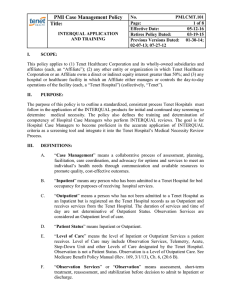
Regulation 42 CFR 421 - Western Missouri Medical Center
advertisement

POSITION TITLE: Utilization Coordinator REPORTS TO: Director of Medical Management DATE: May 21, 2014 JOB SUMMARY: Responsible for review of all inpatient and outpatient admissions to the hospital for appropriateness, facilitating the accurate representation of severity of illness by improving the quality of the physician’s documentation through clinical documentation improvement and manages all access points for admission to the hospital including but not limited to Emergency Department admissions, direct admissions, transfers into and out of the facility and admissions from outpatient areas. Evaluates the medical necessity, appropriateness and efficient use of health care services of all hospitalizations inpatient or outpatient. Skilled with the application of InterQual criteria, works collaboratively with the physicians, healthcare team and the care coordinator to optimally certify the level of care and facilitates the patient’s movement through the continuum of care as appropriate. KNOWLEDGE, SKILLS & EXPERIENCE REQUIRED: RN or Bachelor’s Degree in Nursing required; Bachelors in related field considered 3-5 years recent hospital based patient care 3-5 years Milliman or InterQual experience preferred HMO, managed care, PPO, Utilization Management/medical management experience a plus Current professional licensure in nursing or professional field of certification in the state of Missouri Strong computer skills, excellent communication skills, team building and leadership ability WORKING CONDITIONS: Work environment is located in a comfortable indoor area Conditions such as noise, odors, cramped workspace and/or fumes could sometimes cause discomfort Frequent periods of concentrated or forced attention will be needed to interpret visual, auditory, and sensual inputs Alternate/extended shifts may be required Alertness and careful attention to detail will be required RELATIONSHIPS: Reports directly to the Director of Medical Management PHYSICAL REQUIREMENTS: Frequency Scale: 1 = Rarely/Never; 2 = Occasionally; 3 = Frequently and 4 = Consistently Activity 1 Climbing X 2 3 4 Activity 3 4 - Loud Commands or Public Speaking Pulling X Hearing Pushing X - Normal Conversations X Reaching X - Other Sounds or Auditory Alarms Standing X Vision Sitting X X X Activity 1 2 3 4 Lifting - Normal Conversations X Walking 2 Talking Hand-Eye Coordination Kneeling Stooping 1 X X - Over 50# X - Over 25# X - Under 25# X X Memory X - Acuity, Near - Acuity, Far X - Color Vision X - Short Term X - Long Term X X Analytical Thinking Attention to Detail Concentration X X X Range of Motion Use of Hands - Arms X - General Manual Dexterity - Shoulders X - Keyboard Decision Making X X Reading X X Writing X Skills or Typing AGE CATEGORIES OF INDIVIDUALS SERVED: Demonstrates the knowledge and skills necessary to provide age-appropriate care to the following patient population: ____ Neonatal (1-30 days) ____ Adolescent (13-18 yrs) __X_ No Patient Contact ____ Infants (30 days-1 yr) ____ Adult (19-70 yrs) ____ Children (1-12 yrs) ____ Geriatric (70+ yrs) CORE DEPARTMENTAL COMPETENCIES: Monitors use of healthcare resources, collaborates with physicians to assure patient receives diagnostics/evaluations in the proper setting (i.e. inpatient vs. outpatient). Maintains current knowledge of Condition Code 44, Hospital CoP’s and CMS (Medicare) rules and regulations. Serves as an expert resource to physicians, healthcare staff in the application of InterQual and use of evidence based practices. Serves as patient advocate and enhances a collaborative relationship between the physician and multidisciplinary team with the patient and family to maximize informed decisions. Communicates effectively with third party payors regarding certification, completes initial review prior to or at time of admission. Maintains knowledge of InterQual medical necessity criteria and applies appropriately. Identifies the need to clarify documentation through quality audits in records and initiates communication with physicians utilizing appropriate ‘query’ tools in order to capture documentation in the medical record to accurately support the patient’s severity of illness. Demonstrates knowledge of documentation requirements and guidelines. Assists in the improvement of overall quality and completeness of clinical documentation by ensuring that documentation clarification with physicians has been recorded in the patient’s chart. Reviews clinical data for ED admits, makes level of care recommendations to the ED physician and obtains any additional clinical information to assist in the level of care determination. Manages all direct admits, clarifies level of care orders and performs InterQual screening as appropriate. Acquires additional information if necessary to assist in the level of care determination. Reviews all requests for changes in status for admission from the PACU or any outpatient areas. Applies InterQual criteria to determine appropriateness for the level of care requested and consults with attending if necessary. Insures the operative procedure performed is the operative procedure prior-authorized with the third party payor and communicates any variance. Serves as a resource for facilitating patient transfers, including but not limited to, obtaining or providing clinical information from/to the referring/accepting facility. Performs clinical reviews of all inbound transfers for appropriateness. Demonstrates a working knowledge of HIPAA guidelines and utilizes them in all aspects of communications with customers. Cooperates/communicates with the QIO when a Medicare patient has appealed their discharge. Consults the Physician Advisement process to resolve issues and refers appropriate cases per established protocol. Adheres to and implements the Utilization Management Plan per CMS Conditions of Participation. Reports and documents adverse events and reportable conditions. Consistently follows departmental procedures regarding level of care (service) changes. Discusses cases with particular issues relating to utilization appropriateness with Manager/Director and notifies appropriate peoples when indicated. Displays a high level of flexibility, adaptability and organizational skills in response to the workload and effectively prioritizes work while maintaining productivity. Demonstrates and conveys a favorable image of the Medical Center. Presents a professional appearance in accordance with dress code standards. Demonstrates attendance patterns to reflect commitment to the job requirements and patient care needs. Assists with collection of data for case management metrics per the UM Plan. Supports the Medical Center quality improvement process by identifying and appropriately communicating potential quality issues and participating in focused quality monitoring (i.e. concurrent notification of ADRS, sentinel events, etc.). Contributes to the development of competencies related to job functions and participates in competency evaluations. Participates in department based Performance Improvement activities. Reviews patient’s medical record for over, under and inappropriate utilization. Reviews for justification of patient admission and continued stay. Conducts timely and accurate interventions and follow-through. Informs Patient Financial Services of patients in need of financial counseling. Tracks and documents avoidable days and readmissions with proactive, concurrent action taken when indicated. _____________________________ Director of Medical Management _______________ Date ____________________________ Employee _______________ Date