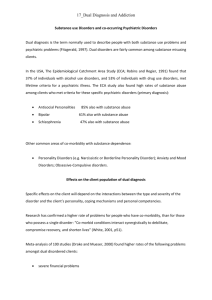
DUAL DIAGNOSIS Dual diagnosis means the diagnosis of
advertisement
DUAL DIAGNOSIS Dual diagnosis means the diagnosis of substance dependence and mental illness. Introduction: Substances can cause psychiatric disorders or make it worse. Psychiatric diseases can cause addiction. This is a highly complicated field and many different situations are possible. The most common disorders are anxiety, depression, hallucinations, schizophrenia and confusion. Prolonged, severe use of nicotine can lead to schizophrenia, sedatives can cause anxiety disorders and marijuana often causes panic attacks and psychosis. Appearance: Dual diagnosis occurs frequently but is rarely picked up early enough and treated correctly. Psychiatric diseases are therefore usually partially and inadequately treated at treatment centers for substance dependence. The situation causes a lot of inconvenience, discomfort, suffering relapses and bigger expense. There are many more complications, doctor visits, poorer results and often leads to suicide. Statistics: Substance dependence occurs in about 10% of a population. Approximately 40% to 60% of patients in rehabilitation centers for dependence have a dual diagnosis. Approximately 33% of patients in psychiatric hospitals are also addicted to drugs (47% schizophrenics, 22% anxiety attack sufferers, 56% bipolar depression, 18% depressed patients, 20% to 40% ADHD). These statistics prove that psychiatric patients addicted to drugs are more than the normal and more dependents suffer from psychiatric illnesses. Reasons for addiction and mental disorders: The reasons for dependence are primarily intoxication, pleasure, recreation, peer pressure, boredom, stress, curiosity, genetic heredity, self-treatment of problems and stress, to relieve side effects of medication, etc.. The reasons for mental illness may be a chemical imbalance in the brain, heredity, traumatic events such as rape, molestation, assault, abuse, etc., overprotection, brain damage, drug addiction and others. In dual diagnosis treatment must deal with the causes of both conditions. Principles of treatment for dual diagnosis: Traditionally substance addiction was treated first and then the psychiatric illness, but often psychiatric illness has not been treated at all. The best is to treat both conditions simultaneously. A thorough evaluation is needed to ensure dual diagnosis is correctly diagnosed. The correct medication must be used for both diseases. A biopsycho-social approach is the best because different specialists give inputs, eg. psychiatrist, psychologist, social worker, physician, nurse, etc.. A Halfway House can help to support and stabilize the patient, where group work is done. The family must also be trained to safeguard the patient and the family must stay involved with treatment for it to be successful. Treatment has to start immediately. Each recovery plan is unique and should suit the needs of the patient and family. Psychiatry and clinical psychology are essential professions in the treatment of dual diagnosis. Signs of dual diagnosis: Frequent relapses on substances Abnormal and deviant behavior Blackouts and memory loss Repression and anxiety -- Suppressed memory and recalling of unpleasant incidents Euphoric recall (recalls only pleasant incidents) Mental illnesses such as depression, schizophrenia, anxiety, psychopathy together with substance abuse Kobus Pienaar CAD ORGANIZER Sources: Hitzeroth, V and Kramer, L: 2010. The end of addiction. Barnard, A. 1994. Wie is dit wat onnodig seerkry?