Hypoxia & Hyperventilation
advertisement
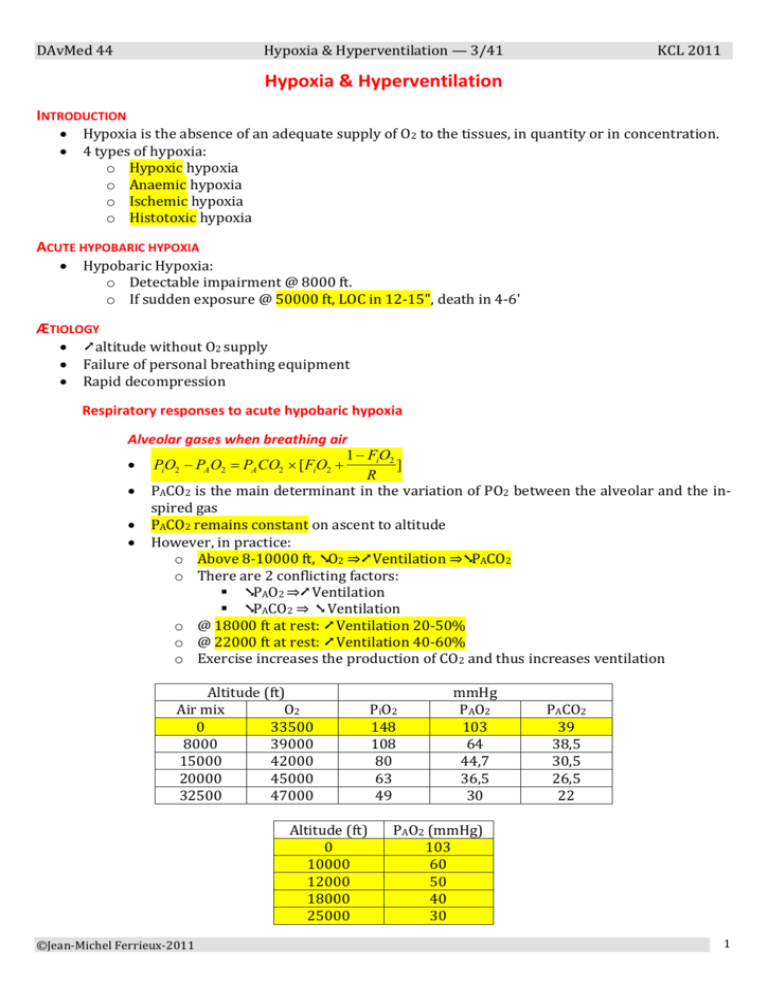
DAvMed 44 Hypoxia & Hyperventilation — 3/41 KCL 2011 Hypoxia & Hyperventilation INTRODUCTION Hypoxia is the absence of an adequate supply of O2 to the tissues, in quantity or in concentration. 4 types of hypoxia: o Hypoxic hypoxia o Anaemic hypoxia o Ischemic hypoxia o Histotoxic hypoxia ACUTE HYPOBARIC HYPOXIA Hypobaric Hypoxia: o Detectable impairment @ 8000 ft. o If sudden exposure @ 50000 ft, LOC in 12-15", death in 4-6' ÆTIOLOGY ➚ altitude without O2 supply Failure of personal breathing equipment Rapid decompression Respiratory responses to acute hypobaric hypoxia Alveolar gases when breathing air 1 FiO2 ] PiO2 PA O2 PA CO2 [FiO2 R PACO2 is the main determinant in the variation of PO2 between the alveolar and the inspired gas PACO2 remains constant on ascent to altitude However, in practice: o Above 8-10000 ft, ➘O2 ⇒➚ Ventilation ⇒➘PACO2 o There are 2 conflicting factors: ➘PAO2 ⇒➚ Ventilation ➘PACO2 ⇒ ➘ Ventilation o @ 18000 ft at rest: ➚ Ventilation 20-50% o @ 22000 ft at rest: ➚ Ventilation 40-60% o Exercise increases the production of CO2 and thus increases ventilation Altitude (ft) Air mix O2 0 33500 8000 39000 15000 42000 20000 45000 32500 47000 Altitude (ft) 0 10000 12000 18000 25000 ©Jean-Michel Ferrieux-2011 PiO2 148 108 80 63 49 mmHg PAO2 103 64 44,7 36,5 30 PACO2 39 38,5 30,5 26,5 22 PAO2 (mmHg) 103 60 50 40 30 1 DAvMed 44 Hypoxia & Hyperventilation — 3/41 Alveolar gases when breathing oxygen After washing out N2 PAO2 = [PB - PH2O] - PACO2 PH2O = 47 mmHg (in the body @ 37°C) In aviation, there often remains 3-5 mmHg N2, one must consider a ➘ PO2 of 3-5 mmHg If 100% O2 is delivered, ⇒ PAO2 103 mmHg @ 33500 ft (equivalent to sea level) o Physiologically equivalent altitudes KCL 2011 so Alveolar gases during rapid decompression ➘ PB ⇒ ➘ PA of the different constituents o ⇒ ↓↓ in PAO2 o If rapid decompression from 8000 to 40000 ft within 1.6": PAO2 falls from 65 to 15 mmHg PvO2 > PAO2 ⇒ large diffusion of O2 from pulmonary blood to the expired air o ⇒ Concept of critical level of PAO2 30 mmHg and critical area under 30 mmHg where there is a high risk of LOC if the area is > 140 mmHg/s o The higher the final altitude + the longer the exposure ⇒the greater the degree of hypoxia o PAO2 at altitude must not fall below 30 mmHg (critical level) o ⇒ to avoid neurological disturbances after rapid decompression, 100% O2 must be breathed before the rapid decompression, or at least be delivered within 2 seconds after the onset of the decompression. Arterial blood gases At rest, the PaO2 leaving the pulmonary capillaries is equal to the PAO2 Altitude (ft) @ rest Air mix O2 PaO2 SaO2 PaCO2 0 33500 95 97% 39-40 11000 40000 45 85% 15-16000 42-43000 36 76 30 Large individual variations @ exercise, there is a ➘ of transit time of blood in the pulmonary capillaries ⇒ ➘ PaO2 & SaO2 Cardiovascular responses Blood flow Blood flow is the cardinal determinant of the tension at which O2 is delivered to the cells ©Jean-Michel Ferrieux-2011 2 DAvMed 44 Hypoxia & Hyperventilation — 3/41 General cardiovascular changes @ rest: Immediate ➚ heart rate when breathing air above 6000-8000 ft: o @ 15000 ft, ➚ of 10-15% o @ 20000 ft, ➚ of 20-25% o @ 25000 ft, ➚ of 100% There is a proportional ➚ in cardiac output The mean arterial blood pressure (BP) remains unchanged, but: o ➚ BPsyst o ➘ peripheral resistance o ➚ pulse pressure KCL 2011 Regional cardiovascular changes Immediate ➚ blood flow through the coronary & cerebral circulations o ➘ renal flow o ➘ viscera flow o ➘ skin flow o ⇒Redistribution of the cardiac output The coronary flow increases in parallel with the cardiac output and is effective ++ o @ 25000 ft breathing air ⇒no ischemic signs on the ECG @ PaO2 > 45-50 mmHg, the cerebral flow is determined by: o PaCO2 with a 1-to-1 effect: If PaCO2 ➘ from 40 to 20 mmHg ⇒➘ cerebral flow by ½ o If PaO2 < 45 mmHg ⇒hypoxic vasodilatation (VD) o If PaO2 = 35-40 mmHg ⇒➚ cerebral flow by 50-100% o There is a balance on cerebral flow between: VD effect of hypoxia VC influence of hypocapnia From 0 to 15000 ft breathing air ⇒ ➘ cerebral blood flow From 16000 to 18000 ft breathing air ⇒ ➚ cerebral blood flow Pulmonary circulation: o With exposure to hypoxia such as there is a 20% ➘ of SaO2 ⇒Reversible VC in the pulmonary circulation. Syncope In 20% of individuals, the immediate cause of LOC is the failure of cerebral blood flow subsequent to a major fall in arterial BP associated with deep bradycardia. Associated symptoms: o pallor o sweating o nausea ± vomiting Tissue oxygen tension The minimum acceptable PO2 in a tissue depends on the tension of O2 in the blood flowing its capillaries. The form of the oxygen dissociation curve explains the rate of fall of PO2 under hypoxia o Protective effect of the haemoglobin (Hb) combination with O2 ©Jean-Michel Ferrieux-2011 3 DAvMed 44 Hypoxia & Hyperventilation — 3/41 KCL 2011 Cyanosis Cyanosis is caused by the presence of an increased concentration of reduced Hb (Hb R) in the capillaries and venules of hypoxic tissues. > 5g HbR/100ml blood ⇒ cyanosis ⇒cyanosis is an unreliable sign of hypoxia o ➘ if anaemia o ➚ if polycythaemia Neurological effects Impairment of mental performances It's of great practical significance in aviation, but with great variability. Variations are due to the variations in the respiratory response to hypoxia o ➘ PaO2 ⇒ ➘ PaCO2 (by hyperventilation—HV) ⇒ ➘ cerebral flow ⇒ ➘ cerebral PO2 o ⇒ ➘ mental performance Psychomotor tasks Well learned and practised tasks are generally preserved until > 10000 ft If PAO2 < 38-40 mmHg (16-18000 ft) ⇒the reaction time ➚ (by 50% if PAO2 35 mmHg) Performance at pursuit-meter tasks are unaffected until > 12-14000 ft Choice-reaction time is impaired ++ @ 12000 ft Also consider the effect of muscular coordination impairment (tremor @ 15000 ft) Cognitive tasks Previously learned tasks are unaffected until > 10000 ft (55 mmHg) But there is a decline at lower PAO2 o 10-15% @ 15000 ft o 40-50% @ 18000 ft Short term & long term memory is affected at as low altitudes as 8-10000 ft (60 mmHg) @ 8000 ft ⇒ ➘ performance at novel tasks (twice the time for complex reaction-choice tasks) Such changes can be demonstrated at altitudes as low as 5-6000 ft. Impairment of special senses Vision o Subjective darkening of the visual fields (VF) which is actually noticed after O2 restoration (environment seems then much brighter) o @ 5000 ft ⇒➘ light sensitivity of the dark-adapted eye (scotopic vision) o Scotopic vision is significantly impaired @ PAO2 < 50 mmHg (12000 ft) o Photopic vision (bright light vision) is unaffected until PAO2 < 40 mmHg (18000 ft) o A moderate to severe hypoxia ⇒ ➘ VF (tunnelling) and appearance of a central scotoma Audition o ➘ auditory acuity by moderate to severe hypoxia Lost of consciousness (LOC) There is a very close correlation between PvJO2 (jugular) and the level of consciousness o LOC occurs when PvJO2 < 17-19 mmHg (PAO2 < 30 mmHg) o LOC may occur @ PAO2 40 mmHg associated with hyperventilation ©Jean-Michel Ferrieux-2011 4 DAvMed 44 Hypoxia & Hyperventilation — 3/41 KCL 2011 Effects during rapid decompression Rapid decompression (RD) to > 30000 ft breathing air ⇒ ➘++ PAO2 < 30 mmHg o ⇒ very profound neurological effects (LOC if the subject remains < 30 mmHg with a "critical" area > 140 mmHg/s Time before decrement in performance is about 12-15" after RD If 100% O2 is provided within 8" after the RD @ 40000 ft, the performance is recovered to control level after 60" If PAO2 never falls < 30 mmHg and rises rapidly with O2 ⇒performance is maintained o ⇒It is essential to maintain or restore rapidly a PAO2 > 30 mmHg Clinical features The speed, the order and the severity of symptoms depend on the rate, the degree and the duration of the exposure to hypoxia Great variations between individuals Factors influencing the clinical presentation: o Intensity of hypoxia (rate, maximum reached altitude, duration) o Physical exertion ⇒ ➘ tolerance to hypoxia o Ambient temperature: cold T° ⇒ ➘ tolerance to hypoxia o Drugs, alcohol, antihistamins: ⇒ ➘ tolerance to hypoxia Clinical picture 0-10000 ft breathing Air (39000 ft with oxygen) No symptoms @ rest Impaired performance at novel tasks 10-15000 ft Air (39-42500 ft oxygen) A warm resting subject would have no or few signs Impairment of performance at skilled tasks If the exposure is prolonged, ⇒headache There are symptoms if physical exertion and/or extreme T° 15-20000 ft Air (42500-45000 ft oxygen) There are signs @ rest Loss of critical judgment and willpower The subject is unaware of the deterioration Changes ++ in emotional state ⇒great importance in aviation ≈ OH intoxication Also consider the disturbances due to ➘ PaCO2 (hyperventilation) Physical exertion ➚++ the severity and speed of onset of symptoms > 20000 ft Ait (> 45000 ft oxygen) Marked ➚ of symptoms and signs Comprehension and performance fall rapidly LOC with little or no warning Myoclonic jerks, then convulsions Death Covert (early) cerebral features: Visual o ➘ light intensity o ➘ VA in poor illumination o ➚ light threshold ©Jean-Michel Ferrieux-2011 5 DAvMed 44 Hypoxia & Hyperventilation — 3/41 o ➘ visual fields Psychomotor o ➘ learning novel tasks o ➚ choice-reaction time o ➘ eye-hand coordination Cognitive o ➘ memory Overt features: Personality changes lack of insight loss of judgment & self-criticism euphoria ➘ memory mental incoordination sensory loss cyanosis hyperventilation and it's symptoms ➘ consciousness LOC Death Time of useful consciousness The TUC is the interval between ➘ PAO2 and the point at which there is a specified degree of impairment of performance. The main factor is the accepted degree of impairment. In practical, the TUC is the period during which the affected subject retains the ability to act to correct his/her predicament. At a given altitude, the TUC is shorter when due to rapid decompression than to slow ascent. o When breathing 100% O2 then air: Altitude (ft) 25000 30000 36000 KCL 2011 TUC 270" 145" 71" Recovery from hypoxia & the oxygen paradox The administration of O2 to a hypoxic subject usually results in rapid recovery. A generalized headache may persist if there was prolonged hypoxia. Some subjects may have a worsening of the symptoms during the first 15-60" of oxygenation. Occurs++ with hypoxic & hyperventilating (= hypocapnic) subjects. It is mostly important to maintain the oxygenation. ©Jean-Michel Ferrieux-2011 6 DAvMed 44 Hypoxia & Hyperventilation — 3/41 KCL 2011 HYPERVENTILATION Condition in which pulmonary ventilation is greater than that required to eliminate CO2 produced by the tissues. There is a close relationship between PCO2 and [H+] in blood and tissues CO2 + H2O ⇌H2CO3 ⇌H+ + HC O3 Aetiology Normal response to hypoxia (PO2 < 55-60 mmHg) Result of voluntary overbreathing ++ Emotional stress, anxiety (20-40% of student aircrew) Experienced aircrew if exposed to the mental stress of a sudden emergency Pain & motion sickness Environmental stress (T°, whole-body vibration @ 4-8 Hz) Pressure breathing. Physiological features of hyperventilation Hypocapnia of hyperventilation ➪has no significant effect on cardiac output or BP Hypocapnia induces VC++ in cerebral arterioles and vessels in the skin o ➚ blood flow in skeletal muscles o ➘➘ the minimum tissue O2 tension o ➪The many changes due to hyperventilation (including LOC) are due to a combination of hypoxia and alkalosis in the cerebral tissues. A reduction in PaCO2 < 25 mmHg causes significant decrement in the performance of psychomotor tasks o Such as tracking and complex coordination tests. o The ability to perform complex mental tasks is compromised by PaCO2 < 30 mmHg o Steadiness of the hands is impaired with PaCO2 = 25 mmHg o Manual tasks are impaired by muscular spasms when PaCO2 < 20 mmHg o Alteration of consciousness and LOC when PaCO2 < 10-15 mmHg. The rise in tissue pH induced by hyperventilation increases the sensitivity of PNS: o Paraesthesiae o Motor disruption Clinical features of hyperventilation Symptoms are manifest when PaCO2 is reduced to 20-25 mmHg: o Light headedness o Dizziness o Anxiety o Superficial paraesthesiae in the extremities and around the nose and lips When PaCO2 = 15-20 mmHg o Muscles spasms in the limbs and the face (carpo-pedal spasm) When PaCO2 < 15 mmHg o The whole body becomes stiff (tetany) The increased irritability of the nervous tissue ➪➚ tendon reflexes (Chvostek's sign) Finally, moderate and severe hyperventilation will produce a general deterioration in mental and physical performance, followed by impairment of consciousness and eventually LOC. If severe hyperventilation with LOC by anxiety,, the supervention of coma will be followed by a gradual recovery as respiration is inhibited and PaCO2 regains normal levels. This is not the case if hyperventilation is induced by hypoxia. ➪Hypoxia should always be suspected when signs of hypocapnia occur @ altitudes > 12000 ft. ©Jean-Michel Ferrieux-2011 7 DAvMed 44 Hypoxia & Hyperventilation — 3/41 KCL 2011 Hypoxia & Hyperventilation Introduction Acute hypobaric hypoxia Ætiology Respiratory responses to acute hypobaric hypoxia Alveolar gases when breathing air Alveolar gases when breathing oxygen Alveolar gases during rapid decompression Arterial blood gases Cardiovascular responses Blood flow General cardiovascular changes Regional cardiovascular changes Syncope Tissue oxygen tension Cyanosis Neurological effects Impairment of mental performances Psychomotor tasks Cognitive tasks Impairment of special senses Lost of consciousness (LOC) Effects during rapid decompression Clinical features Clinical picture 0-10000 ft breathing Air (39000 ft with oxygen) 10-15000 ft Air (39-42500 ft oxygen) 15-20000 ft Air (42500-45000 ft oxygen) > 20000 ft Ait (> 45000 ft oxygen) Time of useful consciousness Recovery from hypoxia & the oxygen paradox Hyperventilation Aetiology Physiological features of hyperventilation Clinical features of hyperventilation ©Jean-Michel Ferrieux-2011 8