever) actions. All of the NSAIDs act by inhibiting the synthesis of prostaglandins (PG). Thus, an understanding of NSAIDs requires comprehension of actions and 114 biosynthesis of prostaglandins from unsaturated fatty acid derivatives containing 20 carbons that include a cyclic ring structure. PG's and related compounds are produced in minute quantities by virtually all tissues. They generally act locally on the tissues in which they are synthesized, and they are rapidly metabolized to inactive products at their sites of action. Prostaglandins of the E and F series evoke some of the local and systemic manifestations of inflammation, such as vasodilation, hyperemia, increased vascular permeability, swelling, pain, and increased leukocyte migration. In addition, they intensify the effects of inflammatory mediators, such as histamine, bradykinin, and 5-hydroxytryptamine. Arachidonic acid, a 20-carbon fatty acid, is the primary precursor of the prostaglandins and related compounds. Arachidonic acid is present as a component of the phospholipids of cell membranes. Free arachidonic acid is released from tissue phospholipids by the action of phospholipase A2 and other acyl hydrolases via a process controlled by hormones and other stimuli. There are two major pathways in the synthesis of the eicosanoids from arachidonic acid: Cyclooxygenase- and Lipoxygenase pathways. PGs act primarily by inhibiting the cyclooxygenase enzymes, but not the lipoxygenase enzymes. Cyclooxygenase-2 is a close structural analog of COX-1 and, like the latter, catalyzes the conversion of arachidonic acid to prostaglandin PgH2 via PgG2. These isozymes are encoded by two different genes. COX-1 is generally regarded to be constitutive and COX-2 inducible. However, this is an oversimplification, since COX-2 is produced in the kidney and brain, but is inducible in other sites, including those that are inflamed, such as joints. Nearly all NSAIDs have a greater selectivity for COX-I. They are used primarily for conditions which are not considered inflammatory (for example, headache and analgesia). Their unwanted side effect causing gastric damage is linked to inhibition of COX-l, resulting in an inability to form protective prostaglandins. This led to the search for a COX-2 inhibitor, commonly referred to as a "safe aspirin", reasoning that if 115 COX-1 in the stomach is unaffected by the new drug, then the gastrointestinal effects would be minimized. NSAIDs are a chemically heterogeneous group of compounds, often chemically unrelated (although most of them are organic acids), which nevertheless share certain therapeutic actions and adverse effects. Acetylsalicylic acid (ASA) also inhibits COX enzymes but in a manner which is molecularly distinct from the competitive, reversible, active site inhibitors and is often distinguished from the NSAIDs. Similarly, acetaminophen, which is antipyretic and analgesic but largely devoid of antiinflammatory activity, is also conventionally segregated from the group despite of its sharing NSAID activity with other actions relevant to its clinical action in vivo. General properties shared by ASA, the NSAIDs, and acetaminophen as a class of COX inhibitors are considered first, followed by determination of important differences among representative drugs. Picture 3 - Eicosanoid synthesis pathway (by Charles R. Craig and others) Salicylates and other similar agents used to treat rheumatic disease share the capacity to suppress the signs and symptoms of 116 inflammation. These drugs also exert antipyretic and analgesic effects, but it is their anti-inflammatory properties that make them most useful in the management of disorders in which pain is proportional to the intensity of the inflammatory process. ASA (aspirin) has three therapeutic dose ranges: the low range (< 300 mg/d) is effective in reducing platelet aggregation; intermediate doses (300–2400 mg/d) have antipyretic and analgesic effects; and high doses (2400–4000 mg/d) are used for their antiinflammatory effect. Aspirin is readily absorbed and is hydrolyzed in blood and tissues to acetate and salicylic acid. Salicylate is a reversible nonselective inhibitor of cyclooxygenase. Elimination of salicylate is first-order at low doses, with a half-life of 3 NSAIDs are a chemically heterogeneous group of compounds, often chemically unrelated (although most of them are organic acids), which nevertheless share certain therapeutic actions and adverse effects. Acetylsalicylic acid (ASA) also inhibits COX enzymes but in a manner which is molecularly distinct from the competitive, reversible, active site inhibitors and is often distinguished from the NSAIDs. Similarly, Acetaminophen, which is antipyretic and analgesic but largely devoid of antiinflammatory activity, is also conventionally segregated from the group despite of its sharing NSAID activity with other actions relevant to its clinical action in vivo. General properties shared by ASA, the NSAIDs, and Acetaminophen as a class of COX inhibitors are considered first, followed by determination of important differences among representative drugs.5 hours. At high (anti-inflammatory) doses, half-life increases to 15 hours or more and elimination becomes zeroorder. Excretion is facilitated via the kidneys. The other NSAIDs are well absorbed after oral administration. Ibuprofen has a half-life of about 2 hours, it is relatively safe, and is the least expensive of the older, nonselective NSAIDs. Indomethacin is a potent NSAID with increased toxicity. Naproxen and piroxicam are noteworthy because of their longer half-lives (12–24 hours), which permit less frequent dosing. These other NSAIDs are used for the treatment of mild to moderate pain--and especially inflammatory pain as seen in cases of rheumatoid arthritis and gout. COX-2 117 inhibitors are primarily used in inflammatory disorders. Selected NSAIDs are also used to treat other conditions, including dysmenorrhea, headache, and patent ductus arteriosus in premature infants. Ketorolac is notable as a drug used mainly as a systemic analgesic, but not as an anti-inflammatory drug (though it has typical nonselective NSAID properties). It is the only NSAID available in a parenteral formulation. Although all NSAIDs are not approved for the treatment of whole range of rheumatic diseases, all are probably effective in rheumatoid arthritis, seronegative spondyloarthropathies (e.g., psoriatic arthritis and arthritis associated with inflammatory bowel disease), osteoarthritis, localized musculoskeletal syndromes (eg, sprains and strains, low back pain), and gout (except tolmetin, which appears to be ineffective in gout). Since aspirin, the original NSAID, has a number of adverse effects, many other NSAIDs have been developed in attempts to improve upon aspirin's efficacy and decrease its toxicity. 8.1. CLASSIFICATION OF NSAIDs There are many classifications of this groop – by chemical structure (derivatives), by mechanism of action (central or peripheral action), by selectivness (selective or nonselective), by its negative action at the joints, and so on. It is very important to remember about pharmacokinetic and pharmacodynamic aspects of these drugs in the practical use. This chemical diversity yields a broad range of pharmacokinetic characteristics. Although there are many differences in the kinetics of NSAIDs, they have some general properties in common. All but one of the NSAIDs is a weak organic acid as an exception, nabumetone, which is a ketone prodrug that is metabolized to the acidic active drug. Most of these drugs are well absorbed, and food does not substantially change their bioavailability. Most of the NSAIDs are highly metabolized, some by phase I followed by phase II mechanisms and others by direct glucuronidation (phase II) alone. NSAID metabolism proceeds, in large part, by way of the CYP3A or CYP2C families of P450 118 enzymes in the liver. While renal excretion is the most important route for final elimination, nearly all undergo varying degrees of biliary excretion and reabsorption (enterohepatic circulation). In fact, the degree of lower gastrointestinal tract irritation correlates with the amount of enterohepatic circulation. Most of the NSAIDs are highly protein-bound (~ 98%), usually to albumin. Some of the NSAIDs (e.g., ibuprofen) are racemic mixtures, while one, Naproxen, is provided as a single enantiomer and a few have no chiral center (e.g., diclofenac). All NSAIDs can be found in synovial fluid after repeated dosing. Drugs with short half-lives remain in the joints longer than they would be predicted from their half-lives, while drugs with longer half-lives disappear from the synovial fluid at a rate proportionate to their half-lives. Various NSAIDs have additional possible mechanisms of action, including inhibition of chemotaxis, down-regulation of interleukin-1 production, decreased production of free radicals and superoxide, and interference with calcium-mediated intracellular events. ASA irreversibly acetylates and blocks platelet cyclooxygenase, while most non-COX-selective NSAIDs are reversible inhibitors. Selectivity for COX-1 versus COX-2 is variable and incomplete for the older members, but the highly selective COX-2 inhibitor, celecoxib, is currently available, and other highly selective coxibs are being developed. The highly selective COX-2 inhibitors do not affect platelet function at their usual doses. In testing using human whole blood, aspirin, indomethacin, piroxicam, and sulindac were somewhat more effective in inhibiting COX-1; ibuprofen and meclofenamate inhibited the two isozymes about equally. The efficacy of COX-2-selective drugs equals that of the older NSAIDs, while gastrointestinal safety may be improved. On the other hand, highly selective COX-2 inhibitors may increase the incidence of edema and hypertension. The NSAIDs decrease the sensitivity of vessels to bradykinin and histamine, affect lymphokine production from T lymphocytes, and reverse the vasodilation of inflammation. To varying degrees, all newer NSAIDs are analgesic, anti-inflammatory, and antipyretic, and 119 all (except the COX-2-selective agents and the nonacetylated salicylates) inhibit platelet aggregation. NSAIDs are all gastric irritants as well, although as a group the newer agents tend to cause less gastric irritation than ASA. Nephrotoxicity has been observed for all of the drugs for which extensive experience has been reported, and hepatotoxicity can also occur with any NSAID. Nephrotoxicity is due, in part, to interference with the autoregulation of renal blood flow, which is modulated by prostaglandins. Several NSAIDs (including acethilsalicylic acid) appear to reduce the incidence of colon cancer when taken chronically. Several large epidemiologic studies have shown a 50% reduction in relative risk when the drugs are taken for 5 years or longer. The mechanism for this protective effect is unclear. 8.2. NONSELECTIVE NSAIDs Acetylsalicylic acid (Aspirin)'s long use and availability without prescription diminishes its glamour compared with that of the newer NSAIDs. Aspirin is now rarely used as an anti-inflammatory medication; it has been replaced by Ibuprofen and Naproxen, since they are effective, are also available over the counter, and have good to excellent safety records. Salicylic acid is a simple organic acid. Sodium salicylate and aspirin are equally effective anti-inflammatory drugs, though ASA may be more effective as an analgesic. The salicylates are rapidly absorbed from the stomach and upper small intestine, yielding a peak plasma salicylate level within 1–2 hours. Aspirin is absorbed as such and is rapidly hydrolyzed (serum half-life is 15 minutes) to acetic acid and salicylate by esterases in tissue and blood. Salicylate is bound to albumin, but the binding and metabolism of salicylates are saturable so that the unbound fraction increases as total concentration increases. Beyond a total body load of 600 mg, increases in salicylate dosage increase salicylate concentration disproportionately. As doses of aspirin increase, salicylate elimination half-life increases from 3-5 hours (for 600 mg/d dosage) to 12–16 hours (dosage ≥ 3.6 g/d). Alkalinization of the urine 120 increases the rate of excretion of free salicylate and its water-soluble conjugates. Mechanism of Action A. Anti-inflammatory effects: Aspirin is a nonselective inhibitor of both COX isoforms, but salicylate is much less effective in inhibiting either isoform. Nonacetylated salicylates may work as oxygen radical scavengers. Aspirin irreversibly inhibits COX and inhibits platelet aggregation, while nonacetylated salicylates do not. B. Analgesic effects: Aspirin is most effective in reducing pain of mild to moderate intensity through its effects on inflammation and because it probably inhibits pain stimuli at a subcortical site. C. Antipyretic effects Aspirin's antipyretic effect is probably mediated by both COX inhibition in the central nervous system and inhibition of interleukin-1 (which is released from macrophages during episodes of inflammation). D. Antiplatelet effects: Aspirin irreversibly inhibits platelet COX, so that aspirin's antiplatelet effect lasts 8-10 days (the life of the platelet). Therapeutic uses: Aspirin is employed for mild to moderate pain of varied origin but is not effective for severe visceral pain. Aspirin and other NSAIDs have been combined with opioid analgesics for treatment of cancer pain, where their anti-inflammatory effects act synergistically with the opioids to enhance analgesia. High-dose salicylates are effective for treatment of rheumatic fever, rheumatoid arthritis, and other inflammatory joint conditions. Aspirin has antiplatelet-aggregation action by decreasing acticity of tromboxan system and can be given to prevent of transient ischemic attacks, unstable angina, and coronary artery thrombosis with myocardial infarction. The optimal analgesic or antipyretic dose of aspirin is less than the 0.6-0.65 g oral dose commonly used. The anti-inflammatory dose for children is 50–75 mg/kg/d in divided doses, and the average starting anti-inflammatory dose for adults is 45 mg/kg/d in divided doses. 121 Adverse Effects At the usual dosage, aspirin's main adverse effects are gastric and duodenal ulcers; hepatotoxicity, asthma, rashes, and renal toxicity occur less frequently. A dose-related increase in fecal blood loss is routinely associated with aspirin administration, although some mucosal adaptation occurs in many patients, so that blood loss declines back to baseline over 4–6 weeks. With higher doses, patients may experience “salicylism” - vomiting, tinnitus, decreased hearing, and vertigo - reversible by reducing the dosage. Still larger doses of salicylates cause hyperpnea through a direct effect on the medulla. At toxic salicylate levels, respiratory alkalosis followed by metabolic acidosis (salicylate accumulation), respiratory depression, and even cardiotoxicity and glucose intolerance can occur. Like other NSAIDs, aspirin can cause elevation of liver enzymes (a frequent but mild effect), hepatitis (rare), decreased renal function, bleeding, rashes, and asthma. The antiplatelet action of aspirin contraindicates its use by patients with hemophilia. Although previously not recommended during pregnancy, aspirin may be valuable in treating preeclampsiaeclampsia. 8.2.1. OTHER NONSELECTIVE DRUGS Like aspirin, these agents may cause significant gastrointestinal disturbance, but the incidence is lower than with aspirin. There is a significant risk of renal damage with any of the NSAIDs, especially in patients with preexisting renal disease. Since these drugs are cleared by the kidney, renal damage results in higher, more toxic serum concentrations. Phenylbutazone, an older NSAID, should not be used chronically because it causes aplastic anemia and agranulocytosis. Serious hematologic reactions have also been noted with indomethacin. 1. Diclofenac: Diclofenac is a phenylacetic acid derivative that is relatively nonselective as a COX inhibitor. 122 Adverse effects occur in approximately 20% of patients and include gastrointestinal distress, occult gastrointestinal bleeding, and gastric ulceration, though ulceration may occur less frequently than with some other NSAIDs. A preparation combining diclofenac and misoprostol decreases upper gastrointestinal ulceration but may result in diarrhea. Another combination of diclofenac and omeprazole was also effective with respect to the prevention of recurrent bleeding, but renal adverse effects were common in highrisk patients. Diclofenac at a dose of 150 mg/d appears to impair renal blood flow and glomerular filtration rate. Elevation of serum aminotransferases may occur more commonly with this drug than with other NSAIDs. A 0.1% ophthalmic preparation is recommended for prevention of postoperative ophthalmic inflammation and can be used after intraocular lens implantation and strabismus surgery. A topical gel containing 3% diclofenac is effective for solar keratoses. Diclofenac in rectal suppository form can be considered a drug of choice for preemptive analgesia and postoperative nausea. In Europe, diclofenac is also available as an oral mouthwash and for intramuscular administration. 1. Etodolac is a racemic acetic acid derivative with an intermediate half-life. It is slightly more COX-2-selective than most other NSAIDs, with a COX-2:COX-1 activity ratio of about 10. Unlike many other racemic NSAIDs, etodolac does not undergo chiral inversion in the body. The dosage of etodolac is 200-400 mg three to four times daily. Etodolac provides good postoperative pain relief after coronary artery bypass operations, although transient impairment of renal function has been reported. There are no data to suggest that etodolac differs significantly from other NSAIDs except in its pharmacokinetic parameters, though it has been claimed to cause less gastric toxicity in terms of ulcer disease than other nonselective NSAIDs. 2. Although diflunisal is derived from salicylic acid, it is not metabolized to salicylic acid or salicylate. It undergoes an enterohepatic cycle with absorption of its glucuronide metabolite followed by cleavage of the glucuronide to liberate again the active 123 moiety. Diflunisal is a subject to capacity-limited metabolism, with serum half-lives at various dosages approximating that of salicylates. In rheumatoid arthritis the recommended dosage is 500–1000 mg daily in two split dosages. It is claimed to be particularly effective for cancer pain with bone metastases and for pain control in dental (third molar) surgery. A 2% diflunisal oral ointment is a clinically useful analgesic for painful oral lesions. Adverse effects: Because its clearance depends on renal function as well as hepatic metabolism, diflunisal's dosage should be limited in patients with significant renal impairment. Its adverse event profile is similar to those of other NSAIDs; pseudoporphyria has also been reported. 3. Fenoprofen, a propionic acid derivative, is the NSAID most closely associated with interstitial nephritis and is rarely used. Its other toxicities mirror those of other NSAIDs. 4. Flurbiprofen is a propionic acid derivative with a possibly more complex mechanism of action than other NSAIDs. Hepatic metabolism is extensive; its (R)(+) and (S)(-) enantiomers are metabolized differently, and it does not undergo chiral conversion. It does demonstrate enterohepatic circulation. The efficacy of flurbiprofen at dosages of 200–400 mg/d is comparable to that of aspirin and other NSAIDs in clinical trials for patients with rheumatoid arthritis, ankylosing spondylitis, gout, and osteoarthritis. It is also available in a topical ophthalmic formulation for inhibition of intraoperative miosis. Flurbiprofen intravenously has been found to be effective for perioperative analgesia in minor ear, neck, and nose surgery and in lozenge form for sore throat. Although its adverse effect profile is similar to that of other NSAIDs in most ways, flurbiprofen is also associated rarely with cogwheel rigidity, ataxia, tremor, and myoclonus. 5. Ibuprofen is a simple derivative of phenylpropionic acid. In doses of about 2400 mg daily, ibuprofen is equivalent to 4 g of aspirin in anti-inflammatory effect. Oral ibuprofen is often prescribed in lower doses (<2400 mg/d), at which it has analgesic but not anti-inflammatory efficacy. It is available over the counter in low-dose forms under several trade 124 names. A topical cream preparation appears to be absorbed into fascia and muscle; an (S) (-) formulation has been tested. Ibuprofen cream was more effective than placebo cream for the treatment of primary knee osteoarthritis. A liquid gel preparation of ibuprofen 400 mg provides prompt relief and good overall efficacy in postsurgical dental pain. In comparison with indomethacin, ibuprofen decreases urine output less and also causes less fluid retention than indomethacin. Ibuprofen is effective in closing patent ductus arteriosus in preterm infants with much the same efficacy and safety as indomethacin. The oral and intravenous routes are equally effective for this indication. Adverse effects: Gastrointestinal irritation and bleeding occur, although less frequently than with aspirin. The use of ibuprofen concomitantly with aspirin may decrease the total anti-inflammatory effect. The drug is relatively contraindicated in individuals with nasal polyps, angioedema, and bronchospastic reactivity to aspirin. In addition to the gastrointestinal symptoms (which can be modified by ingestion with meals), rash, pruritus, tinnitus, dizziness, headache, aseptic meningitis (particularly in patients with systemic lupus erythematosus), and fluid retention have been reported. Interaction with anticoagulants is uncommon. The concomitant administration of ibuprofen antagonizes the irreversible platelet inhibition induced by aspirin. Thus, treatment with ibuprofen in patients with increased cardiovascular risk may limit the cardioprotective effects of aspirin. Rare hematologic effects include agranulocytosis and aplastic anemia. Effects on the kidney (as with all NSAIDs) include acute renal failure, interstitial nephritis, and nephrotic syndrome, but these occur very rarely. Finally, hepatitis has been reported. 6. Indomethacin, introduced in 1963, is an indole derivative. It is a potent nonselective COX inhibitor and may also inhibit phospholipase A and C, reduce neutrophil migration, and decrease T cell and B cell proliferation. Probenecid prolongs indomethacin's half-life by inhibiting both renal and biliary clearance. It differs somewhat from other NSAIDs in its indications and toxicities. 125 Indomethacin is indicated for use in rheumatic conditions and is particularly popular for gout and ankylosing spondylitis. In addition, it has been used to treat patent ductus arteriosus. Indomethacin has been tried in numerous small or uncontrolled trials for many other conditions, including Sweet's syndrome, juvenile rheumatoid arthritis, pleurisy, nephrotic syndrome, diabetes insipidus, urticarial vasculitis, postepisiotomy pain, and prophylaxis of heterotopic ossification in arthroplasty. An ophthalmic preparation seems to be efficacious for conjunctival inflammation and to reduce pain after traumatic corneal abrasion. Gingival inflammation is reduced after administration of indomethacin oral rinse. Epidural injections produce a degree of pain relief similar to that achieved with methylprednisolone in postlaminectomy syndrome. Adverse effects: At higher dosages, at least a third of patients have reactions to indomethacin requiring discontinuance. The gastrointestinal effects may include abdominal pain, diarrhea, gastrointestinal hemorrhage, and pancreatitis. Headache is experienced by 15–25% of patients and may be associated with dizziness, confusion, and depression. Rarely, psychosis with hallucinations has been reported. Hepatic abnormalities are rare. Serious hematologic reactions have been noted, including thrombocytopenia and aplastic anemia. Hyperkalemia has been reported and is related to inhibition of the synthesis of prostaglandins in the kidney. Renal papillary necrosis has also been observed. A number of interactions with other drugs have been reported. 7. Ketoprofen is a propionic acid derivative that inhibits both COX (nonselectively) and lipoxygenase.. Concurrent administration of probenecid elevates ketoprofen levels and prolongs its plasma half-life. The effectiveness of ketoprofen at dosages of 100–300 mg/d is equivalent to that of other NSAIDs in the treatment of rheumatoid arthritis, osteoarthritis, gout, dysmenorrhea, and other painful conditions. In spite of its dual effect on prostaglandins and leukotrienes, ketoprofen is not superior to other NSAIDs. Its major adverse effects are on the gastrointestinal tract and the central nervous system. 126 8. Ketorolac is an NSAID promoted for systemic use mainly as an analgesic, not as an anti-inflammatory drug (although it has typical NSAID properties). The drug is an effective analgesic and has been used successfully to replace morphine in some situations involving mild to moderate postsurgical pain. It is most often given intramuscularly or intravenously, but an oral dose formulation is available. When used with an opioid, it may decrease the opioid requirement by 25–50%. An ophthalmic preparation is available for ocular inflammatory conditions. Toxicities are similar to those of other NSAIDs, although renal toxicity may be more common with chronic use. 9. Meclofenamate and mefenamic acid inhibit both COX and phospholipase A2. They are rarely used today. 10. Naproxen is a naphthylpropionic acid derivative. It is the only NSAID presently marketed as a single enantiomer, and it is a nonselective COX inhibitor. Naproxen's free fraction is significantly higher in women than in men, although albumin binding is very high in both sexes. Naproxen is effective for the usual rheumatologic indications and is available both in a slow-release formulation and as an oral suspension. A topical preparation and an ophthalmic solution are also available. The incidence of upper gastrointestinal bleeding in over-thecounter use is low but still doubles that of over-the-counter ibuprofen (perhaps due to a dose effect). Rare cases of allergic pneumonitis, leukocytoclastic vasculitis, and pseudoporphyria as well as the more common NSAID-associated adverse effects have been noted. 11. Piroxicam, an oxicam, is a nonselective COX inhibitor that at high concentrations also inhibits polymorphonuclear leukocyte migration, decreases oxygen radical production, and inhibits lymphocyte function. Its long half-life permits once-daily dosing. Piroxicam can be used for the usual rheumatic indications. Toxicity includes gastrointestinal symptoms (20% of patients), dizziness, tinnitus, headache, and rash. When piroxicam is used in dosages higher than 20 mg/d, an increased incidence of peptic ulcer and bleeding is encountered. Epidemiologic studies suggest that this 127 risk is as much as 9.5 times higher with piroxicam than with other NSAIDs. 12. Sulindac is a sulfoxide prodrug. It is reversibly metabolized to the active sulfide metabolite, which is excreted in bile and then reabsorbed from the intestine. The enterohepatic cycling prolongs the duration of action to 12–16 hours. The indications and adverse reactions of sulindac are similar to those of other NSAIDs. In addition to its rheumatic disease indications, sulindac suppresses familial intestinal polyposis; it may inhibit the development of colon, breast, and prostate cancer in humans. It appears to inhibit the occurrence of gastrointestinal cancer in rats. The latter effect may be caused by the sulfone rather than the sulfide. Adverse effects: Stevens-Johnson epidermal necrolysis syndrome, thrombocytopenia, agranulocytosis, and nephrotic syndrome have all been observed. Like diclofenac, sulindac may have some propensity to cause elevation of serum aminotransferases; it is also sometimes associated with cholestatic liver damage, which disappears or becomes quiescent when the drug is stopped. 8.3. COX-2-SELECTIVE INHIBITORS The COX-2-selective inhibitors may have a reduced risk of gastrointestinal effects, including gastric ulcers and serious gastrointestinal bleeding. Celecoxib is a sulfonamide and may cause a hypersensitivity reaction in patients who are allergic to other sulfonamides. 1. Celecoxib is a highly selective COX-2 inhibitor – about 10–20 times more selective for COX-2 than for COX-1. Celecoxib is as effective as other NSAIDs in rheumatoid arthritis and osteoarthritis, and in trials it has caused fewer endoscopic ulcers than most other NSAIDs. Because it is a sulfonamide, celecoxib may cause rashes. It does not affect platelet aggregation. It interacts occasionally with warfarin – as would be expected of a drug metabolized via CYP2C9. The coxibs continue to be investigated to determine whether their effect on prostacyclin production could lead to a prothrombotic state. 128 The frequency of other adverse effects approximates that of other NSAIDs. Celecoxib causes no more edema or renal effects than other members of the NSAID group, but edema and hypertension have been documented. 2. Meloxicam is an enolcarboxamide related to piroxicam that has been shown to preferentially inhibit COX-2 over COX-1, particularly at its lowest therapeutic dose of 7.5 mg/d. It is not as selective as the other coxibs. The drug is popular in Europe and many other countries for most rheumatic diseases and has recently been approved for treatment of osteoarthritis in the USA. Its efficacy in this condition and rheumatoid arthritis is comparable to that of other NSAIDs. It is associated with fewer clinical gastrointestinal symptoms and complications than piroxicam, diclofenac, and naproxen. Similarly, while meloxicam is known to inhibit synthesis of thromboxane A2, it appears that even at supratherapeutic doses, its blockade of thromboxane A2 does not reach levels that result in decreased in vivo platelet function. Other toxicities are similar to those of other NSAIDs. 3. Rofecoxib, a furanose derivative, is a potent, selective COX-2 inhibitor. Rofecoxib is approved for osteoarthritis and rheumatoid arthritis, and it also appears to be analgesicand antipyretic – in common with other NSAIDs. This drug does not inhibit platelet aggregation and appears to have little effect on gastric mucosal prostaglandins or lower gastrointestinal tract permeability. At high doses it is associated with occasional edema and hypertension. Other toxicities are similar to those of other coxibs. 8.4. PRINCIPLES OF THE PRACTICAL USE The choice of an NSAID thus requires a balance of efficacy, costeffectiveness, safety, and numerous personal factors (e.g., other drugs also being used, concurrent illness, compliance, medical insurance coverage), so that there is no best NSAID for all patients. There may, however, be one or two best NSAIDs for a specific person. 129 Contraindications and Drug Interactions: Co-morbid factors that increase the risk of NSAID-induced GI bleeding include history of ulcer disease, advanced age, poor health status, treatment with certain drugs, and long duration of NSAID therapy, smoking, and heavy alcohol use. Because of their renal effects, NSAIDs must be used with caution in patients with renal impairment, heart failure, hypertension, and edema. The use of NSAIDs is contraindicated in persons who have had a hypersensitivity reaction to salicylates or any other NSAIDs. Asthmatics are at particular risk for these reactions. NSAIDs should be used during pregnancy only if the potential benefit justifies the risk to the fetus. Because NSAIDs decrease prostaglandin synthesis in the kidney, these drugs can increase the nephrotoxicity of agents, such as aminoglycosides, amphotericin B, cidofovir, cisplatin, cyclosporine, foscarnet, ganciclovir, pentamidine, and vancomycin. NSAIDs can decrease the renal excretion of drugs such as lithium. NSAIDs can decrease the effectiveness of antihypertensive drugs, such as β-blockers and water pills. 130 REFERENCES 1. Bertram G. K. Basic and Clinical Pharmacology : textbook / Bertram G. Katzung. – 10th edition. – San Francisco : McGraw-Hill Companies, 2007. – 1200 p. 2. Goodman S. The pharmacological basis of therapeutics / S. Goodman, A. Gilman. – 9th edition. – New York : McGraw-Hill, 1996. – 1811 p. 3. Harvey R. A. Pharmacology / A. Richard Harvey, Pamela C. Chempe – 2nd edition. – Lippincott Williams & Wilkins, 1997. – 564 p. 4. Kresyun V. A. General pharmacology : cource of lectures / V. A. Kresyun, D. Yu. Andronov, K. F. Shemonaeva. – Odessa : OSMU, 2005. – 215 p. 5. Pharmacology : textbook / I. S. Chekman, N. O. Gorchakova, N. I. Panasenko, P. O. Bekh. – Vinnytsya : NOVA KNYHA Publishers, 2006. – 384 p. 6. Polevik I. V. Lectures on Pharmacology: For the Foreign Students Being Educated in English / I. V. Polevik, A. I. Beketov, M. G. Kurchenko. – Simferopol : Вид-во «Симферопільська міська типографія», 2003. – Part 1. – 100 p. 7. Polevik I. V. Lectures on Pharmacology: For the Foreign Students Being Educated in English / I. V. Polevik, A. I. Beketov, M. G. Kurchenko. – Simferopol : Вид-во «Симферопільська міська типографія», 2003. – Part 2. – 108 p. 8. Stefanov O. Pharmacology with General Prescription : textbook / O. Stefanov, V. Kurcher. – К. : Вид-во «Ельіньо». – 2004. – 156 p. 9. Stefanov O. Pharmacology with General Prescription : textbook / O. Stefanov, V. Kurcher. – К. : Вид-во «Ельіньо». – 2007. – 318 p. 10. Vysotsky I. Yu. Drugs affecting peripheral nervous system: for foreign students being educated in English / I. Yu. Vysotsky, R. A. Chramova, A. A. Kachanova. – Sumy : Sumy State Univer-sity Publishers, 2009. – 62 p. 11. Vysotsky I. Yu. Medical Prescription (for foreign students being educated in English) / I. Yu. Vysotsky, R. A. Chramova, A. A. Kachanova. – Sumy : Sumy State University Publishers, 2008. – 40 p. 12. Газій T. В. Study guide to basic pharmacology : навчальний посібник / T. В. Газій. – Харків : “Факт”, 2005. – 126 c. 131 CONTENTS P. 1. GENERAL PRINCIPLES OF CLINICAL PHARMACOLOGY ........ 3 1.1. Principles of Pharmacokinetics and Pharmacodynamics .......... 3 1.2. Routes of Administration .......................................................... 5 1.3. Drugs Interections ..................................................................... 6 2. ANTIHYPERTENSIVE AGENTS ...................................................... 9 2.1. General Principles of Hypertention Treatment ......................... 9 2.2. Clinical Uses of Antihypertensive Drugs................................ 12 2.3. Classification of Antihypertensive Drugs ............................... 13 2.3.1. Diuretics ................................................................................. 15 2.3.2. Inhibitors of the Renin-Angiotensin System ......................... 18 2.3.3. Angiotensin II Receptor Antagonists ..................................... 26 2.3.4. Antiadrenergics Drugs ........................................................... 30 2.3.5. Calcium-Channel Blockers (the Calcium Slow Channel Blocking Agents) ................................................................... 38 2.4. Second Line Therapy .............................................................. 41 2.4.1. Ganglionic Blocking Agents ................................................. 41 2.4.2. Alpha 1-Blockers .................................................................. 42 2.4.3. Vasodilators .......................................................................... 43 2.4.4. Centrally Acting Adrenergic Drugs ....................................... 45 2.4.5. Hypertensive Emergency ....................................................... 47 3. ANTIANGINAL DRUGS .................................................................. 48 3.1. General Principles in the Treatment of Ischemic Heart Disease (IHD) ......................................................................... 48 3.2. Organic Nitrates ..................................................................... 52 3.3. Myocardial Infarction ............................................................ 57 4. ANTIHYPERLIPEDEMIC DRUGS .................................................. 58 4.1. Principles of Treatment in Accordance With the Types of Dyslipidemia....................................................................... 59 4.2. HMG CoA Reductase Inhibitors ............................................ 62 4.3. Niacin (Nicotinic Acid)........................................................... 65 4.4. Fibric Acid Derivatives ( Fibrates ) ........................................ 66 4.5. Bile Acid Binding Resins........................................................ 68 4.6. Cholesterol Absorption Inhibitors .......................................... 69 4.7. Combination Drug Therapy ................................................... 70 5. DRUGS FOR ASTHMA OR COPD TREATMENT ......................... 71 5.1. General Principles in the Treatment of Bronchial Obstructive Syndrome ............................................................ 72 132 5.2. Adrenomimetics ..................................................................... 73 5.3. Antimuscarinic Agents............................................................ 74 5.4. Corticostroids .......................................................................... 76 5.5. Mat Cell Stabilizers ................................................................ 78 5.6. Leukotriene Modulators .......................................................... 79 5.7. Methylxantine Drugs .............................................................. 79 6. GENERAL PRINCIPLES OF ANTIMICROBIAL THERAPY ........ 80 6.1. Bet-Lactam Compounds and Other Cell Wall Inhibitors........ 81 6.2. Protein Synthesis Inhibitors .................................................... 90 6.3. Miscellaneous Antibacterial Agents ....................................... 97 6.4. Antimicrobial Agents Affecting Topoisomerase .................... 98 6.5. Antifolate Drugs ................................................................... 100 7. DRUGS USED IN THE TREATMENT OF GIT DISORDERS ..... 103 7.1. General Principles in the Treatment of Peptic Ulcer Disease ................................................................................. 103 7.1.1. Inhibitors of the H+/K+-ATPase Proton Pump ................... 106 7.1.2. H2-Receptor Antagonists ..................................................... 107 7.1.3. Antacids ............................................................................... 109 7.1.4. Mucosal Protective Agents .................................................. 110 7.1.5. Upper Gastrointestinal Promotility Drugs ........................... 111 7.2. Drugs Affecting Other GIT Organs ..................................... 112 8. NONSTEROIDAL ANTI-INFLAMMATORY DRUGS ............... 114 8.1. Classification of NSAIDs ..................................................... 118 8.2. Nonselective NSAIDs ........................................................... 120 8.2.1. Other Nonselective Drugs .................................................... 122 8.3. COX-2-Selective Inhibitors .................................................. 128 8.4. Principels of the Practical Use .............................................. 129 References ............................................................................................. 131 Contents ................................................................................................. 132 133 Навчальне видання Методичні вказівки для самостійного вивчення курсу «Клінічна фармакологія лікарськіх засобів, що використовуються в лікуванні внутрішніх хвороб» для іноземних студентів спеціальності 7.110101 «Лікувальна справа» денної форми навчання (Англійською мовою) Відповідальний за випуск І. Ю. Висоцький Редактор С. В. Чечоткіна Комп’ютерне верстання А. O. Рощупкін Підписано до друку 17.08.2015, поз. Формат 60х84/16. Ум. друк. арк. 7,91. Обл.-вид. арк. 8,20. Тираж 100 пр. Зам. № Собівартість видання грн к. Видавець і виготовлювач Сумський державний університет, вул. Римського-Корсакова, 2, м. Суми, 40007 Свідоцтво суб’єкта видавничої справи ДК № 3062 від 17.12.2007. 134 Міністерство освіти і науки України Міністерство охорони здоров’я України Сумський державний університет До друку та в світ дозволяю на підставі «Єдиних правил» п. 2.6.14 Начальник організаційно-методичного управління В.Б. Юскаєв CLINICAL PHARMACOLOGY OF DRUGS USED IN TREATMENT OF INTERNAL DISSEASES Клінічна фармакологія лікарськіх засобів що використовуються в лікуванні внуришніх хвороб Усі цитати, цифровий та фактичний матеріал, бібліографічні відомості перевірені, запис одиниць відповідає стандартам Укладач Відповідальний за випуск Директор медичного інституту Сум ДУ А.О. Рощупкін І.Ю. Висоцький В.А. Сміянов 135