SUMMARY IGRAs are recommended for: 4
advertisement

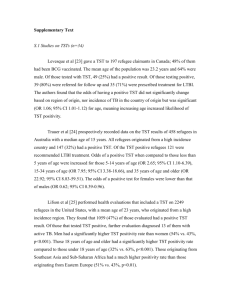
DR.RAGHAVENDRA.H.GOBBUR PROFESSOR OF PEDIATRICS B.L.D.E.UNIVERSITY’S Shri.B.M.Patil MEDICAL COLLEGE ,BIJAPUR rhgobbur@gmail.com Newer modalities in TB diagnosis Guest lecture given at state PEDICON 2011 DR.RAGHAVENDRA.H.GOBBUR PROFESSOR OF PEDIATRICS B.L.D.E.UNIVERSITY’S Shri.B.M.Patil MEDICAL COLLEGE ,BIJAPUR. rhgobbur@gmail.com Newer modalities in TB diagnosis • • • • • • IGRA assay Interferon (IFN)-γ Assay Microscopy LED Culture :Liquid Medias: BACTEC, BAC T/ALERT 3D, MGIT DNA NAAT: Real-time PCR, LIPA Enzyme Assay: ADA QUANTIFERON-TB GOLD in place of Mantoux test . INTERFERON G ASSAY (IGRA) IFN-γ QUANTIFERON-TB GOLD . IN VITRO TEST ESAT-6 ,CFP-10 synthetic peptides are used (Absent in BCG and most NTM) stimulate T-cells from infected people releasing IFN-γ, from These T-cells *early secretory antigenic target-6 **culture filtrate protein-10 LTBI - TST V/S V/S DISEASE ? IGRA QUANTIFERON-TB GOLD . • Objective , and controlled test Reduces subjectivity in TB diagnosis • Simple diagnostic cut-off (> .35 IU/ml IFN-γ = + ) Straight forward positive/negative interpretation • Eliminates 2 step testing • No ‘booster’ effects in-vitro • Faster turn-around, results in 24 - 48 hours • Results are electronic (computer generated reports) INDIAN STUDY USING QUANTIFERONTB GOLD • Dogra S, Narang P, Mendiratta DK, Chaturvedi P, Reingold AL, Colford JM Jr, Riley LW, Pai M. Comparison of a • whole blood interferon-gamma assay with tuberculin skin testing • . ( J Infect 2007; 54:267–76.) • Compared QFT to the TST in 105 children ( suspected of TB, or had contact with an index case). • • • • • 11 children (10.5%) were QFT positive, whereas the TST was positive in 15 (15%) at ≥5mm, 11 (10.5%) at ≥10mm, or 4 (4%) at ≥15mm . Concordance of TST with QFT was high (95%) at the 10mm TST cut off • All subjects with≥15mm TST , were QFT positive. • There were • no indeterminate QFT results, despite 40% children being <4 years old , and 57% of them being malnourished. SUMMARY of IGRA TESTING IGRAs are recommended for 1. Contacts of active TB Close contacts (HIGH RISK) TST OR IGRA if either is positive, treat for “L TB I” (latent infection) Casual contacts (LOW RISK) can have IGRA confirmation if TST is positive to verify infection v/s BCG or MOTT 2. Immune compromised “suspected child" TST first, if negative do IGRA and if IGRA positive treat as LTBI M.TB. STAINING BY ZEIL-NEILSON STAIN • >1,000 Organism per ml sputum required for ordinary microscope. • Fluorescent, LED microscope detects even 100 M.TB. organism per ml AFB + SPUTAM SMEAR fluorescent LED microscope based on the proven Primo Star platform.( FIND/Zeiss microscope offers superior optics, FIND and Carl Zeiss reflected light illumination, easy switch from bright field to fluorescent light) MYCOBACTERIAL CULTURE Culture remains the gold standard for lab confirmation of TB Advantages: Increases number of case detection Detects cases among smear negative patients Establishes viability of organisms Distinguishing between Mycobacterial species Helps in performing DST (drug sensitivity test) Helps in diagnosing cases of treatment failure Limitations: Expensive Require enriched media Require considerable expertise Time consuming Processing of sputum with CPC Method If delay of more than 48 hours between collection and processing is anticipated, the sputum should be collected with 1%CPC and 2%NaCl2 CPC acts as homogenizing and decontaminating agent It helps in retaining viability of Tubercle bacilli up to 7 days These specimens should not be treated with NaOH ( Petroff’s) Culture: Extra-Pulmonary Samples Aseptically collected samples Body fluids: Spinal ,Pleural, Pericardial, Synovial, ascitic, Blood, Pus & Bone marrow Tissues: Lymph node, Needle biopsies or Tissue biopsies Specimens known to contain contaminating flora: Gastric lavage, Bronchial washings & Urine L J MEDIA CORD LIKE GROWTH OF M.TB. IN MEDIA NEWER CULTURE METHODS for M.TB. • Microscopic Observation of Broth Culture & • MODS Micro Colony Detection System (slide culture) • Septi-check AFB : Non radiometric, Non automated • MGIT 960 : Automated. monitors every 60min. O2 utilization, Intensification of O2 quenching fluorescent dye • MB/BAC T - ALERT : Non radiometric, colorimetric detection of CO2 • BACTEC Radiometric BACTEC 460 TB System(radio metric) Developed in 1969 by Deland and Wagner. Principle BACTEC 12B vial , utilize 14C labeled substrate (fatty acid) On inoculation, mycobacteria, grow & release 14CO2. The BACTEC instrument measures quantitatively the radioactivity on a scale ranging from 0-999, as GI.(Growth Indicator) The daily increase in GI is proportional to growth in the medium. DST Drug Susceptibility Test When ATT is introduced in the medium reduced production of 14CO2 and decrease in GI. MB BACT-ALERT 3D LIGHT EMITTING SENSORS The MGIT 960 System The MGIT 960 system is a non-radiometric automated system that uses the MGIT media & sensors to detect the fluorescence. Advantages: -The system holds 960 plastic tubes which are continuously monitored. - Early detection with the machine monitoring & reading the tubes every hour. II Mycobacteria Growth Indicator Tube (MGIT) Tube contains modified Middle brook 7H9 broth base with OADC enrichment & PANTA antibiotic mixture. All types of clinical specimens, pulmonary as well as extra-pulmonary ( except blood ) could be cultured on this type of media. The OADC supplement O ----- Oleic acid ( Metabolic stimulant) A ----- Albumin ( to bind toxic free fatty acid ) D ---- Dextrose (Energy source ) C ----- Catalase ( Destroy toxic peroxides that may be present in the medium ) The PANTA antibiotic mixture P ---- Polymyxin B A ---- Amphotericin B N ---- Nalidixic acid T ---- Trimethoprim A ---- Azlocillin +/- Vancomycin The antibiotic mixture inhibits the growth of contaminating bacteria. Principle of the procedure:(MGIT) A fluorescent compound (which is sensitive to O2) is embedded in silicone on the bottom of the tube. The actively respiring microorganisms consume the oxygen & allow the fluorescence to be observed using UV trans-illuminator lamp. III Polymerase Chain Reaction (PCR) & Gene probe Nucleic acid Amplification Tests polymerase enzymes amplify specific DNA sequences, using Nucleic acid probes, using DNA extracted from MTB in the sample. Advantages: - Rapid procedure ( 3 – 4 hours) - High sensitivity (1-10 bacilli / ml sputum) CDC recommends NAAT for all suspected TB cases PCR ASSAY The thermal cycling, DNA melting separates the strands of DNA double helix at 95°C Heat-stable DNA Taq polymerase, ( Bacteria Thermus aquaticus.) Enzymatically assembles new DNA strands(selectively amplify ) using DNA primers ( DNA oligonucleotides.) & template(each strand) at 55 °C The selectivity of PCR results from the use of primers that are complementary to the DNA region targeted for amplification under specific thermal cycling conditions. RR REALTIME-PCR ASSAY • A TB specific primer and probe mix is provided and this can be detected through the FAM channel. • The primer and probe mix exploits the so-called TaqMan® principle. • During PCR amplification, forward and reverse primers hybridize to the TB DNA/Cdna • . A fluorogenic probe is included in the same reaction mixture , it consists of a DNA probe labelled with a • 5`-dye (reporter) and a 3`-quencher. (5’3’DQ) • During PCR amplification, the probe is cleaved and the Reporter dye and Quencher are separated. • The resulting increase in fluorescence can be detected on a range of real-time PCR platforms PCR ASSAY • The PrimerDesign™ genesig Kit for Mycobacterium Tuberculosis (TB) Genomes is designed • for the in vitro quantification of TB genomes. • The kit is designed to have the broadest detection profile possible whilst remaining specific to the TB genome. • The primers have 100% homology with all other reference sequences in the NCBI database. • Fig 1 Accession numbers for detected TB isolates. • CP000717.1, CP000611.1, AM408590.1, U43540.1, AE000516.2, BX842583.1, BX842577.1, • BX842572.1, BX248339.1, U35021.1, U35017.1, AF041819.1, BX248346.1, BX248334.1, Disadvantages: - Very expensive. - Require specialist training & equipment. - False positive results.( CONTAMINATION) - Can not differentiate between living & dead bacilli. . - Sputum specimens (3%--7%) might contain inhibitors that prevent or reduce amplification and cause false-negative NAA results. RAPID RECOGNITION OF DRUG RESISTANCE • PCR PROBES ARE AVAILABLE • • • • KAT-gene INH RESISTANCE RPO gene RIFAMPICIN RESISTANCE GYR –A FLUROQUINOLOE RESISTANCE LIPA( Line Probe Assay ) amplified DNA is applied to strips with probe for M.TB. And Rif. resistance MODS versus other culture methods* Method Pos.each Pos. by Method(%) atleast one cult.(%) Sens. % Median detection days Auramine 0 76 98 78 MODS 89 97 92 9 (4-31) MGIT 88 95 93 10 (3-39) LJ 73 96 76 24 ( 6-59) Micro COL 7H11 75 96 78 14.5(4-28) PCR 81 90 90 * Based on 172 samples Caviedes.L. et al J..Clin.Microbiol. 2000, 38, 1203 Identification of M. tuberculosis from the growth Growth temperature 35o-37oC only No pigmentation Niacin positive Catalase negative at 68oC No growth on LJ medium containing PNB Positive reaction for nitrate reduction Differentiation of Mycobacteria Colony morphology M.tuberculosis NTM Rough, eugonic Mostly smooth Growth at 37oC + +/ - Growth at 25oC - + Pigmentation - +/ - Niacin + - PNB - + Nitrate reduction + - Catalase at 68oC - + Can high drug dosage still have an effect on resistant strains? Isoniazid Mutants katG – high MIC inhA – low MIC Quinolones Mutants Mainly in gyrA – low MIC Early clinical trial Guinea-pig study Evaluation of different methods of diagnosis As regards the time: MGIT shortest time to positivity at 13.3 days BACTEC 460 system 14.8 days & for L J medium 25.6 days . As regards the no. of culture yield: The best yield, was with BACTEC 460, followed by BACTEC MGIT 960 , & then with L J medium. As regards contamination rate: L J medium (17%) had the highest contamination rate (Tortoli E, Cichero P,Et al. 1999) then the MGIT 960 ( 10.0% ) Compared with radiometeric system (3.7%) SUMMARY Useful newer modalities 3idiots? • QUANTIFERON-TB GOLD • MB BACT-ALERT 3D LIGHT EMITTING SENSORS • PCR PROBES for antibiotic resistance • INH,REF,ETH,FLORO Q Tuberculosis (TB) Diagnostic Tests in Use, Recently Endorsed by the World Health Organization (WHO), and in Later Stages of Development. Dorman S E Clin Infect Dis. 2010;50:S173-S177 © 2010 by the Infectious Diseases Society of America Tuberculosis (TB) Diagnostic Tests in Use, Recently Endorsed by the World Health Organization (WHO), and in Later Stages of Development. • BACTEC Myco/F�Sputa Culture Medium, for use with the BACTEC 9000MB System to detect mycobacteria species in clinical samples. • BACTEC Myco/F Lytic. • • • • • • • • • • • • • Dogra S, Narang P, Mendiratta DK, Chaturvedi P, Reingold AL, Colford JM Jr, Riley LW, Pai M. Comparison of a whole blood interferon-gamma assay with tuberculin skin testing for the detection of tuberculosis infection in hospitalized children in rural India. J Infect 2007; 54:267–76. An Indian study that compared QFT to the TST in 105 children who were suspected of having TB, or had contact with an index case. In this study 11 children (10.5%) were QFT positive, whereas the TST was positive in 15 (15%) at ≥5mm, 11 (10.5%) at ≥10mm, or 4 (4%) at ≥15mm. Concordance of TST with QFT was high (95%) at the 10mm TST cut-off. All ≥15mm TST subjects were QFT positive. There were no indeterminate QFT results, despite 40% of the children being <4 years old and 57% of them being malnourished. SUMMARY IGRAs are recommended for 1. Contacts of active TB Close contacts (HIGH RISK) can get both TST and IGRA and if either is positive, be treated for LTBI Casual contacts (LOW RISK) can have IGRA confirmation if TST positive to verify infection vs BCG or MOTT 2. Immune compromised TST first, if negative do IGRA and if IGRA positive treat as LTBI 3. Low risk people who are TST positive Do an IGRA, if positive consider as LTBI FIND and Carl Zeiss Micro Imaging GmbH have co- developed a fluorescent LED microscope based on the proven Primo Star platform. FIND/Zeiss microscope offers superior optics, reflected light illumination, easy switch from brightfield to fluorescent light Components of the post-research-and-development process for promising new tuberculosis (TB) diagnostic technologies. Dorman S E Clin Infect Dis. 2010;50:S173-S177 © 2010 by the Infectious Diseases Society of America Reporting of culture results Report Reading No Growth • Negative 1 – 19 colonies • Positive • Positive (1+) • Positive (2+) • Positive (3+) • Contaminated 20-100 colonies >100 colonies Confluent growth Contaminated ( No.of colonies) INDIAN STUDY USING QUANTIFERONTB GOLD • Dogra S, Narang P, Mendiratta DK, Chaturvedi P, Reingold AL, Colford JM Jr, Riley LW, Pai M. Comparison of a • whole blood interferon-gamma assay with tuberculin skin testing • for the detection of tuberculosis infection in hospitalized • children in rural India. J Infect 2007; 54:267–76. • Compared QFT to the TST in 105 children ( suspected of TB, or had contact with an index case). • • • • 11 children (10.5%) were QFT positive, whereas the TST was positive in 15 (15%) at ≥5mm, 11 (10.5%) at ≥10mm, or 4 (4%) at ≥15mm. Concordance of TST with QFT was high (95%) at the 10mm • TST cut-off. All ≥15mm TST subjects were QFT positive. • There were no indeterminate QFT results, despite 40% of the children • being <4 years old and 57% of them being malnourished. Thank you