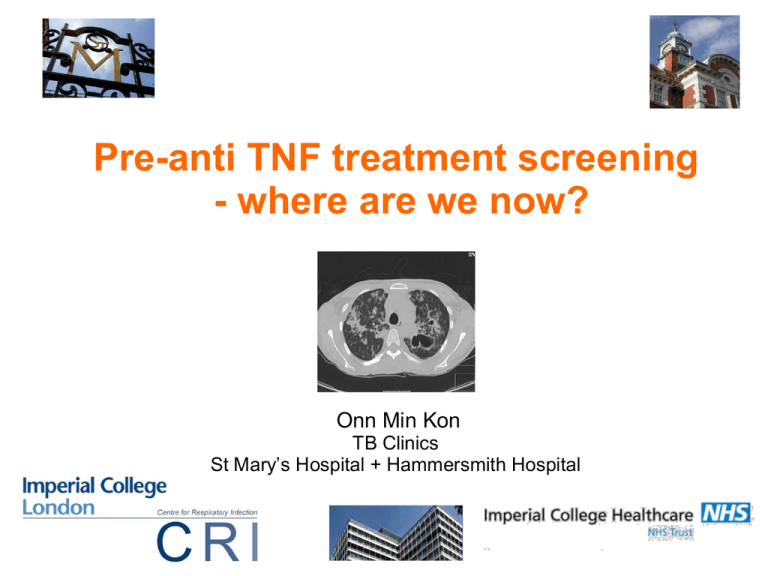
Pre-anti TNF treatment screening
- where are we now?
Onn Min Kon
TB Clinics
St Mary’s Hospital + Hammersmith Hospital
Latent TB Infection
in Rheumatological Conditions
An ongoing debate…….
• Epidemiology
• How do we evaluate LTBI?
TST
IGRA
CXR
Mouse
binding site
for TNF-
k
Anti-TNF- therapies
k
Infliximab (Remicade) Human (IgG1)
chimaeric MoAB
Adalimumab (Humira) fully human MoAB
Golimumab (Simponi) human IgG1 k MoAB
Certolizumab pegol (Cimzia) PEGylated Fab' fragment of a humanized TNF inhibitor MoAB
Enbrel (Etanercept) :
soluble TNF-receptor
dimeric p75 TNFR
bound to Fc of IgG1
Post 4 months anti-TNF
Infliximab and TB
Keane et al, NEJM 2001
– 70 reported cases from 147,000 given infliximab
worldwide between 1998-2001
– 40 (56%) extra-pulmonary TB (US rate 18%)
– 17 (24%) disseminated TB (US rate < 2%))
– Most within 3 treatment cycles (median 12 wks)
– No granuloma in lung biopsy in one patient
– Probable reactivation
– 64/70 patients from areas of low incidence (< 20 per
100,000)
Different risks associated with specific agents
Tubach et al Arthritis Rheum 2009 French registry data 3y on TB
• Case control analysis to investigate risk of TB
associated with specific anti-TNF agents
• 69 patients (40 RA, 18 spondyloarthritides, 9
inflammatory colitis, 1 psoriasis) treated with various
anti-TNF agents
• Standardised incidence ratios of TB:
Infliximab
18.6 (13.4-25.8)
Adalimumab
29.3 (20.3 – 42.4)
Etanercept
1.8 (0.7 -4.3)
Risk of tuberculosis in patients with rheumatoid arthritis in
Hong Kong - the role of TNF blockers in an area of high
tuberculosis burden
RA compared to the general population Hong Kong 2004 and 2008
2441 RA patients followed at the 5 centres
Standardised Incidence Ratio Active TB - TNF naïve RA: 2.35, 95% CI 1.17-4.67, p=0.013
- TNF treated RA: 34.92, 95% CI 8.89-137.20, p<0.001
Independent variables associated with increased risk of active TB
- older age at study entry (RR 1.05, p=0.013)
- a past history of pulmonary TB (RR 5.48, p=0.001)
- extra-pulmonary TB (RR 16.45, p<0.001)
- Felty's syndrome (RR 43.84, p=0.005)
- prednisolone>10mg daily (RR 4.44, p=0.009)
- TNF blockers (RR 12.48, p<0.001)
Tam LS et al. Clin Exp Rheumatol. 2010 Sep-Oct;28(5):679-85
Different risks associated with specific agents
British Society for Rheumatology Biologics Registry (BSRBR)
• adalimumab (144 events/100 000 pyrs)
• infliximab (136 events/100 000 pyrs)
• etanercept (39 events/100 000 pyrs)
IRR compared with etanercept-treated patients
- infliximab was 3.1 (95% CI 1.0, 9.5)
- adalimumab 4.2 (95% CI 1.4, 12.4)
Risks associated with different countries
Infliximab
• Spanish registry
1113 per 100 000
• Korea
2558 per 100 000
• Japan
325 per 100 000
• Portugal
1500 per 100 000
• USA
• Sweden
62 per 100 000
145 per 100 000
Analysis database of linked statistical records :
Hospital admissions and death certificates for the whole of England (1999 to 2011)
+ Oxford Record Linkage Study - southern England
Rate ratios for TB comparing immune-mediated disease cohorts with comparison cohorts
Particularly high levels of risk :
• Addison's disease (rate ratio (RR) = 11.9 (95% CI 9.5 to 14.7))
• Goodpasture's syndrome (RR = 10.8 (95% CI 4.0 to 23.5))
• SLE (RR = 9.4 (95% CI 7.9 to 11.1))
• polymyositis (RR = 8.0 (95% CI 4.9 to 12.2))
• polyarteritis nodosa (RR = 6.7 (95% CI 3.2 to 12.4))
• dermatomyositis (RR = 6.6 (95% CI 3.0 to 12.5))
• scleroderma (RR = 6.1 (95% CI 4.4 to 8.2))
• autoimmune hemolytic anemia (RR = 5.1 (95% CI 3.4 to 7.4))
•
•
•
•
Rheumatoid Arthritis RR 3.2
Ankylosing spondylitis RR 4.2
Crohn’s RR 3.7
Psoriasis RR 2.6
Corticosteroids and risk of TB
Arthritis Rheum. 2006 Feb 15;55(1):19-26.
Glucocorticoid use, other associated factors
and the risk of tuberculosis.
Jick SS, Lieberman ES, Rahman MU, Choi HK.
•
•
•
•
•
•
Case-control TB cases 1990-2001 - UK GP Research Database
4 controls were matched to each case
497 new cases of tuberculosis and 1,966 controls derived from 16,629,041
person-years at risk (n = 2,757,084 persons)
Adjusted odds ratio TB for current use glucocorticoid compared with no use was
4.9 (95% confidence interval [95% CI] 2.9-8.3)
<15 mg 2.8 (95% CI 1.0-7.9)
>15 mg of prednisone or its equivalent daily dose were and 7.7 (95% CI 2.8-21.4)
AOR of TB 2.8 for patients with BMI <20 compared with normal
AOR
1.6 for current smokers compared with nonsmokers
3.8 history of diabetes
3.2 emphysema
2.0 bronchitis
1.4 asthma
(all P values <0.05)
Agent
Adjusted RR
Any DMARDs
3.0
MTX
3.4
Leflunomide
11.7
Cyclosporine
3.8
Other
1.6
Corticosteroids
2.5
Arthritis Rheum. 2009 Mar 15;61(3):300-4.
Rheumatoid arthritis, its treatments, and the risk of tuberculosis in Quebec, Canada.
Brassard P et al.
So how do we diagnose LTBI in pre-TNF cases?
The missing ‘gold standard’
So how do we diagnose LTBI in pre-TNF cases?
BTS 2005 – pre IGRA
Recommendations for
assessing risk and for
managing
Mycobacterium
Tuberculosis infection
and disease in
patients due to start
anti-TNF-a treatment.
Thorax 2005;60:800-805
• If immunosuppressed
no TST – risk stratify only
• If not immunosuppressed
even if TST positive – risk
stratify
If negative TST – no action
Example Risk Tables
Case type
Annual risk
of TB
/100,000
TB risk
adjusted
x5 for anti
TNF
Risks of
prophylaxis
/100,000
Risk/
Benefit
conclusion
White
age 55-74
UK born
7
35
278
Observe
Indian Sub continent
age>35
In UK 3 years
593
2965
278
Chemo
Prophylaxis
Black African
Age 35-54
168
840
278
Chemo
Prophylaxis
Other ethnic
Age 35+
In UK>5 years
39
195
278
Observe
Epidemiology versus risk of treatment
• ‘Individual’ risk
―
Prior LTBI/ TB - never treated
―
Close contact
• ‘Population’ risk
―
Ethnicity
―
Country of birth
―
Where one lives
Plain CXR
Evidence of LTBI?
Tuberculin Test
US statistics on latent TB activation and Mantoux
TST is attenuated in RA
Treatment of TST positive RA cases
post implementation of screening
reduced TB incidence
INH 9 months given if:
1) history of untreated or partially treated TB, or exposure to an active TB case
2) CXR showing residual changes indicative of prior TB infection
3) reaction of 5 mm in diameter TST or 2-step TST ( 359 patients - 28%)
risk ratio for the incidence of active TB, compared with the
background population, before March 2002 was 25.15 (95% CI
14.05–45.17) and dropped 74% to 6.72 (95% CI 0.16–41.07)
following the official recommendations date
2004 Interferon-gamma release assays - new biomarkers of TB infection
ELISpot
quantification IFN-g-releasing cells
ELISA
quantification released IFN-g
• ELISA versus TST
associated better with risk
factors for LTBI
• ELISA poorly correlated to TST
• ELISA less affected by BCG
― Used 5mm cutoff (?higher TST
+ve rate)
― TST remote to IGRA
― Swiss Hospital
― High (83%) BCG vaccinated
― TST still had a positive
association
Comparison of an interferon-gamma assay with tuberculin skin testing
for detection of tuberculosis (TB) infection
in patients with rheumatoid arthritis in a TB-endemic population.
Lima Peru
101 RA patients and 93 controls
5mm cutoff on RA/ 10mm in controls
• QFT comparable between RA and controls (44.6% vs 59.1% NS)
• TST significantly less in RA (26.7%) than controls (65.6%)
Ponce de Leon et al
J Rheumatol. 2008 May;35(5):776-81.
Overall IGRA in place of TST halved those receiving chemoprophylaxis
In ‘LTBI’ (CXR and/or history of contact) -
Mariette X et al.
Multi-centre
French Study
•
Patients in 62 German rheumatology centres - screened TST and IGRA (TSPOT or
QFT)
•
1529 - TST, 844 - TSPOT and 685 - QFT
• ‘LTBI’
•
8.0% - positive TST and no previous BCG
7.9% - positive IGRA
11.1% Combination
Clinical risk factors (CRF) for LTBI in 122 patients
TST influenced by CRF (OR 6.2; CI 4.08 to 9.44, p<0.001) and BCG vaccination
status (OR 2.9; CI 2.00 to 4.35, p<0.001)
QFT and TSPOT only influenced by CRF (QFT: OR 2.6; CI 1.15 to 5.98, p=0.021;
TSPOT: OR 8.7; CI 4.83 to 15.82, p<0.001)
• ‘In patient populations with low rates of TB incidence and BCG
vaccination, the use of both TST and IGRA may maximise sensitivity in
detecting LTBI but may also reduce specificity’
Prignano F
Florence, Italy
Combined TST and IGRA highest sensitivity
Overlapping positives and context
All
BCG naive
BCG
Hsia et al.
Even small doses of steroids affect QFT
A UK study
Singanayagam A et al. Thorax 2013;68:955-961
Overlapping yield for tests when mutually positive.
Singanayagam A et al. Thorax 2013;68:955-961
Copyright © BMJ Publishing Group Ltd & British Thoracic Society. All rights reserved.
3/7 triple positive
2/7 TST only
2/7 double IGRA only
(total 5/7 double IGRA)
Case 1
48 year old woman (?ethnicity) with IBD
TST negative / Tspot indeterminate
No prophylaxis – stopped Infliximab
Three months later
- Travelled in country incidence 101 per 100 000
Returned - TB meningitis 5 weeks later and died 2 weeks later
Case 2
41 year old Moroccan man with Ankylosing Spondylitis
TST/Tspot negative - Infliximab
Travelled to Morocco (approximately 82 per 100,000) 6 weeks
Returned 3 months later EPTB - M.bovis
Thorax 2013 68: 1079-1080
What we think we know in inflammatory disease……
•
•
•
•
•
•
Differential effect of anti-TNF treatment - type and setting
Steroids and Immunosuppression affects IGRA and TST sensitivities
IGRA more specific than TST
IGRA and TST in inflammatory disease - only minor overlap
QFT versus T Spot in inflammatory disease - some overlap
Epidemiology and TST or IGRA - only minor overlap
• ?Double and triple tests increase ‘sensitivity’
• In moderate to high prevalence or risk factors > 1 mode
• In low incidence or no risk factors + immunocompetent –
- 1 mode reasonable as likely low false negative (?IGRA)
• Patients develop TB - post negative screening
BSR 2010
Recommendation 4: prior to commencing treatment with anti-TNF
therapy, all patients should be screened for mycobacterial infection
in accordance with the latest National guidelines. Active mycobacterial
infection needs to be adequately treated before anti-TNF therapy can be
started. (Level IIb evidence, Grade of recommendation B.)
Recommendation 5: prior to commencing anti-TNF therapy,
consideration of prophylactic anti-TB therapy (as directed by the
latest National guidelines) should be given to patients with
evidence of potential latent disease (past history of TB or abnormal
chest X-ray). (Level IIb evidence, Grade of recommendation B.)
Recommendation 6: all patients commenced on anti-TNF therapies
should be closely monitored for mycobacterial infections. This
should continue for at least 6 months after stopping treatment due to the
prolonged elimination phase of the drug. (Level IV evidence, Grade of
recommendation C.)
Anti-TNF and TB screening
- suggested approach
• Use IGRA/ TST/ CXR – chemoprophylaxis if
any positive
• If negative and immunosuppressed use epidemiological risk factors and history of
recent exposure/ new entrant + balance
treatment risk
• Newly acquired infection and repeat
screening: no guidance
• Need to have high index of suspicion for TB
Symptoms suggest
active TB/contact history or
previous history
of untreated TB/abnormal
chest radiograph?
Yes
No
Fully investigate to rule out TB
OR
Perform TST and IGRA and
risk assess using BTS risk
stratification tables
Offer chemoprophylaxis if no
active TB and prior untreated
or evidence granulomas
Either test positive
or high risk
All tests negative and
low risk
Treat with chemoprophylaxis
New entrant to UK < 5 years
AND on
immunosuprressants?
Yes
‘Imperial’ Model
No
Risk assess by using
originating country rates
High risk
Treat with chemoprophylaxis
low risk
No treatment required
Sester 2014 – a TBNet study
AJRCCM
In RA:
• Indeterminates QFT>Elispot
• More +ve TST>IGRAs
• All 3 tests
• Best correlation IGRA to IGRA
• Lesser correlation TST to either IGRA
Sester et al 2014 in press AJRCCM
•
•
•
•
•
Mixed conditions – retrospective
Some given chemoprophylaxis
Test modality – none ideal
TST most predictive in HIV
All who were given chemoprophylaxis - none
progressed
IGRA in all - Is it cost effective?
BSR 2013
• At the age of 50 years UK White Caucasian population
- incidence of active TB disease 5/100 000
- incidence of latent TB is approximately 10 times this level (50/100 000)
- Number of tests to detect 1 case LTBI 2000
- (£70 000 Quantiferon and £200 000 T-spot)
• Cost effectiveness better in older patients
• Cost effectiveness worse (more than double the cost) < 35 years
• Cost-effectiveness better for ethnic minorities
- South Asia 120/100 000 numbers needed to test 82
- black Africans 240/100 000 numbers needed to test 41
‘The true-negative predictive value of a negative test or the true-positive
predictive value of a positive test is still not known,’
29 year old woman RA
• sulphasalazine and hydroxychloroquine (MTX
prior)
• UK born caucasian
• No TB contacts/ HIV negative
• Holidays - Sri Lanka 2009/ Egypt 2010
• Oct 2013 – CXR NAD/ TST and IGRA non
reactive
• Nov 2013 – Infliximab
Progress….
• BAL negative but commenced Rx for TB
• EBUS – non caseating granuloma/ PCR and smear
negative
• Culture positive
• Visited Sri Lanka pre screening – 66 per 100,000
• Visited Egypt pre screening – 17 per 100,000
• Lives in Brent - 100.6 per 100,000
Summary points
• Immune mediated disease - higher risk for TB
• Some other therapies increase risk of progression
• Screen for LTBI/TB before initiating steroids/immunosuppressive
treatment/anti-TNF
• Effect of steroids and DMARDs on tests
• Most ‘sensitive’ approach is tri-modality (TST/IGRA/CXR)
• IGRA more specific (+ more practical?) but prognosis unclear
• Epidemiology useful once on immunosuppressants
• Rifampicin/Isoniazid 3 months OR Isoniazid 6 months if drug
interactions important
• Consider rescreen if new exposure or travel
• Vigilance even in ‘screen negatives’
Unanswered questions
in pre-TNF screening
•
•
•
•
•
Prognostic value of a TST+ve/ IGRA –ve test?
Prognostic value of a TST-ve/ IGRA +ve test?
What is the utility of just using a TST or IGRA?
Hepatotoxicity in this cohort
Cost effectiveness of mode of approach in low versus
high incidence settings or individuals
• How do we quantitate high risk travel?
• How do we rescreen?
We think we know what we don’t know…
NICE due 2015…..
https://www1.imperial.ac.uk/nhli/training/educationcentre/shortcourses/london_tb/