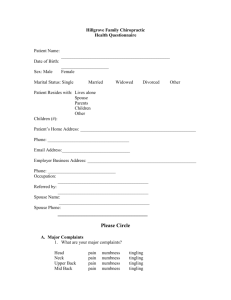
patient history questionnaire
advertisement

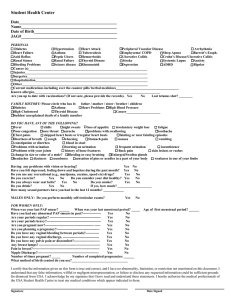
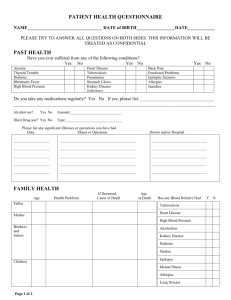
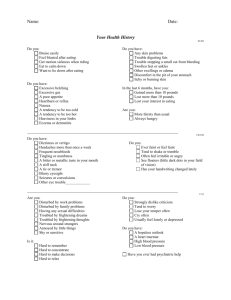
PATIENT HISTORY QUESTIONNAIRE Please fill in as much as possible to facilitate your examination: Name:____________________ Age:_______ D.O.B._______________ Today’s Date:________________ Chief Complaint: (describe briefly your present medical symptoms) ______________________________ _____________________________________________________________________________________ MEDICAL HISTORY: (Please check if you are allergic to any of the following) Penicillin_______ Sulfa______ Aspirin ______ Tetracycline______ Codeine ______ Others: __________________________________ Any foods:____________________________ List any medications you are currently taking, including vitamins, health supplements, herbal medications, allergy injections, contraceptive pills or injections:______________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ _____________________________________ List any previous illnesses or hospital stays, including chicken pox, rheumatic fever, high blood pressure, diabetes, etc: ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ ___________________________________ List any operations you have had and when, including tonsillectomy, appendectomy, C section, etc: _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ PERSONAL HISTORY: Do you smoke? _____ If yes, how long? _____ How many packs per day? _____ Have you ever been a smoker? _____ If so, when did you quit? _____ How much alcohol do you consume per week? _____ Do you now or have you ever used recreational drugs? ______________________________________ Do you wear a helmet when biking, skate boarding, etc.? _______ Do you eat balanced meals? _____ HEALTH MAINTENCE: When was your last: Tetanus injection________ Flu Vaccine_______ Pneumonia Vaccine________ What was your last cholesterol level? _________________ Do you have a living will? ______________ Have you ever had, and if so when: EKG __________________ Chest X-Ray __________________ Sigmoidoscopy _________________ Eye exam ___________________ Dental exam _______________ FOR WOMEN ONLY: Menstrual History: Age at onset or menopause: __________ Regular? ______ Cycle-days (from start to finish) _________________ Usual duration? _________ Date of last period?______________________ Number of pregnancies? _______Do you plan future pregnancies? _________ How many children born alive?_________ Number of abortions or miscarriages? __________ Have you had a mammogram? ____ If yes, when? _________ Do you perform monthly self breast exam? ____ When was your last pap smear? _______ Have you ever had an abnormal pap smear or any type of cervical treatment? ____ If yes, when? _______________ Do you take a calcium supplement? _______ FOR MEN ONLY: Have you ever had prostate trouble? _____ Do you perform self testicle exams on a regular basis? _____ When was your prostate last checked? _____________________________________________________ Please check the following if you have or ever had: _____ Eye disease _____ Fainting spells _____ Loss of consciousness _____Dizziness _____ Depression or anxiety _____ Enlarged glands _____ Trouble with nose, sinuses, mouth, throat _____ Convulsions _____ Paralysis _____ Frequent or severe headaches _____ hallucinations _____Allergies _____Skin disease _____ Chronic or frequent cough _____ Night Sweats _____ Vomiting or cough up of blood ______ Difficulty sleeping ______ Shortness of breath ______ Swelling of hands or feet ______ Indigestion ______ Enlarged thyroid or goiter ______ Frequent nosebleeds ______ Palpitations or fluttering heart ______ Chest pain or angina pectoris ______ Easy bruising ______ Bleeding gums _____ Extreme tiredness or weakness _____ Hemorroids or rectal _____ Liver or gall bladder disease Bleeding _____ Constipation or diarrhea _____ Frequent urination _____ Blood in urine _____ Burning with urination _____ Bladder or kidney stones _____ Sexually transmitted disease _____ Asthma _____ Hay fever _____ Wheezing FAMILY HISTORY IF LIVING: LIVING IN RELATIVE AGE ANY ILLNESSES _____ Trouble swallowing _____ Stomach trouble or ulcer _____ Colitis or other bowel disease _____ Abdominal pain _____ Difficulty controlling urine _____ Loud snoring IF DECEASED: AGE & CAUSE OF DEALTH SAME HOUSEHOLD? Father Mother Brother(s) or Sister(s) Spouse Children If any blood relative has had any of the illnesses listed below, please specify which relative(s): Cancer________________ Tuberculosis _____________________ Suicide______________Arthritis____________ Diabetes_______________ Heart trouble________________ Nervous breakdown/depression________________ Schizophrenia_______________ Stroke_________________ Leukemia_________________ Asthma___________ High blood pressure_________________ Epliepsy_________________ Birth defects/congenital heart__________ Bleeding tendency__________________ Senility/Alzheimer’s_________________ Colitis_____________________ Kidney disease/kidney failure____________________ Alcoholism_________________ Osteoporosis____________