Supplementary Text S.1 Studies on TSTs (n=34) Levesque et al [23
advertisement
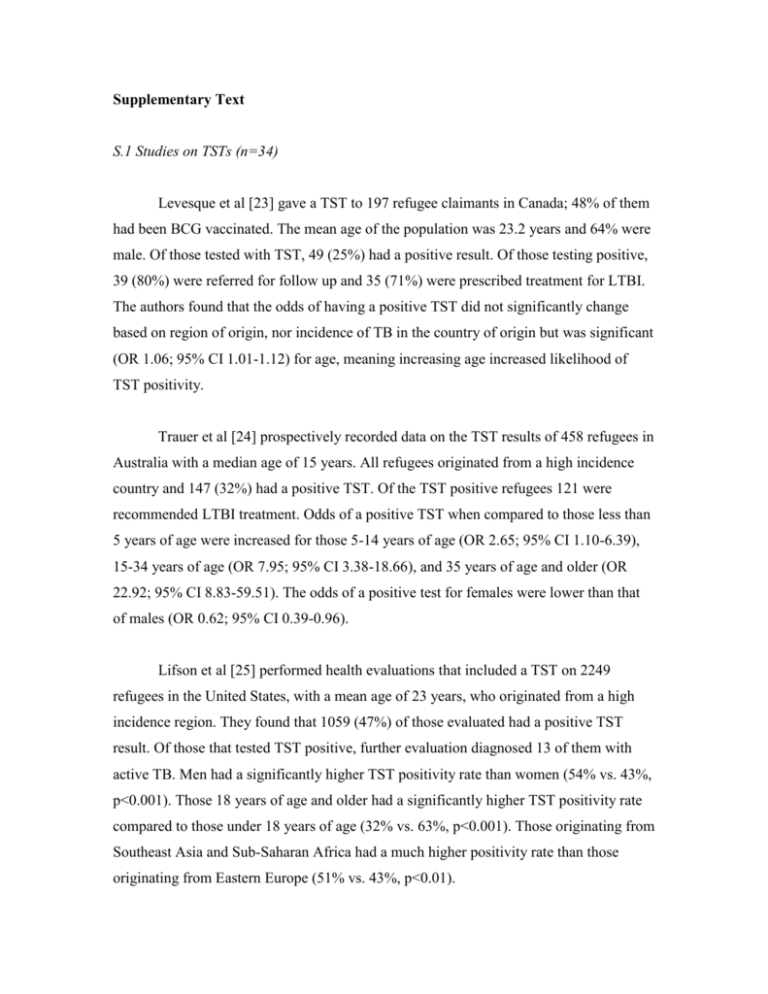
Supplementary Text S.1 Studies on TSTs (n=34) Levesque et al [23] gave a TST to 197 refugee claimants in Canada; 48% of them had been BCG vaccinated. The mean age of the population was 23.2 years and 64% were male. Of those tested with TST, 49 (25%) had a positive result. Of those testing positive, 39 (80%) were referred for follow up and 35 (71%) were prescribed treatment for LTBI. The authors found that the odds of having a positive TST did not significantly change based on region of origin, nor incidence of TB in the country of origin but was significant (OR 1.06; 95% CI 1.01-1.12) for age, meaning increasing age increased likelihood of TST positivity. Trauer et al [24] prospectively recorded data on the TST results of 458 refugees in Australia with a median age of 15 years. All refugees originated from a high incidence country and 147 (32%) had a positive TST. Of the TST positive refugees 121 were recommended LTBI treatment. Odds of a positive TST when compared to those less than 5 years of age were increased for those 5-14 years of age (OR 2.65; 95% CI 1.10-6.39), 15-34 years of age (OR 7.95; 95% CI 3.38-18.66), and 35 years of age and older (OR 22.92; 95% CI 8.83-59.51). The odds of a positive test for females were lower than that of males (OR 0.62; 95% CI 0.39-0.96). Lifson et al [25] performed health evaluations that included a TST on 2249 refugees in the United States, with a mean age of 23 years, who originated from a high incidence region. They found that 1059 (47%) of those evaluated had a positive TST result. Of those that tested TST positive, further evaluation diagnosed 13 of them with active TB. Men had a significantly higher TST positivity rate than women (54% vs. 43%, p<0.001). Those 18 years of age and older had a significantly higher TST positivity rate compared to those under 18 years of age (32% vs. 63%, p<0.001). Those originating from Southeast Asia and Sub-Saharan Africa had a much higher positivity rate than those originating from Eastern Europe (51% vs. 43%, p<0.01). Tafuri et al [26] performed a study at a refugee reception center in Italy where 982 people, with an average age of 25 years, were screened with a TST. In their population, 86% were male, 86% were from a high incidence country, and 596 (61%) had a positive TST result. Each TST positive immigrant was recommended LTBI treatment, however 7 were discovered to have active TB, while 7 TST negative immigrants were also diagnosed with active TB. Men had significantly higher TST positivity rates than women (63% vs. 47%, p<0.0001). Age played a role in the proportion of positive tests with 20% in those under 6 years, 41.4% aged 6-18 years, 62.4% aged 19-35 years, and 61.4% 35 years and older testing positive (p<0.001). TST positivity rates were significantly higher in those from high TB incidence countries compared to those from low incidence countries (p<0.05). Sanfrancisco et al [27] performed a study on immigrants to Spain from countries of high TB incidence. There were 2216 immigrants included, with a mean age of 25.4 years and comprised of 89% males. Of those included, 722 (32%) had positive TST results. Active TB was diagnosed in 2 TST positive immigrants. TST positivity rates were significantly higher in immigrants arriving from Cameroon and Congo than other countries (57% vs. 29%, p<0.00001). Significant differences in TST positivity were not noted based on age or gender. There was no information on BCG vaccination rate and no further analysis was performed. Perez-Stable et al [28] evaluated Latino immigrants arriving to the United States, of which only 6% came from high incidence countries and 42% were BCG vaccinated. Of the 1232 tested with TST, 56% were female and the mean age was 28 years. Positive TST results were seen in 650 (53%) of those tested. Active TB was diagnosed in 2 TST positive immigrants. TST positivity rates were similar for those who were BCG vaccinated (57%) and those who were not vaccinated (61%). Positive TST rates in those immigrants who had been in the United States one year or less were 50% compared to 59% in those who had been in the United States for six or more years. Those from El Salvador or Guatemala had higher rates of TST positivity (63% and 68%, respectively) than those from Mexico or Nicaragua (45% and 48%, respectively). Those under 20 years of age (N=438) had TST positivity rates of 23.2%, those 20 years to 34 years (N=403) had a rate of 72.0%, and those 35 years to 90 years (N=391) had a rate of 65.9%. Menzies et al [29] prospectively evaluated 1198 immigrants in Canada with a TST. The immigrants had a mean age of 21.3 years and 33% had been BCG vaccinated. Positive TST results were seen in 388 (32%) of those tested. Those who reported they had been BCG vaccinated had higher odds for TST positivity than those who did not (OR 1.87; 95% CI 1.22-2.28). In Italy, El-Hamad et al [30] prospectively recruited 993 immigrants from high incidence countries. Of those tested, 58% were male and 82% were less than 35 years of age. There were 392 (39%) screened immigrants with a positive TST result. There were 8 cases of active TB discovered in those testing TST positive. Men had increased odds compared to females for a positive TST (OR 1.62; 95% CI 1.23-2.13). Those from SubSaharan Africa had increased odds (OR 1.66; 95% CI 1.28-2.15) for a positive TST compared to all other regions. Those with a BCG vaccine scar had decreased odds (OR 0.44; 95% CI 0.34-0.58) for a positive TST when compared to those without a BCG scar. Asgary et al [31] performed a prospective study in the United States that evaluated 43 immigrant adults with a TST. In the study, 52% were female and the mean age was 38.7 years. In total, 97% of the adults tested were from a high incidence country and 24 (56%) had a positive TST result. There was no significant relationship between having a positive TST and radiographic evidence of tuberculosis, region of origin, gender or age, speculated by the authors to be due to the small number of participants tested with a positive TST. The study did not perform any further analysis and did not report rate of BCG vaccination. Robertson et al [32] conducted a study on TST results of Vietnamese immigrants to the United States. Of the 121 adults included, 78% were men and all immigrants were over 18 years of age with a mean age of 35 years. None of the immigrants had a BCG vaccine and 35 (29%) had a positive TST result. There were no significant differences seen in age (p=0.07), gender (p=0.19), or CXR result (p>0.2) in those who tested positive and those who tested negative with a TST. No further analysis of the data was performed, as the primary goal of this study was to characterize delayed tuberculin reactivity. Padovese et al [33] performed a study that assessed the TST results in adult Vietnamese immigrants to Malta. The immigrants had a mean age of 26.5 years and 81% were male. Of the 500 adults included, all came from high incidence countries and 15% were BCG vaccinated. A positive TST was seen in 248 (50%) of those tested. Of the positive results, 214 (86%) received a CXR and 32 (15%) were referred for follow-up IGRA due to abnormalities. A positive IGRA was seen in 19 (8%) of those who initially had a positive TST and considered indicative of LTBI. All 19 were offered preventative treatment. Carvalho et al [34] performed a prospective study in Italy that tested 213 immigrant adults with a TST, all of which originated from a country with a high TB incidence. In the study population, 70% were male and the mean age was 27 years. Of those tested, 124 (58%) had a positive TST. Of the positives, 55 (44%) were diagnosed and began treatment for LTBI. Female immigrants had lower odds for LTBI diagnosis compared to males (OR 0.4; 95% CI 0.2-0.8). The highest rates of LTBI were seen in those from North Africa (64%) followed by Latin America (62%) and Pakistan (61%). Alperstein et al [35] performed a study in Australian public schools that administered TSTs to overseas-born children and 76% were vaccinated with BCG. Of the 353 tested, the majority was between 5-7 years of age. The TSTs resulted in 99 (28%) children having a positive result. Clinical assessment was advised for 140 of the original 353 (39.7%) and 89 of these 140 (63.5%) were offered preventative therapy, with nine declining. Active TB was found in 2 of the 140 referred for assessment. It was found that age at arrival was not significantly associated with having a positive TST. Of the children tested from a low incidence country (N=27), 19% were TST positive, while 29% of the children tested from a high incidence country (N=326) were TST positive. Minodier et al [36] completed a study that recorded TST results in immigrant school children in Canada. Of the 3401 children that received a TST, 52% were males and the mean age was 12.2 years. Of those tested, 777 (23%) were positive and of those positives, 692 (89%) were BCG vaccinated. Of the positives, 683 (88%) visited a clinic and 573 (74%) began treatment with 334 (43%) adequately completing LTBI treatment. Compared to those immigrating from a country with an established market economy, all those immigrating from other regions showed higher odds for a positive TST, including those from Southeast Asia (OR 2.41; 95% CI 1.15-5.06), Eastern Mediterranean (OR 2.65; 95% CI 1.23-5.69), low HIV Africa (OR 3.0; 95% CI 1.33-6.78), high HIV Africa (OR 3.9; 95% CI 1.57-9.73), Central Europe (OR 3.0; 95% CI 1.18-7.64), the Western Pacific (OR 3.44; 95% CI 1.67-7.08), East Europe (OR 4.23; 95% CI 2.04-8.77), and Latin America (OR 4.03; 95% CI 1.93-8.39). It was found that age at the time of TST or mean age at immigration were not significantly associated with a positive test. Of those from low incidence countries (N=1091), 3% were TST positive and 33% of those from high incidence countries (N=2229) were positive. Geltman et al [37] performed a study on TST results in refugee children living in Massachusetts. In the study population, 94% of the refugee children were from countries of high TB incidence. They found that the 1737 included children were aged 0-17 years and 48% were female. Positive TSTs were seen in 440 (25%) of children tested. TST positivity rates were higher in those 6-17 (30%) than in those 5 years of age and less (14%). Rates of TST positivity in Africa, the Americas, East Asia, the former Soviet Union, and former Yugoslavia were all similar (21-29%), however rates in the Near East were lower (9%). No significance or association tests were performed in this study and BCG vaccination was not evaluated. Sheikh et al [38] completed a study evaluating TST results in refugee children coming from regions of high TB incidence visiting an Australian clinic. It was found that of the 216 tested, 53% were female and all children were aged 0-17 years. Of those tested, 71 (33%) had a positive TST, while many of the positive results were vaccinated with BCG. Rates of TST positivity were highest in the Middle East (93%), Eastern Africa (44%), and Western Africa (28%), while rates were much lower in Asia (14%) and Central Africa (7%). No significance or association tests were performed in the study to quantify strength of effect. Gray et al [39] evaluated at the TST results of refugee children from varying countries in Australia. Included were 328 children aged 0.5-17.5 years with 46% of them female. They found that 92 (28%) of those tested had a positive TST result. Of those positive for TST, 81 (88%) were diagnosed with LTBI and recommended treatment. The study compared vitamin D deficiency with presence of LTBI infection and found that rates of LTBI trended higher the more vitamin D deficient the participant was. No other analysis was performed and significance and association were not evaluated. Losi et al [40] administered a TST to immigrant children in Italy. About 67% of those tested came from regions of high TB incidence. There were 621 children aged 0-19 years given a TST and 104 (17%) had positive results. TST positivity rates differed across age groups with those 0-11 years of age having positivity rates less than 5% and those 12-19 years of age with rates of approximately 18%. Those with TST 5 mm or greater were given an IGRA. It was found that four (8%) of the 50 IGRA and TST positive children had active TB. All children diagnosed with active TB were greater than ten years of age and had been BCG vaccinated. No further analysis was performed. Hladun et al [41] completed a study on immigrants to Barcelona between February 2001 and 2005. Participants were given a TST, of which they were all ≥15 years of age and 58% were male. Of the 309 total participants, 87 (28%) were positive and diagnosed with LTBI if they had a normal chest x-ray. No differences were detected in rate of positive test results based on WHO region of origin (p=0.057). Baussano et al [42] performed a retrospective study in immigrants to Western Europe between January 1991 and December 2010. Of the 26,554 participants, 91% were ≥20 years of age and 59% were male. Nearly 80% of immigrants came from countries that had a TB incidence ≥100 cases per 100,000 person years. There were 9180 (34.6%) immigrants who tested positive for LTBI with a TST. Males were equally likely to test positive compared to females, as TB incidence increased from <25 cases per 100,000 person years, the odds of a positive TST increased with odds of 2.0 (95% CI 1.6-2.6), 1.6 (95% CI 1.2-2.1), 2.6 (95% CI 2.1-3.3), and 2.2 (95% CI 1.7-2.9) for those in TB incidences of 25-49, 50-99, 100-299, and ≥300, respectively. Age increased odds of LTBI; compared to those <20 years of age, odds of 1.9 (95% CI 1.7-2.2), 3.1 (95% CI 2.8-3.5), and 3.1 (95% CI 2.7-3.5), were seen in those aged 20-29, 30-39, and ≥40 years of age, respectively. Kowatsch-Beyer et al [43] completed a study that evaluated refugees admitted to the United States with a TST in 2008. The median age of the cohort was 30, with 52% male. Of the 224 refugees who took a TST, 102 (45.5%) were positive. The prevalence of positive results was highest in immigrants from East Asia and lowest in immigrants from South Asia. In total 113 refugees were referred for follow-up, of which 60 attended. Odds of follow-up was found to be higher in those from East Asia compared to those from Africa (OR 12.48; 95% CI 2.32-67.06). Martin et al [44] conducted a retrospective examination of TST results of 2033 refugees in Australia with 50% between 15 and 34 years of age. Of those tested 1040 (51%) had a positive TST result. The analysis showed the highest rates of TST positivity was in refugees 15 to 19 years of age, with 55% being positive compared to only 0.7% for native Australians in that age range. Region of birth did not affect TST positivity significantly. Those arriving from a low incidence country (N=616) had a 47% positivity rate while 52% were positive if they were from high incidence countries (N=1517). Varkey et al [45] looked at 9842 refugee arrivals to the United States, 97% of which were 65 years of age or less. A TST was performed in each refugee and 4990 (51%) were positive. Only 2446 (49%) of TST positive refugees were diagnosed and treated for LTBI. There were also 36 TST positive refugees diagnosed with active TB, while 5 TST negative were diagnosed with it as well. Compared to women, men had increased odds of 1.6 (95% CI 1.5-1.8) for a positive TST. Each increase in 10 years of age had increased odds for a positive TST (OR 1.38; 95% CI 1.33-1.41) and originating from Africa had increased odds (OR 1.6; 95% CI 1.5-1.8) when compared to other continents. MacIntyre et al [46] retrospectively reviewed 938 refugees to Australia with a mean age of 33 years, all of whom came from a high incidence country. The refugees were given a TST and 561 (60%) had a positive result. Only 124 (22%) of TST positive refugees were diagnosed and given LTBI therapy. Those with a positive skin test were older than those who did not have a positive skin test (median age 24 years vs. median age 20 years, p<0.0001). Chai et al [47] conducted a retrospective cohort review of 611 refugees and asylum seekers, with median ages of 22 years and 31 years respectively, to the United States who received a TST. Of those tested, 56% were male and over 95% were from a high incidence country. In total, 239 (39%) had a TST that was positive. LTBI therapy was recommended in 184 TST positive participants. Refugees in the study were at higher odds of being recommended LTBI treatment in comparison to refugees (OR 2.7; 95% CI 1.2-6.0). There was no significant difference between asylees and refugees in terms of TST positivity rates. In total, two cases of active tuberculosis were found in the retrospective cohort (0.3%), although TST result was unclear. Hobbs et al [48] evaluated TST results of refugees in New Zealand. Of the 869 refugees included, 82% were from a high incidence country, 68% were male, and 97% were under 50 years of age. Positive TSTs were seen in 316 people (36%), 160 (51%) of which were then diagnosed with LTBI and treated with chemoprophylaxis. There were 718 (80%) refugees further screened with CXR of which, 12 were diagnosed with active TB and given full multi-drug treatment. Of these 12, 4 had a positive TST result. Bran et al [49] completed a retrospective study of TST results on 728 immigrants to Spain who were predominantly male (78%) and aged 25-35 years (64%). Of those tested, 351 (48%) had a positive TST result. There were 61 TST positive immigrants who were recommended treatment. Men had higher odds of having a positive TST compared to females (OR 1.59; 95% CI 1.10-2.32). Age increased the odds of a positive TST. When compared to those 0-14 years, immigrants between 15-24 years of age (OR 7.12; 95% CI 2.28-24.72) and immigrants 25-35 years (OR 7.28; 95% CI 2.39-24.82) had higher odds of a positive TST. When compared to South America, only those from Africa had higher odds of a positive TST (OR 1.93; 95% CI: 1.32-2.78). Li et al [50] performed a retrospective study on TST results of foreign-born immigrants to the United States. 20 808 people were included with 54% being males and the vast majority between 10-64 years of age (96%). BCG vaccination was found in 91% of participants and 8219 (39%) of those tested had a positive TST result. Using a prevalence ratio (PR) TST positivity in men was more prevalent than in women (PR 1.2; 95% CI 1.15-1.24). TST positivity was more prevalent in those BCG vaccinated at birth (PR 2.3; 95% CI 2.0-2.5) and after one year of birth (PR 2.1; 95% CI 1.8-2.4), compared to those unvaccinated. Age increased the prevalence of a positive TST. Compared to those under 5 years of age, TST positivity was more prevalent in those aged 5-19 years (PR 2.3; 95% CI 1.2-4.2), 20-34 years (PR 2.8; 95% CI 1.5-5.2), 35-64 years (PR 3.2; 95% CI 1.8-5.9), and 65 years and older (PR 2.8; 95% CI 1.5-5.2) Compared to a low incidence country, a high incidence country had a higher prevalence of a positive TST (PR 1.7; 95% CI 1.6-1.8). Of those from low incidence countries (N=3356), 28% had a positive TST while 42% of those from high incidence countries (N=17,250) had a positive TST. Desale et al [51] performed a study where a TST was given to immigrant adults in the United States, the majority of which originated from countries of low TB incidence. The mean age was 34 years and 64% were male. In total 391 adults were given a TST and 164 (42%) had a positive test result. Women (N=148) had a lower TST positivity rate at 37.2% compared to males (N=242) with 44.6%. TST positivity rates in this population varied greatly by specific country of origin (p<0.001). There were 101 (62%) TST positive individuals that were eventually diagnosed with LTBI and 53 (32%) that completed LTBI treatment. Of those from low incidence countries (N=117), 49% were TST positive while of those from high incidence countries 50% were TST positive (N=191). Truong et al [52] performed a retrospective study on the TST results of Tibetan immigrant adults to the United States. The median age was 30 years and 53% were male. There were 160 immigrants in the study and 154 (96%) had a positive TST result. The authors compared TST positivity rates among other studies and found that those from Tibet had significantly higher rates of positive TSTs than Vietnamese (44%), Hmong (10%), and Russian (51%) refugees (p<0.001). Further evaluation by CXR was performed in all Tibetan immigrants and it was found that 97 had abnormalities. LTBI preventative therapy was recommended in 110 Tibetan immigrants. The 4 immigrants who did not complete therapy developed active TB. Mulder et al [53] evaluated TST results of adult immigrants to the Netherlands. There were 643 adults included with 43% being male and 76% aged 18-34 years. BCG vaccination was noted in 85% of participants. A positive TST result was found in 418 (42%). Of the BCG vaccinated (N=549), 249 (45%) had a positive TST. TST positivity rates in those 18-24 years of age (28%) were lower than in those 25-34 years of age (48%) and in those 35 years of age and older (48%), although significance tests were not reported. TST positivity rates were highest in those from Sub-Saharan Africa (53%), although significance tests against Europe and the Americas (41%), North Africa and Middle East (43%), and other Asian countries (39%) were not reported. Hayes et al [54] performed a retrospective review of TST results for refugees attending a United States clinic. The 128 children included had a mean age of 10 years and 42% were female. Approximately 95% of the refugees included were from countries of high TB incidence. All children were screened with a TST within 7 months of arrival and 45 (35%) had a result that was positive. Further radiographic testing was performed in all 45 who had a positive TST. It was discovered that one patient had active TB, two had inconclusive results, and the remaining 43 did not have evidence of any abnormalities. No analysis was done and BCG vaccination was not reported. Fortin et al [55] performed a retrospective study in Canada that looked at TST results in immigrant children. Approximately 75% of the immigrant children included in the study were from high incidence countries and 73% were BCG vaccinated. Of the 515 with TST results, 73% were female and ages ranged from 0.3-19 years. There were 85 (16%) children who tested TST positive. It was found that for every year of age, there were increased odds of a positive TST (OR 1.2; 95% CI 1.1-1.3). Having a BCG vaccination lead to an increased odds for a positive TST (OR 2.2; 95% CI 1.2-4.1), compared to no vaccination. Gender and region of origin were not significantly associated with a difference in rates of positive TSTs. Brassard et al [56] performed a retrospective study that looked at TST results in immigrant children (aged 4-18 years) in Canada. Approximately 90% of those tested were from countries of high TB incidence. Positive TST results were seen in 542 (21%) of the 2524 tested. Of the positives, 375 (69%) started LTBI treatment. There were 484 children that were referred and attended follow-up. Of these children, 53% were male, they had a mean age of 12.4 years, and 84% were BCG vaccinated. No further analysis was performed in this study that looked at associations for a positive TST. S.2 Studies on IGRAs (n=9) Bodenmann et al [57] evaluated IGRA responses of 125 immigrants to Switzerland, of which about 30% were from a high incidence country. The mean age of the study population was 34.8 years and 47% were female. It was found that 24 (19%) of those tested were positive. Of those who were positive, 2 were smear positive for TB. There were 16 (67%) of the 24 positives followed up for LTBI and 14 (58%) were diagnosed with LTBI. Preventative treatment was accepted by 10 (71%) people and completed adequately by 5 (50% of those who accepted). No evaluation of risk association was performed and BCG vaccination was not noted. Pareek et al [58] performed a study on 1229 immigrants at three different immigrant-screening centers in the UK. All immigrants included were under 35 years of age and 51% were female. BCG vaccination was confirmed for 43% of the cohort. Of those tested, 245 (20%) had a positive IGRA result. It was found that age and BCG vaccination were not associated with having a positive IGRA. Males had increased odds for a positive IGRA compared to females (OR 1.4; 95% CI 1.1-1.9). Compared to TST positivity rates in Europe and the Americas, Asia (OR 5.2; 95% CI 1.2-22.8), the Indian Subcontinent (OR 5.8; 95% CI 1.4-24.1), and Sub-Saharan Africa (OR 9.1; 95% CI 2.238.5) all had increased odds of a positive IGRA. Compared to low incidence countries, countries with a TB incidence of 251-350 cases per 100 000 people (OR 13; 95% CI 1.798.2) and greater than 350 cases per 100 000 people (OR 11.7; 95% CI 1.5-91.5) had an increased odds of having a positive IGRA. Mulder et al [59] performed a retrospective analysis of IGRA test results of 1468 adult immigrants to the Netherlands. In the population included, 79% were between 18 and 34 years of age and 54% were female. Positive IGRA results were seen in 296 (20%) of immigrants tested. Age (p=0.982) and gender (p=0.086) were not significantly associated with higher rates of IGRA positivity. Those coming from a high incidence country had significantly higher rates of IGRA positivity than those from low incidence countries (p<0.01). No further analysis was performed on this retrospective cohort of patients. Garfein et al [60] performed a study in the United States looking at IGRA test results of adult immigrants, none of who were from a high incidence country. The 133 tested had a median age of 35 years and 63% were female. Positive IGRA results were seen in 53 (40%) and 76% were BCG vaccinated. There was no significant increase in odds of a positive IGRA based on age (p=0.16), gender (p=0.71), or BCG vaccination (0.10). There were 10 participants who had symptoms suggestive of active TB, however none were diagnosed with TB. No further analysis was performed in the study. Harstad et al [61] performed a study in refugees over 18 administering an IGRA to 823 individuals. In the population, 74% was male and 95% fell between the ages 18-49 years. Of those tested, 246 (30%) tested positive with an IGRA. Of the IGRA positive patients, only 8 (3.3%) began LTBI treatment, yielding a positive predictive value (PPV) of 3.3%. Those 50 years of age or older had IGRA positivity rates of 57%, higher than those 18-49 with a rate of 29%. Higher IGRA positivity rates were found in those from Africa (44%) compared to those from Europe (18%) and Asia (20%). This study found no significant difference between median interferon-gamma levels in IGRA positives with TB compared to those without disease (p>0.05). In the IGRA positive group, 8 refugees were diagnosed with active TB, while only 1 refugee in the IGRA negative group had this diagnosis. Bennett et al [62] completed a study in San Diego County examining refugee arrivals between January 2006 and December 2007, retrospectively. The population had a mean age of 19.8 and 49% were male. Every entrant was from a typically high-incidence region (Africa and Asia). There were 4280 refugees given an IGRA and 916 (21.4%) were positive. Chest x-rays were given to each of the positive patients and 823 were diagnosed with LTBI while 14 had a result consistent with active TB. Refugees from Sub-Saharan Africa had the highest prevalence of LTBI (OR 5.3; 95% CI 3.9-7.2), males were more likely to have LTBI (OR 1.7; 95% CI 1.4-2.0), increasing age contributed to LTBI with those 35-49 years of age and those ≥50 years of age at increased odds of LTBI compared to those 13-17 years of age with odds of 2.9 (95% CI 2.0-4.0) and 6.5 (95% CI 4.6-9.2), respectively. Of the 823 diagnosed with LTBI, 489 were recommended for treatment, of which 373 actually initiated treatment; only 219 completed treatment adequately. Initiation of treatment was much lower in those from Africa (OR 0.5; 95% CI 0.3-0.8). Banfield et al [63] performed a retrospective review of IGRA results of 1130 refugees to Australia, 1004 (89%) of which had determinate results and all of which originated from countries with a high incidence of TB. The refugees had a mean age of 19.8 years and were 49% male. They discovered that 264 (26%) of those tested had a positive IGRA result. Of these positives, 8 were diagnosed with active TB. It was found that gender and country of origin were not significantly associated with increased IGRA positivity rates. A higher age at the visit to the clinic was found to lead to increased odds for a positive IGRA (OR 1.1; 95% CI 1.08-1.12). Having the test in autumn (OR 0.46; 95% CI 0.28-0.74), winter (OR 0.52; 95% CI 0.34-0.79), and spring (OR 0.64; 95% CI 0.42-0.98) all had lower odds of a positive IGRA than testing in summer. Indeterminate IGRA results were associated with age at visit (OR 0.94; 95% CI 0.93-0.96). Simpson et al [64] completed a retrospective review of IGRA results in 533 immigrants and refugees to the United States. The populations mean age was 29 years and 49% were male. It was found that 128 (23%) of those tested had a positive IGRA result. Age (Cramer’s V=0.297), race (Cramer’s V=0.167), ethnicity (Cramer’s ϕ=0.074), gender (Cramer’s ϕ=-0.053), TB symptoms (Cramer’s ϕ=0.032), and prevalence of TB in country of origin (Cramer’s V=0.139) were associated with having a positive IGRA. Indeterminate results in Burmese participants (7/228) when compared to other countries (1/313) were much higher in proportion (p<0.05). Paxton et al [65] performed a retrospective review of IGRA screening in refugees from high incidence countries in Australia. There were 208 children included who were between 0 and 17 years of age. It was found that 33 (16%) of the children tested had a positive IGRA result. The same study reviewed 602 adult refugees 18 years of age or older. It was found that 136 (23%) of the adults tested had a positive IGRA result. No further analysis on either study group was performed in this study and BCG vaccination was not evaluated. S.3 Studies on both TSTs and IGRAs (n=8) Orlando et al [66] performed a study in Italy on immigrants, of which 50% were from high incidence countries. In total, 899 immigrants received TST testing while 1115 received IGRA testing. Only 6% of the population was BCG vaccinated. The population was 44% male and the median age was 35.3 years. TST positives were seen in 407 (45%) of those tested, while 337 (30%) of those tested with an IGRA were positive (p<0.0001). No significant differences in odds for TST or IGRA positivity was noted based on gender, BCG vaccination, or continent of origin. The odds of a positive IGRA were higher in those from countries with a TB prevalence greater than 200 cases per 100 000 persons when compared to those from low prevalence countries (OR: 2.72; 95% CI 1.75.02). Saracino et al [67] performed a study evaluating 279 immigrants in Italy with a TST and an IGRA. The average age was 27.1 years and 96% of immigrants were male. Nearly 97% of the immigrants were from high incidence countries, with 72 (26%) testing positive with a TST and 107 (38%) testing positive with an IGRA. Overall test agreement was 70.9% (κ 0.35). Of the discordant results, 58 were IGRA positive and TST negative, while 23 were IGRA negative and TST positive. Positivity rates for IGRA or TST were not significantly associated with age, region of origin, or TB burden in country of origin. Further, these variables were not significantly associated with discordance. Baker et al [68] performed a study looking at the TST and IGRA results of 195 refugees in the United States, nearly all of which were from a high incidence country. The median age in the population was 19 years and 34% were males. A positive TST was seen in 108 (55%) while 105 (54%) had a positive IGRA. Concordant results were observed in 78% of given tests (κ 0.56; 95% CI 0.44-0.67). Concordance was significantly associated with both age (p=0.001) and gender (p=0.011), however not associated with country of origin (p=0.8785). Repeat testing of the IGRA was performed with concordance of 89% (κ 0.76; 95% CI 0.66-0.86). Weinfurter et al [69] evaluated 594 high-risk refugees to the United States with both TST and IGRA results. The population was 52% male and 51% were less than 30 years of age. BCG vaccination was noted in 92% of those screened. Of those tested, 271 (46%) were positive for TST and 171 (29%) were positive for IGRA (p<0.01). It was found that positive agreement between the two tests was 24% while negative agreement between the two tests was 71% (κ 0.46; 95% CI 0.39-0.53). In comparing these high-risk refugees to US-born people, the odds of a positive TST were significantly higher (OR 15.45; 95% CI 9.30-25.65) and the odds of a positive IGRA were higher (OR 7.72; 95% CI 4.64-12.83). Pottumarthy et al [70] performed a prospective study in 237 refugees to New Zealand from countries with a high TB incidence, screening them with both TST and IGRA. The median age of those tested was 28 years. They found that 86 (36%) and 71 (30%) of those screened were positive with a TST and IGRA, respectively. It was found that negative agreement between the two tests was 89%, while positive agreement was 64% (κ 0.55). Of the 47 immigrants that had discrepant TST and IGRA results, none had radiological evidence of TB. No further analysis was performed in this group and BCG vaccination was not evaluated. Carvalho et al [71] evaluated 100 adult immigrants with a TST and IGRA in Italy. The median age was 28 years and 75% were male. In the cohort, 92% were from high incidence countries and 64% were BCG vaccinated. They found that 44 (44%) had a positive TST and 15 (15%) had a positive IGRA. It was found that negative agreement between the two tests was 100%, while positive agreement was only 34% resulting in an overall agreement of 71% (κ 0.37). There were lower odds of discordance in the presence of BCG vaccination (OR 0.28; 95% CI 0.10-0.77), however no associations were found for discordant results based on gender, age, race, and previous TB contact. Winje et al [72] performed a prospective study on 912 asylum seekers to Norway. Of those included, 75% were male and the median age was 29 years. In the population, 264 (29%) were IGRA positive and 311 (34%) were TST positive. Positive agreement between the two tests was found to be 21%, while negative agreement was found to be 58%, resulting in an overall agreement of 79% (κ 0.51; 95% CI 0.45-0.57). It was found that those 50 years of age or older had increased odds of a positive IGRA result compared to those 18-29 years of age (OR 3.5; 95% CI 1.8-7.1). Those from Africa had increased odds of a positive IGRA compared to those from Asia (OR 3.1; 95% CI 2.2-4.2). Painter et al [73] completed a prospective study between December 2008 and January 2010 in Vietnamese visa applicants at the Cho Ray Medical Visa Unit in the United States. In those included, the mean age was 37.3 years and 48% were male. Of the 20,100 visa applicants 17,802 had a normal chest x-ray and of those 479 were recruited to the LTBI study. Positive TST results were seen in 236 (49%) and a positive IGRA was seen in 161 (34%). Agreement between tests was deemed to be fair (κ 0.32). Overall, those ≥30 had higher rates of positive TST and IGRA, while the same trend was seen in males compared to females.