The Food Hygiene
advertisement

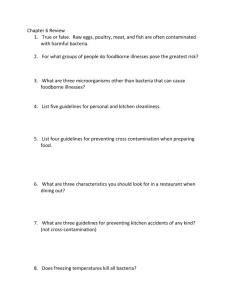
`Food Safety Matters’: Work Pack 2013 1 bettertogether Contents Page Introduction 3 What the Law says 4 The history of food safety 5 What is food safety? 6 Importance of Food Safety 6 What is food poisoning? 6 Food Safety Hazards 7 - Microbiological hazards Chemical hazards Allergenic hazards Physical hazards 7 13 13 14 The main causes of food poisoning 14 Visual signs of poor hygiene conditions 15 The Four C’s 15 - Cleaning Cooking Chilling Cross-Contamination 15 16 16 16 Food safety in the community 17 Food at work and you 18 Overview of strategies to prevent food poisoning 20 Summary: Prevention of Food Poisoning 22 References 23 2 Introduction It has been suggested that in the UK 5.5 million people contract food-borne illnesses each year. Most of us experience food poisoning when we are in a fit and healthy state and so, by and large, we manage to survive. This is not always the case for vulnerable and ill people who are at a higher risk of contracting food-borne illnesses and becoming seriously unwell. Food hygiene and food safety is therefore an area of extreme importance. The potential risk for food poisoning is enormous, and when things do go wrong the consequences can lead to serious illness and deaths, possibly involving large numbers of people. People receiving healthcare and requiring food want to be assured that what they are eating is safe and not contaminated. Food Hygiene is therefore about measures taken to ensure food is wholesome and safe. It is a requirement under the Food Hygiene Regulation 2006 (Regulation (EC) No. 852/2004 on hygiene of food stuffs and The Food Hygiene (England No. 2) Regulations Great Britain 2006) that all ‘food handlers’ are either supervised, instructed and/or trained in food hygiene practices commensurate with their work. A ‘food handler’ is defined as anyone involved in the food service operation including storage, preparation, transportation and serving of food and drink whether open (unwrapped) or packaged. Food includes drinks, ice infant feeds including artificial formula and expressed breast milk. As a student, you may be responsible for the preparation, cooking/reheating or serving of food eaten by service users. Failure to handle food correctly can result in legal action being taken against the organisation and the individual member(s) of staff concerned. As a food handler, you must maintain a high standard of personal hygiene. Also, remember that you have a legal duty to ensure that this food is safe to eat and free from contamination. All people working in a food handling area must wear suitable protective clothing. The standards of clothing may differ depending upon the duties being carried out. However, the following are considered as a minimum requirement: Personnel preparing open food must wear a clean, uniform or similar, plus a disposable apron Do not wear uniforms when travelling to work As a ‘food handler’ you must also practice good personal and hand hygiene. This includes: Ensuring they have clean hands when handling food. Wearing aprons as per NPSA (2007) colour coding for handling and distributing food. No smoking – many health and social care organisations are smoke-free. No eating or drinking whilst handling food. Not wearing jewellery (a plain band ring is acceptable), false nails or nail varnish. Covering wounds likely to cause risk of contamination of foods. Staff who report for duty with a dressing on should have it changed before they enter a food area. Any loss of dressings must be reported immediately. Employees with open wounds must be excluded from food handling areas e.g. production kitchen/ward kitchen. Food handlers known or suspected of having or carrying, any food transmitted disease must be prohibited from practising if there is a risk of cross-contamination with pathogenic micro-organisms. Personal illness MUST be reported because food poisoning bacteria can be carried on/in the body and thereby passed to food. Students must always report immediately illnesses to the relevant Clinical Team Leader, Practice Support Line (PPO) and the Occupational Health Department. These include: Diarrhoea Vomiting Septic conditions Skin infections 3 This work package begins with a discussion regarding various organisms that cause foodborne illness in humans and their epidemiology. It will also explore how organisms are transmitted and address prevention and control measures to assure food safety. This work package is designed to outline the practical methods of handling food in order to minimise risk of contamination and therefore food borne illness. Throughout this work package, you will be asked to think about how this information can be used when you are handling food, and to identify situations that reflect the topic being discussed. These will be found in shaded boxes. You are required to complete these activities and put your completed book and print out from your MCQ into your practice portfolio. Once you have completed the MCQ, please print two copies of your MCQ results (you must gain 85% to pass). Please give one print out to your Academic Personal Tutor and show your practice mentor your completed workbook and your print out of attaining 85% for your MCQ. You can access the MCQ from the Clinical Skills pages at http://learntech.uwe.ac.uk/cs/food-hygiene.aspx you will need to log in with your password. The test is found in the MCQ file on the left hand menu. Studying and completing the exercises will help you to: – comply with the law – demonstrate safe standards of practice – Maintain the safety and well-being of service users – protect your organisation and Profession’s reputation What the Law Says Keeping food safe is a legal requirement and failure to do so can lead to prosecution. It is essential that food and drink provided in the community and hospital health care environment is managed and handled in a manner that it does not pose any risk to children, families, visitors or staff. All staff involved in working with food must ensure good food hygiene practices at all times. Under the Food Safety Act (GB 1990), water and ice are classed as food and therefore must be handled with the same good food hygiene practices as food. Failure to do so could result in a serious outbreak of food poisoning and potential loss of life. Following the food poisoning outbreak at Stanley Royal Hospital in August 1984, Crown Immunity was lifted from NHS hospitals in February 1987. Consequently ALL ASPECTS of hospital catering are now subject to control under the Law. Under the Health and Social Care Act (GB 2008), The Code of Practice for the NHS on the prevention and control of healthcare associated infections it is a requirement that there is a food hygiene policy within Hospitals and Community HealthTrusts. The Food Hygiene (England) Regulations 2006 provide the framework for the EU legislation to be enforced in England. There are similar regulations in Wales, Scotland and Northern Ireland. The Food Safety (General Food Hygiene) Regulations 1995 and the Food Safety (Temperature Control) Regulations 1995 do not apply anymore. Many of the requirements of these regulations are included in the new EU legislation. The main new requirement is to have 'food safety management procedures' and keep up-to-date records of these. The Food Hygiene (England) Regulations (GB 2006) requires that all food business operators shall put into place, implement and maintain a permanent procedure based on the principles of Hazard Analysis Critical Control Points (HACCP). The HACCP principles referred to consist of the following; Penalties under the Act Unlimited fines or up to 2 years imprisonment or both, could be imposed on the responsible employee and his or her superiors. It is therefore vital for all concerned that every effort is made to avoid an offence. Defence to Charges under the Act To properly defend a possible charge under the Act, we must be able to prove ‘due diligence’. The three basic EU food hygiene regulations are: 4 Regulation (EC) 852/2004 on the hygiene of foodstuffs (EU 2004) Regulation (EC) 853/2004 laying down specific hygiene rules for food of animal origin (EU 2004) Regulation (EC) 854/2004 laying down specific rules for the organisation of official controls on products of animal origin intended for human consumption (EU 2004) Managers must put in place ‘food safety management procedures’ based on the principles of HACCP (hazard analysis and critical control point). HACCP is a way of managing food safety. It is based on putting in place procedures to control hazards. In practice, this means that you must follow the procedures that have been put in place to manage food safety ‘hazards’ in your Trust. The Local Authority Environmental Health Officer has open access to all Trusts and can inspect these areas at any time. All ward kitchens and ward refrigerators are bound by legal requirements and therefore are subject to, and must conform to Food Hygiene Regulations. Documented systems must be in place such as the ‘Safer Food Better Business Package’ (FSA 2010) The History of Food safety During the early 20th century, contaminated food, milk and water caused many foodborne infections. The ‘sanitary revolution’ began in an attempt to eliminate disease organisms before they reached consumers. Public health departments or sanitation boards helped institute sewage and water treatment facilities in the early 1900’s in many cities throughout the UK (figure 1). The sanitary revolution included; Sewage and water treatment Hand-washing, sanitation Pasteurization of milk was developed in 1864 and used in milk in 1908 to decrease pathogen load Refrigeration became available for household use in 1913 which helped decrease the growth of foodborne pathogens in the home Before vaccines or antibiotics were discovered, these were the prevention methods taken. Once microbiology methods were improved, the etiology, characteristics, and sources of foodborne diseases were able to be identified. Animals identified as a source of foodborne pathogens Improved animal care and feeding Improved carcass processing Improvements were made regarding healthier animal care, feeding and carcass processing. These measured improved the quality of the food supply. Improved surveillance, research and outbreak investigations have helped discover mechanisms of contamination and led to new control measures through Laws and policies regarding food handling The various laws and policies that have been implemented to improve food handling that you were introduced to in the last section, will be discussed further in the epidemiology and prevention/control sections of this work package. Figure 1: Early 1900 Sanitation Boards 5 What is Food safety? Food Safety is the action of keeping food free from harm. It is the process of storing, preparing, cooking and serving ‘safe’ food. Who Cares and Why? Saves organisations money in the long run Avoids you poisoning your service users Food safety standards increase Ensures you are compliant with the Law Food quality standards increase Organises your process to produce safe food Organises staff promoting teamwork/efficiency Due diligence defence in court Importance of Food Safety Every year thousands of people experience food borne illness often described as food poisoning, which can be extremely unpleasant and in some cases life threatening. Particular care needs to be taken when preparing, cooking and serving food to service users as they are vulnerable to harmful microorganisms and other hazards. This may be because they are either; Neonates Under 2 years of age Immuno-compromised Acutely ill Receiving antibiotics and/or steroid medication Of course anyone can become ill from contaminated food; you might have had food poisoning at some time in your life. Food poisoning is easy to prevent. What is Food Poisoning? Food borne illness or food poisoning is an illness caused from consuming food that contains a harmful substance, harmful micro-organisms or their toxins. This normally results in some of the following symptoms: Abdominal pain/cramps Diarrhoea Nausea Vomiting Fever Dizziness Headaches Flu-like symptoms These normally occur between 2-48 hours after eating contaminated food. However, some viruses and bacteria may multiply and symptoms may take days or even weeks to show. Most often food poisoning results in symptoms which pass reasonably quickly, within a few days. Sometimes the symptoms result in more acute illness which can be very unpleasant, even leading to long-term illness. There are approximately 5.4 million cases per year in UK, and death occurring in 200 severe cases per year. One of the unique factors of foodborne diseases is the variability in incubation times (period from exposure to the pathogen to the demonstration of clinical signs) of the organisms – see figure 2 below. 6 Figure 2: Usual incubation period ranges for select foodborne diseases Food Safety Hazards A hazard is something that could be dangerous. And there are lots of different hazards. When we are talking about hazards in relation to food, a hazard is something that could mean that food will not be safe to eat. The four main food safety hazards that can make food potentially harmful are; Microbiological & Toxins Chemical Allergenic Physical Microbiological Hazards Some micro-organisms are used to make foods such as yoghurt and bread. These microorganisms are not harmful. The micro-organisms that can make us sick include: Viruses e.g. Rotavirus, Caliciviruses (better known as Norovirus or Norwalk viruses) Bacteria e.g. Salmonella, E. coli, Listeria Parasites e.g. Toxoplasma gondii, Trichinella spiralis Mould e.g. Aspergillus flavus Micro-organisms such as viruses and bacteria are the most common causes of food poisoning. But, parasites, natural and manufactured chemicals, and toxins from organisms can also cause food poisoning. However, bacteria are the most common cause. These micro-organisms include; Food spoilage bacteria: may cause food to smell or taste ‘off’ or change texture or colour. This results in food being inedible. See figure 3 below. Figure 3: 7 Food borne virus: these may use food as a mode of transfer, once inside the body, they multiply and cause illness. For example, Norovirus (Norwalk) is a common virus which can be transferred of food and food surfaces. Remember, viruses do not require food or moisture to survive, but are controlled by good hygiene techniques outlined in this work package. Moulds and yeasts: may grow in food and change its appearance or taste. These contaminate food and can make it unusable. Pathogenic bacteria are the main concern of food safety. There are an estimated 250 pathogens that can cause foodborne related illnesses. Foodborne illness is defined as two or more cases of a similar illness resulting from ingestion of a common food. It can result from consuming foods contaminated with various pathogens. In most cases bacteria are the major pathogen followed by viruses, then parasites. The most commonly recognized foodborne infections are caused by Campylobacter, Salmonella, E. coli O157:H7. This is because they cause food poisoning without changing the food taste or appearance. Transmission Food safety problems are often caused by these pathogenic bacteria (figure 4), because they can; Spread from hands, equipment or surfaces that have not been thoroughly cleaned Survive in food that is not properly cooked Grow and multiply in food that is left out at room temperature or is not properly chilled Spread from raw food to ready-to-eat food if they are not kept separate Figure 4: Transfer of micro-organisms by hands 8 Activity Think about the food handling tasks you might be required to carry out on your first placement. This may include: Serving food and feeding Preparing formula feeds Assisting mothers with breast feeding/breast expressing Making drinks and working in staff food areas Identify how individuals, families and colleagues could acquire food borne illness from the food and drinks you will handle Important Organisms • • • • • • • Norovirus (Norwalk) like viruses Campylobacter Salmonella E. coli O157:H7 Clostridium botulinum Shigella spp Toxoplasma Emerging organisms Although many pathogens can cause foodborne illnesses, we will briefly cover those of greatest impact. These may also be potential bioterrorism agents for food sources. The pathogens we will discuss include Norwalk viruses, Campylobacter, Salmonella, E. coli O157:H7, Clostridium botulinum, Shigella, and recently emerging organisms such as Norovirus (Table 1). Norovirus (Norwalk) An outbreak of nausea and vomiting in Norwalk, Ohio in 1968 led to the discovery of Norwalk virus. Later, other small round structured viruses were identified as causing a similar disease and named Norwalk-like viruses. They are all members of the Caliciviridae family and have recently been renamed Norovirus. They are an important cause of sporadic gastrointestinal disease outbreaks throughout the world. It is considered the most common foodborne infectious agent and an estimated 23,000 cases occur each year. It is transmitted in the stool and vomit of infected persons and can be shed for up to 2 weeks. Raw shellfish, such as clams and oysters that are harvested from sewage contaminated waters may also induce a norovirus infection. Food-handlers who do not adequately wash their hands may contaminate food or water and spread this disease. Small infectious dose; very contagious and can take as small as 10 viral particles to infect someone o Signs 12-48 hours post-exposure Nausea, vomiting, diarrhoea, abdominal cramps Headache, low-grade fever Duration: 2 days This organism can be shed in the faeces and vomit for up to two weeks, but typically it is recommended that food-handlers not return to work for 3 days after symptoms subside to prevent further spread. Campylobacteriosis Develops 2- 4 weeks after the Campylobacter infection when, diarrhea signs and symptoms disappear. Foodborne related illnesses due to campylobacteriosis is increasing in incidence. It is 9 caused primarily by Campylobacter jejuni, but also C. fetus and C. coli. It is considered the leading bacterial cause of foodborne related diarrhoea affecting 2.4,000 people in the UK each year (514% of all diarrheal illnesses worldwide). Usually these are children under the age of 5 and young adults (15-29 years of age). Very few deaths are caused by this organism. Recently Guillain-Barré Syndrome has been associated with a small number of Campylobacter cases. This syndrome is the leading cause of acute paralysis and develops 2-4 weeks after a Campylobacter infection again that is once diarrhea signs and symptoms disappear. o Sources Raw or undercooked poultry Non-chlorinated water Raw milk Infected animal or human faeces: Poultry, cattle, puppies, kittens, pet birds o Clinical signs Diarrhoea, abdominal cramps, fever, nausea Duration: 2-5 days Salmonellosis This is a gram negative bacteria, which has many serotypes that can cause foodborne related illnesses. The ones we most commonly associated with human foodborne illness are S. typhimurium and S. enteritidis in the UK. They account for about 41% of all human cases reported. S. newport has been on the rise since 1996. Salmonellosis causes an estimated 1.4 million reported cases annually with 580 deaths. Salmonellosis is most severe in elderly, infants and persons with chronic diseases. People with AIDS are particularly vulnerable and often suffer recurring episodes. o Sources Raw poultry and eggs Raw milk Raw beef Unwashed fruit, vegetables, alfalfa sprouts Reptile pets: Snakes, turtles, lizards o Clinical signs Onset: 12-72 hours Diarrhoea, fever, cramps Duration: 4-7 days Escherichia coli O157:H7 Escherichia coli, is a pathogen of foodborne related illnesses. Harmless strains of E. coli are found in nature, including the intestinal tracts of humans and animals. Diarrhoeal disease is caused by several different strains of harmful E. coli. The most dangerous type is entero-haemorrhagic E. coli (EHEC). It gets its name because it can cause bloody diarrhoea and can lead to kidney failure in children or immune-compromised persons. E. coli O157:H7 is the most common EHEC and its entero-haemorrhagic toxin is what actually causes the disease. Surface proteins; toxin o Sources Undercooked or raw hamburger; salami Alfalfa sprouts; lettuce Unpasteurized milk, apple juice or cider Well water Animals: Cattle, other mammals o Clinical signs Watery or bloody diarrhoea, nausea, cramps Onset: 2-5 days Duration: 5-10 days 10 o Sequela Haemolytic Uraemic Syndrome (HUS) Acute kidney failure in children Life threatening Clostridium botulinum Botulism is caused by a neurotoxin from Clostridium botulinum. Fortunately cases are limited, but can be very severe when they do occur. This toxin causes flaccid paralysis and cranial nerve deficits, and can lead to death. Infants are at greatest risk. Approximately 10-30 outbreaks and 110 cases are reported each year. Neurotoxin leads to flaccid paralysis o Sources Home-canned foods fermented meats honey o Clinical signs Double vision, drooping eyelids, difficulty speaking and swallowing Onset: 18-36 hours If botulism is suspected, medical attention should be sought immediately. For more information, please refer to the specific botulism PowerPoint and fact sheet. Shigellosis Shigellosis is also known as bacillary dysentery. Most cases are caused by Shigella sonnei. However, S. dysenteriae, S. flexneri and S. boydii can also cause foodborne related illnesses. Approximately 9,000 cases are reported every year in the UK. It is most commonly transmitted by sick or asymptomatically infected food service workers. o Sources: Human faecal contamination of food, beverages, vegetables, water o Clinical signs: Watery or bloody diarrhea, nausea, vomiting, cramps, fever Onset: 2 days Duration: 5-7 days Toxoplasmosis Toxoplasmosis is caused by an intracellular protozoan, Toxoplasma gondii, which can infect all species of mammals, including humans. As mentioned previously, it is one of the three leading causes of death from a foodborne disease; the others were Salmonella and Listeria. It causes an estimated 1,125 cases of foodborne illness each year and 37 foodborne related deaths. Pregnant women and immuno-compromised individuals, especially HIV positive service users, are at the greatest risk of toxoplasmosis. Toxoplasma gondii- intracellular protozoan o Sources Infected cats (shedding in their faeces and soil undercooked meat mechanical vectors such as cockroaches and flies o Clinical signs Fever, headache, swollen lymph nodes If the protozoan cysts develop in tissue, other more severe clinical signs can be observed. Cyclospora (Protozoan) There have also been increases in the number of cases caused by the protozoan Cyclospora implicated in a 1996 epidemic from imported raspberries. Listeria monocytogenes Listeriosis is one of the 3 most common causes of foodborne related death. 11 o o Sources Ready-to-eat meats such as hot dogs, lunch meat soft cheeses Clinical signs Human abortions and stillbirths Septicaemia in young or low-immune Activity Using information within this work pack and your own research; complete table 1 Table 1: Common food vehicles for certain food-borne related illness pathogens Pathogen Campylobacter jejuni or coli Food sources Symptoms Onset time Clostridium perfringens Escherichia coli 0157:H7 Listeria monocytogenes Salmonella spp. (nontyphoid) Staphylococcus aureas Vibrio sp. 12 Chemical hazards Chemical hazards include; Naturally Occurring Intentionally added Unintentionally added Naturally Occurring Natural or manufactured chemicals and toxins from organisms can also cause foodborne illnesses. Toxins are poisonous substances produced by some micro-organisms, plants and animals. Most toxins that cause food poisoning are tasteless and remain dangerous when cooked. Toxins form in: potatoes when they are exposed to light and turn green fish and other seafood when they feed on algae or other fish that contain toxins. Intentionally and unintentionally added chemical hazards Chemicals in the hospital and the community include those used: to clean kitchen surfaces and equipment; degreasers, detergents, disinfectants, descalers as pesticides. Chemicals can be very harmful if they are: spilt on or near food mistaken for food or drink Be careful when using chemicals around food areas and always follow the COSHH Regulations (The Control of Substances Hazardous to Health, 2002). Remember to; Keep chemicals well away from food Keep them in their original clearly marked container Dilute correctly Wipe them away thoroughly before preparing food on surfaces Read the safety directions before using a chemical to identify how to use it safely and use according to instructions Never put chemicals in food containers or drink bottles Always label chemicals clearly Allergenic hazards These are food ingredients that cause individuals to have an allergic reaction to food when eaten. You must take care to ensure that vulnerable service users are not exposed to these allergens. This is increasingly common in children. Common allergens include; Peanuts Tree nuts Milk Egg Fish Shellfish Physical hazards Soya products Gluten; wheat, rye, barley flour Sesame seeds Celery Mustard Activity Go to: http://tna.europarchive.org/20120419000433/allergytraining.food.gov.uk/english/ This will give you access to the Food Standards Agency's food allergy online training programme. It has been developed by the Agency for Law enforcement officers but it is a useful resource for anyone needing to learn more about food allergy. 13 Physical hazards Any potentially harmful extraneous matter not normally found in food which might physically injure people and/or introduce harmful bacteria into food. Examples include; Glass Wood Stones Metal Plastic Dead insects Hair Jewellery Activity View ‘Bacteria Bite Business’ online video; http://www.flyonthewall.com/FlyBroadcast/FSA/BacteriaBiteBusiness/ This 8-minute video has been produced by the Food Standards Agency (FSA). It demonstrates the importance of good food hygiene, focusing on the 4 Cs (Cleaning, Cooking, Chilling and Cross-contamination). The main causes of food poisoning Includes; Undercooked food Food cooked too far in advance Poor temperature control of food Food contaminated by food handlers Cross contamination of ready to eat food from raw food NB. Food poisoning is often caused by food that looks, smells and tastes normal. Figure 5: Factors contributing to food poisoning outbreaks in UK 14 Visual signs of poor hygiene conditions You have an important role to play in protecting your service users from food borne illness. You should be able to spot the signs of poor hygiene either in the hospital environment or the service user’s home. Some of these indicators might include: Dirty cutlery, glasses and other food equipment Unwashed dishes left for long periods Food in fridges that is mouldy, smelling, uncovered, or out of date Dirty toilets Chemicals left around food Dirty dishcloths Signs of pest infestations such as mouse droppings Food being served at the wrong temperature General unsatisfactory levels of dirt and food debris The Four C’s There are 4 main things to remember for good food hygiene; 1. Cleanliness 2. Cooking 3. Chilling 4. Cross-contamination 1. Cleanliness Cleaning is the process of removing dirt and grease particles and debris, and is often followed by the disinfection process, which then reduces microorganisms to a low safe level. Cleaning and disinfection should be integrated into a work routine and should be formalised in cleaning schedules. Cleaning schedules ensure that cleaning is carried out; At the appropriate frequency In the correct manner Using correct products and materials Using the correct protective equipment Cleanliness will: Ensure a pleasant, safe and attractive environment Promote a favourable image to the service user Reduce materials that would provide food for, or harbour pests Reduce the risk of food poisoning Reduce the risk of physical contamination from foreign matter Remember to: Remove and store food away before cleaning and disinfection Clean as you work, before, between and after food handling tasks Use detergents with hot water to clean surfaces Use sanitisers or other food safe disinfectants to make surfaces and items safe to use Pay particular attention to food contact and hand contact surfaces Make sure that cloths and other cleaning materials are regularly replaced and are not a source of contamination 15 You can prevent the spread of harmful pathogens by observing good personal hygiene and keeping work surfaces, utensils etc clean. It is important to wash your hands regularly, especially: After visiting the toilet After handling raw foods Before touching ready-to-eat food And remember: Don’t handle food when you are ill with stomach problems, such as diarrhoea or vomiting Don’t touch food if you have sores or cuts, unless they are covered with a waterproof dressing 2. Cooking Cooking food to a high temperature will kill harmful pathogens such as listeria, salmonella, E. col 0157 and campylobacter. Above 630C most bacteria die and by 800C even most heat tolerant bacteria are dead. Temperature is a way of ensuring food is safe to eat: Check that the middle/core temperature of food when cooked is at least 700C and ideally 750C or hotter Reheat food, only once, to at least 750C (in Scotland the Law states 820C) When serving food it must be at or above 630C Use a temperature probe as a sure method of testing temperature or check for signs of undercooking such as pinkness of flesh and cooking juices or signs of blood. This applies especially to minced meat and poultry. 3. Chilling Bacterial growth slows down as the temperature drops. Below 5 0C, they only multiply very slowly and when food is frozen they become dormant. Therefore, it is very important to keep certain foods at the right temperature to prevent bacteria growing or toxins forming. Always look at the label on the packaging. If it says that the food needs to be refrigerated, make sure that you keep it in the fridge. If food needs to be chilled is left standing at room temperature, food poisoning bacteria can grow and multiply to dangerous levels (figure 6). Some important temperatures to remember are; Keep chilled ready-to-eat food at or below 80C to comply with the Law Keep food stored in a fridge below 50C. ideally between 1-40C Keep frozen at -180C or colder Cooked leftovers should be cooked quickly and then put in the fridge. Putting food in shallow containers and dividing it into smaller amounts will speed up the cooling process. 4. Cross-contamination Cross-contamination is the transfer of bacteria from foods (usually raw) to other foods. The bacteria can be transferred directly when one food touches (or drips onto) another, or indirectly, for example from hands, equipment, work surfaces or knives and other utensils. Crosscontamination is one of the major causes of food poisoning. 16 To prevent cross-contamination: Always wash your hands thoroughly after touching raw food Keep raw and ready-to-eat foods separate Store raw meat in sealable containers at the bottom of the fridge, so it cannot drip onto other foods Use different chopping boards/work surfaces for raw food and ready-to-eat food Clean knives and other utensils thoroughly after use with raw food Activity We need to control these possible routes of contamination. Think about the areas you work in and how efficiently this control of potential crosscontamination is carried out. It may be by; Using disposables By colour coding equipment Thorough cleaning and disinfection between tasks Figure 6: Important Food Safety temperatures to remember Food Safety in the Community When working on placement in the community environment, particularly in the individuals own home, you may be presented with particular food safety issues. These often result from the fact that the home environment is not regulated under food safety legislation and standards of hygiene and equipment being used may not always be seen as adequate. Particular issues may be: Poor standards of refrigeration due to inefficient and/or unclean fridges Lack of safe, easy to clean work surfaces Food being past its use by date or best before dates 17 Unmarked uncovered food left in the fridge or on work surfaces Lack of cleaning materials Unclean or damaged crockery and cutlery Poor lighting Pest contamination Inefficient or dirty cooking or reheating equipment Lack of food temperature probes and sanitising materials Activity Think about how you might overcome some of the difficulties faced in the community as listed above. You might be doing some of the following; Bring your concerns to the attention of the individual Cleaning before using kitchen without upsetting the individual Checking for signs of pests and reporting any concerns Check use by dates of food in the fridge Throw away unsafe food with prior permission from the individual Cover, label and date anything you leave in the fridge for subsequent use Food at work and you Staff food Food brought in by staff must be stored in a designated staff fridge rather than the service users’ refrigerator. Where a staff fridge is not available, the service users’ fridge may be used provided there is adequate storage space. Staff food must be labelled with the staff members name and date. Any cartons of juice must be dated with the date of opening. A nominated person must ensure that the food beyond the use by date is discarded. Kitchens in your placement area All ward/care home kitchens and refrigerators are bound by legal requirements and therefore are subject to, and must conform to Food Hygiene Regulations. The Local Authority Environmental Health Officer has open access to the Trust and can inspect these areas at any time The Support Service Manager is responsible for ensuring that the following controls are maintained within kitchens: Clean daily and as spills occur Check fridge / freezer door seals regularly for mould splits and general repair state Defrost freezer monthly and use only for short-term storage – fridges/freezers Service users’ personal food must be wrapped or sealed and labelled with the person’s name and date it was placed in the refrigerator. A nominated member of staff must check expiry dates daily. Any food found to be out of date must be discarded (including service user food). Under no circumstances must raw meat, fish or poultry be stored in the ward refrigerator Refrigerators must be used for food storage ONLY. Blood, drugs and specimens are not to be stored in the ward/Kitchen fridge. The refrigerator temperature must be checked and recorded in the morning and evening. The refrigerator must operate below 50C. Where there is a rise in temperature, the door must not be opened for 15 minutes when a second reading must be taken. If the temperature consistently rises above 80C the Support Service Manager should be informed immediately so that alternative storage arrangements or a replacement can be arranged 18 All new appliances must be fitted with a digital temperature display, and be designed to operate between +1 C and +8 C. Microwaves: only dishes designed specifically for microwave use are to be used. Medicine dispensing containers These should be washed in the kitchen sink, NOT in the hand wash basin, and thoroughly dried. Disposable medicine containers must be discarded following use. Service users/Relatives Must not be permitted into hospital ward kitchen under any circumstances. This may not be applicable in a care or nursing home. Service user’s food should never be re-heated. Any low risk food belonging to the service user, such as dried fruit, should be kept in the service user’s locker or room in a labelled plastic sealable container, box or bag Take away food, once in the healthcare setting is the responsibility of the Trust. Any take away food should be piping hot on arrival and eaten straight away. Any left-over should be discarded. Temperature Control Ensure that heated meal trolleys are plugged in immediately on arrival. Ensure that food is served immediately and never reheated. Confirmation that the food has reached the required temperature is made using the appropriate temperature probe by kitchen staff. This must be documented. Food must be removed immediately after the meal with the exception of ‘red food trays’ (if used) which identify service users with nutritional needs. If service users are away at meal times the hot meal must never be retained for longer than 30 minutes. If the service user is likely to be away for longer, then a meal will need to be arranged for them on their return All frozen food should be stored at or below -18°C. Frozen food when arriving must not be above -12°C. All chilled foods should be stored between 0°C and 8°C. Chilled food must not be left outside of chilled storage for more than 4 hours. Any food left out for more than 4 hours must be disposed of appropriately. All hot food must be cooked to a core temperature of above 75°C and should be served before the temperature drops below 63°C. Hot food can be kept for 4 hours if the temperature remains above 75°C, or 2 hours if between 63°C and 75°C (FSA 2007) Ice Creams supplied by the Catering Department are provided in insulated tubs. These must be consumed within one hour of the meal time for which they are provided for. If not consumed within this time, they should be discarded. Preparation of Specialised Formula Feeds, Supplement Drinks and Enteral feeding If required, it is the responsibility of the nursing staff for these to be prepared and distributed in a safe manner that prevents contamination. The following recommendations therefore apply:o Formula Feeds, Supplement Drinks, Single fluid cartons; These need not be refrigerated before use if they are in a sealed container Check that the date on the bottle/carton has not expired before opening Once a bottle/carton has been opened they should be consumed within 4 hours or refrigerated. They should be labelled with the date and time opening before placing in the refrigerator After 24 hours of refrigeration they must be discarded. 19 o Powdered Sachets Before preparing, ensure that hands are washed well and implements used for mixing are clean and dry before use Sachets should be mixed according to the manufacturer’s instructions with cold freshly drawn tap water, freshly boiled water, or cold milk directly from the refrigerator Milk can be heated in the microwave Sachets should be supplied from catering/dietician for single use only, a sachet which has already been opened should not be used The preparation of these drinks should be made in the designated kitchen Once mixed, any drink should be consumed within 4 hours, if not it must be discarded No open packets from home to be brought in Enteral Feeding The National Institute for Health and Clinical Excellence found that 30% of feeds were contaminated with a variety of micro-organisms, with the highest rates of contamination in home settings (NICE 2003). The risk of infection is associated with three main interventions; The preparation and storage of feeds The administration of feeds Care of the insertion site and enteral feeding tube Individuals undertaking enteral feeding must ensure that their hands are decontaminated before; preparing feeds assembling feeding systems any manipulation of the feeding system A clean disposable apron should be worn each time the enteral system is manipulated (NICE 2003). Flushing the feeding tube Sterile water for irrigation is to be used for service users with enteral tube feeding in hospitals and cooled boiled water in the service users’ home. The feeding tube must be flushed with water Before and after feeding Before and after administration of each medicine. Additional flushes may be needed to meet the service users’ daily fluid requirements as specified in their feeding regimen. Feed handling times Hanging times are influenced by the risk of microbial contamination in different circumstances Sterile feed in pre-filled containers can hung for up to 24 hours. Once opened sterile feed must be used within 24 hours or discarded. Giving sets are to be used for one feeding episode and discarded Feed pumps Feeding pumps should be cleaned daily with detergent wipes. Any spillage in between is to be removed with a detergent wipe. Overview of Strategies to prevent food poisoning The main strategies to prevent food poisoning are: Ensure food does not become contaminated Kill or slow down the growth of micro-organisms. 20 o To ensure food does not become contaminated keep hands and nails clean and wash hands and nails thoroughly with warm, running water and soap before: eating, preparing or handling food; between handling raw meat, poultry and seafood, and handling cooked food or food that will be eaten raw after coughing, sneezing, using a handkerchief etc. after going to the toilet after handling rubbish after touching animals after handling chemicals (e.g. cleaning products) o Dry hands thoroughly o Cover cuts and infections on hands o Keep the kitchen clean o When cleaning plates and equipment; scrape and rinse off surface food wash in clean, soapy water rinse in clean water air dry where possible if drying immediately, use only a clean, dry towel o Pest control and animals stop pests such as cockroaches and mice coming into the area where food is kept discourage pests by not leaving food or dirty dishes out on the benches keep animals out of the kitchen o Handle food safely. avoid preparing food when sick or feeling unwell keep raw meats, poultry and seafood separated from cooked food and food to be eaten raw protect food in the refrigerator by placing in covered containers or covering with plastic wrap use clean equipment, plates or containers to prevent contamination of cooked food (or food that will be eaten raw) with traces of raw food use clean equipment, rather than hands, to pick up food wear clean clothes or a clean apron wash fruit and vegetables to be eaten raw under running water. o To kill or slow down the growth of micro-organisms: Cook high-risk foods thoroughly such as; mince, burger patties, sausages, rolled roasts, stuffed meats, rabbit, seafood, poultry o Keep hot food hot and cold food cold: Avoid keeping food in the temperature danger zone of 5°C - 60°C keep cooked food at 60°C or above until served refrigerate or freeze food that is to be prepared well in advance and reheat until steaming hot before serving cook or reheat packaged food strictly in accordance with any directions on the label Place hot food in the refrigerator once it has stopped steaming. Divide large quantities of food into small shallow containers for faster cooling. When reheating for use, heat as quickly as possible until steaming hot. o Keeping cold food cold Avoid keeping food in the temperature danger zone of 5°C - 60°C 21 o take cold groceries home to the refrigerator quickly as possible keep chilled and frozen food cold if it will be a long time before it can be placed in a refrigerator or freezer store cold food at 5°C or less keep cold food in the refrigerator as much as possible thaw frozen food in the refrigerator or microwave store and handle cold food according to any directions on the label check the temperature of the refrigerator regularly Animal products are not the only food that can be contaminated. Various foodborne disease outbreaks have occurred due to fruits and vegetables. The table below indicates the many possible sources for contamination during the processing of produce. Event Production and harvest - Growing, picking, bundling Contamination sources Irrigation water, manure, lack of field sanitation Initial processing - Washing, waxing, sorting, boxing Wash water, handling Distribution - Trucking Ice, dirty trucks Final processing - Slicing, squeezing, shredding, peeling Wash water, handling, cross-contamination Summary: Preventing food poisoning 22 References European Parliament (2004) The General Food Regulations 2004, Regulation (EC) 854/2004 London: TSO, [online]. Available from: http://eurlex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2002:031:0001:0024:EN:PDF [Accessed 30th August 2012]. European Parliament (2004) Hygiene of Foodstuffs, EU Regulation 852/2004, London: TSO, [online]. Available from: http://ec.europa.eu/food/food/biosafety/hygienelegislation/index_en.htm [Accessed 30th August 2012]. European Parliament (2004) Specific Hygiene Rules for Food of Animal Origin, EU Regulation 853/2004, London: TSO, [online]. Available from: www.fsai.ie/.../food.../food_hygiene/specific_hygiene_rules_for_foo... [Accessed 28th August 2012]. European Parliament (2007) Guidance for Food Business Operators on Microbiological Criteria for Foodstuffs, EU Regulation No. 1441/2007, London: TSO, [online]. Available from: http://tna.europarchive.org/20120419000433/http://www.food.gov.uk/foodindustry/regulation/europ eleg/eufoodhygieneleg/microbiolreg [Accessed 30th August 2012]. Food Standards Agency (2006) Food Hygiene: A Guide for Businesses, London: TSO, [online]. Available from: http://webarchive.nationalarchives.gov.uk/20120206100416/http://food.gov.uk/multimedia/pdfs/publ ication/hygieneguidebooklet.pdf [Accessed 30th August 2012]. Food Standards Agency (2006) Food Law Inspections and Your Business, London: TSO, [online]. Available from: www.food.gov.uk/multimedia/pdfs/.../foodlawinspec0310.pdf [Accessed 30th August 2012]. Food Standard Agency (2007) Guidance on Temperature Control Legislation in the United Kingdom EC Regulation 852/2004, London: TSO, [online]. Available from: www.food.gov.uk/multimedia/pdfs/tempcontrolguiduk.pdf [Accessed 30th August 2012]. Food Standard Agency (2007) Bugs Like it Hot, London: TSO, [online]. Available from: http://www.food.gov.uk/multimedia/pdfs/publication/bugslikeithot0607.pdf [Accessed 30th August 2012]. Food Standard Agency (2007) Guidelines for Making up Special Feeds for Infants and Children in Hospital, London: TSO, [online]. Available from: www.food.gov.uk/multimedia/pdfs/.../babypowdertoolkit1007[Accessed 30th August 2012]. Food Standards Agency (2009) Hazard Analysis Critical Control Points (HACCP), London: TSO, [online]. Available from: http://www.food.gov.uk/business-industry/meat/haccpmeatplants/ [Accessed 28th August 2012]. Food Standard Agency (2010) Safer Food Better Business, London: TSO, [online]. Available from: www.food.gov.uk/multimedia/pdfs/fsactguide.pdf [Accessed 30th August 2012]. Great Britain (1990) Food Safety Act 1990, London: TSO, [online]. Available from: www.legislation.gov.uk/ukpga/1990/16/contents [Accessed 30th August 2012]. Great Britain (1999) The Food Standards Act 1999, London: TSO, [online]. Available from: http://www.food.gov.uk/enforcement/regulation/foodstandardsact [Accessed 30th August 2012]. Great Britain (2006) The Food Hygiene Regulations 2006 (as amended), London: TSO, [online]. Available from: www.food.gov.uk/enforcement/regulation/ [Accessed 30th August 2012]. 23 Great Britain (2006) Food Hygiene (England) Regulations 2006, London: TSO, [online]. Available from: http://tna.europarchive.org/20120419000433/legislation.gov.uk/uksi/2006/14/contents/made [Accessed 30th August 2012]. Great Britain (2008) Health and Social Care Act 2008, London: TSO. National Institute for Clinical Excellence (2003) Guidelines for the Management of Enteral Tube Feeding in Adults, London: NICE, [online]. Available from: www.nice.org.uk/nicemedia/live/10978/29981/29981.pdf [Accessed 30th August 2012]. National Patient Safety Agency (2007) Colour Coding Hospital Cleaning Materials and Equipment, London: TSO, online]. Available from: www.nrls.npsa.nhs.uk/Home/Patient safety resources [Accessed 30th August 2012]. 24 Table 1: Common food vehicles for certain food-borne related illness pathogens Pathogen Campylobacter jejuni or coli Clostridium perfringens Escherichia coli 0157:H7 Listeria monocytogenes Salmonella spp. (nontyphoid) Staphylococcus aureas Vibrio sp. Food sources Major: poultry Minor: milk, mushrooms, clams, hamburger, water, cheese, pork, shellfish, eggs, cake icing Major: meat, meat strews, meat pies, beef, turkey, chicken gravies Minor: beans, seafood Major: beef particularly ground beef Minor: poultry, apple cider, raw milk, vegetables, cantaloupe, hot dogs, mayonnaise, salad bar items Major: soft cheese, pate, ground meat Minor: poultry, dairy products, hot dogs, potato salad, chicken, seafood, vegetables Major: poultry, meat, eggs and their products Minor: vegetables, fruit, chocolate, peanuts, shellfish Major: workers handling foods: meat (especially sliced meat), poultry, fish, canned mushrooms Minor: dairy products, prepared salad dressing, ham, salami, bakery items, custards, cheese Major: oysters Minor: other seafood Symptoms Diarrhoea, abdominal cramps, headache Onset time 2-5 days Paralysis, diarrhoea 12-36 hours Watery or bloody diarrhoea, nausea cramps, haemolytic uraemic syndrome 2-5 days Fever, muscle aches, and sometimes with nausea and vomiting. Can lead to Meningitis Variable, can be a few days, or occasional 2 monmths Diarrhoea, fever cramps 12-36 hours Vomiting, abdominal pain, low temperature 1-7 hours Vomiting, diarrhoea, abdominal pain. In very vulnerable people it can lead to septic shock 1-7 days 25