OUTLINE Jaundice Drugs for Reducing bilirubin levels Causes of
advertisement
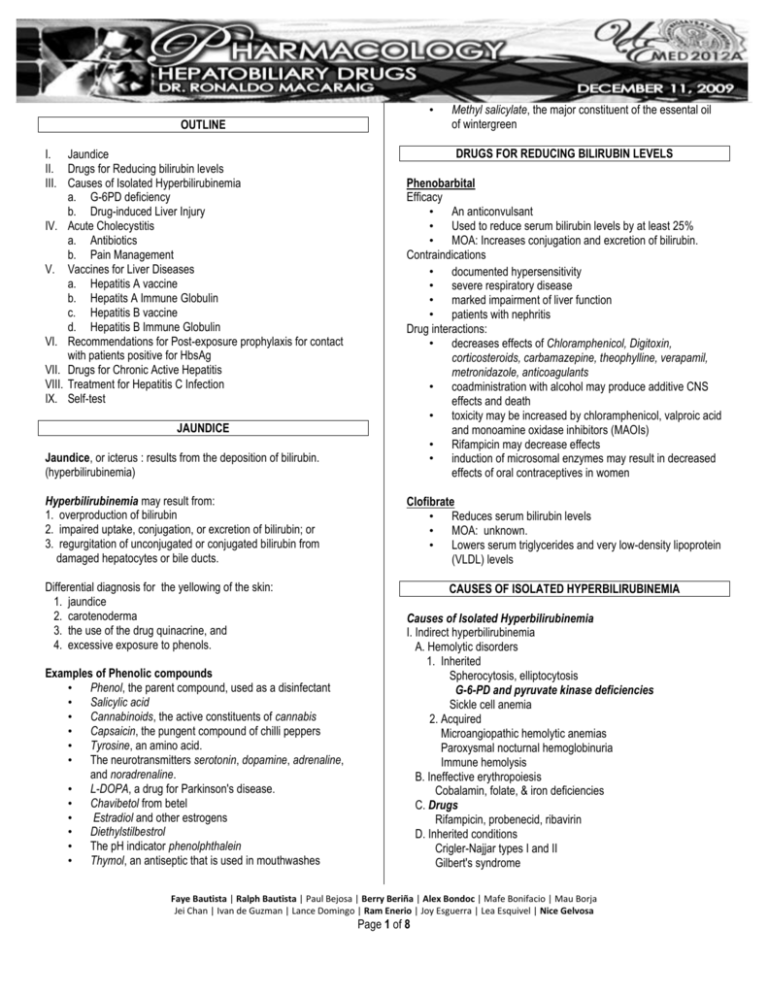
• OUTLINE I. Jaundice II. Drugs for Reducing bilirubin levels III. Causes of Isolated Hyperbilirubinemia a. G-6PD deficiency b. Drug-induced Liver Injury IV. Acute Cholecystitis a. Antibiotics b. Pain Management V. Vaccines for Liver Diseases a. Hepatitis A vaccine b. Hepatits A Immune Globulin c. Hepatitis B vaccine d. Hepatitis B Immune Globulin VI. Recommendations for Post-exposure prophylaxis for contact with patients positive for HbsAg VII. Drugs for Chronic Active Hepatitis VIII. Treatment for Hepatitis C Infection IX. Self-test Methyl salicylate, the major constituent of the essental oil of wintergreen DRUGS FOR REDUCING BILIRUBIN LEVELS Jaundice, or icterus : results from the deposition of bilirubin. (hyperbilirubinemia) Phenobarbital Efficacy • An anticonvulsant • Used to reduce serum bilirubin levels by at least 25% • MOA: Increases conjugation and excretion of bilirubin. Contraindications • documented hypersensitivity • severe respiratory disease • marked impairment of liver function • patients with nephritis Drug interactions: • decreases effects of Chloramphenicol, Digitoxin, corticosteroids, carbamazepine, theophylline, verapamil, metronidazole, anticoagulants • coadministration with alcohol may produce additive CNS effects and death • toxicity may be increased by chloramphenicol, valproic acid and monoamine oxidase inhibitors (MAOIs) • Rifampicin may decrease effects • induction of microsomal enzymes may result in decreased effects of oral contraceptives in women Hyperbilirubinemia may result from: 1. overproduction of bilirubin 2. impaired uptake, conjugation, or excretion of bilirubin; or 3. regurgitation of unconjugated or conjugated bilirubin from damaged hepatocytes or bile ducts. Clofibrate • Reduces serum bilirubin levels • MOA: unknown. • Lowers serum triglycerides and very low-density lipoprotein (VLDL) levels JAUNDICE Differential diagnosis for the yellowing of the skin: 1. jaundice 2. carotenoderma 3. the use of the drug quinacrine, and 4. excessive exposure to phenols. Examples of Phenolic compounds • Phenol, the parent compound, used as a disinfectant • Salicylic acid • Cannabinoids, the active constituents of cannabis • Capsaicin, the pungent compound of chilli peppers • Tyrosine, an amino acid. • The neurotransmitters serotonin, dopamine, adrenaline, and noradrenaline. • L-DOPA, a drug for Parkinson's disease. • Chavibetol from betel • Estradiol and other estrogens • Diethylstilbestrol • The pH indicator phenolphthalein • Thymol, an antiseptic that is used in mouthwashes CAUSES OF ISOLATED HYPERBILIRUBINEMIA Causes of Isolated Hyperbilirubinemia I. Indirect hyperbilirubinemia A. Hemolytic disorders 1. Inherited Spherocytosis, elliptocytosis G-6-PD and pyruvate kinase deficiencies Sickle cell anemia 2. Acquired Microangiopathic hemolytic anemias Paroxysmal nocturnal hemoglobinuria Immune hemolysis B. Ineffective erythropoiesis Cobalamin, folate, & iron deficiencies C. Drugs Rifampicin, probenecid, ribavirin D. Inherited conditions Crigler-Najjar types I and II Gilbert's syndrome Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 1 of 8 II. Direct hyperbilirubinemia Inherited conditions Dubin-Johnson syndrome Rotor's syndrome 2. 3. 4. G-6-PD DEFICIENCY To decrease likelihood of hemolysis, AVOID: • Antimalarials: Primaquine, Chloroquine, Dapsone (antileprosy drug), Pamaquine, Pentaquine • Antimicrobials urinary antiseptic (nitrofurantoin) quinolones (nalidixic acid, ciprofloxacin, norfloxacin) chloramphenicol antiparasitic (antischistosomal niridazole) sulfonamides anti-TB (isoniazid) • Antimethemoglobinemic dye (methylene blue) • Urinary analgesic (phenazopyridine) • Vitamin K analogs • Certain chemicals such as those in mothballs (naphthalene) • Analgesic (acetanilid) • Antineoplastic antibiotic (doxorubicin) • Isobutyl nitrite • Ineffective erythropoiesis occurs in cobalamin, folate, and iron deficiencies 5. 6. 7. ** These are at increased risk due to depletion of glutathione stores. 8. 9. FOR JAUNDICE in patients with chronic hemolysis, high incidence of pigmented (calcium bilirubinate) gallstones increases the likelihood of choleducholithiasis as an alternative explanation for hyperbilirubinemia. DRUG-INDUCED HEPATOCELLULAR INJURY Classification of Drug-induced hepatocellular injury: 1. Predictable : dose-dependent & affects all patients who ingest a toxic dose of the drug in question. Classic example: paracetamol hepatotoxicity 2. Unpredictable or idiosyncratic : not dose-dependent & occur in minority Isoniazid hepatotoxicity (not very common) Environmental toxins - important cause of hepatocellular injury • industrial chemicals vinyl chloride • herbal preparations containing… pyrrolizidine alkaloids (Jamaica bush tea) the mushrooms Amanita phalloides or verna (contain hepatotoxic amatoxins) Risk factors for drug-induced liver injury 1. Race • blacks & Hispanics more susceptible to isoniazid (INH) toxicity rate of metabolism under the control of P-450 enzymes Age • Elderly persons are at increased risk Sex • More common in women for unknown reasons Alcohol Ingestion • induces liver injury & cirrhotic changes • causes depletion of glutathione (hepatoprotective) stores that make the person more susceptible to toxicity by drugs Liver Disease Genetic Factors • Genetic factors affecting P450 enzymes Other comorbidities • AIDS • Malnutrition • Fasting Drug Formulation • Long-acting drugs may cause more injuries Host factors that may enhance susceptibility to drugs, possibly inducing liver disease • Female: Halothane, nitrofurantoin, sulindac • Male: Amoxicillin-clavulanic acid (Augmentin) • Old age: paracetamol, halothane, INH, co-amoxiclav • Young age: valproic acid, salicylates (We don’t give Aspilet, a salicylate, to children now since they are very prone to Reye’s Syndrome; which can also make children more prone to viral infection like chicken pox and croup) • Fasting or malnutrition: paracetamol • Large body mass index/obesity: halothane (binding to fat cells) • Diabetes mellitus: methotrexate, niacin • Renal failure: tetracycline, allopurinol • AIDS: dapsone, cotrimoxazole (used for treating Pneumocystis carinii) • Hepatitis C: ibuprofen, ritonavir, flutamide • Pre-existing liver disease: niacin, tetracycline, methotrexate Signature Effects of Drugs on the Liver • Paracetamol (Acetaminophen): hepatotoxicity due to the toxic metabolite N-acetyl-p-benzoquinone (NAPQI) causing centrilobular necrosis • Amoxicillin: moderate rise in SGOT or SGPT levels, or both • Amiodarone: abnormal liver function test results in 15-50% of patients • Chlorpromazine: resembles that of infectious hepatitis with laboratory features of obstructive jaundice • Quinolones; cholestatic jaundice with repeated use • Diclofenac: induced liver injury with elderly female more susceptible; elevation of one or more liver tests • Erythromycin: may cause hepatic dysfunction; increased liver enzyme levels and hepatocellular and/or cholestatic hepatitis • Fluconazole: mild transient elevations in transaminase levels to hepatitis, cholestasis, and fulminant hepatic failure • Isoniazid: severe and fatal hepatitis Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 2 of 8 • • • • • • • Methyldopa: contraindicated in patients with active liver disease Oral contraceptives: can lead to intrahepatic cholestasis without portal inflammation and vascular lesions; with pruritus and jaundice Statins: biochemical abnormalities of liver function like moderate elevations of serum transaminase levels Rifampicin: mild hepatitis, usually a general hypersensitivity reaction Valproic acid and Divalproex sodium: microvesicular steatosis Cocaine: abuse associated with acute elevation of hepatic enzymes with necrosis and microvascular changes. Ecstasy: an amphetamine used as a stimulant which may cause hepatitis and cirrhosis. Inducers of the Hepatic P-450 enzymes: • Phenobarbital • Phenytoin • Carbamazepine • Primidone • Ethanol • Glucocorticoids • Rifampin • Griseofulvin • Quinine • Omeprazole - Induces CYP 1A2 Inhibitors of the Hepatic P-450 Enzymes • Amiodarone • Cimetidine • Erythromycin • Grape fruit • Isoniazid • Ketoconazole • Metronidazole • Sulfonamides • Quinidine • Omeprazole - Inhibits CYP2C8 ACUTE CHOLECYSTITIS Initial empiric anti-microbial therapy: • Must be comprehensive • Should cover both aerobic and anaerobic gram-negative organisms • Most commonly indicated for Cholangitis and Cholecystits Initial Treatment of Acute Cholecystitis • bowel rest • intravenous hydration • analgesia • intravenous antibiotics • For mild cases: antibiotic therapy with a single broadspectrum antibiotic is adequate Acute Cholecystitis • Current antibiotic recommendations include: ampicillin, ampicillin/sulbactam, or piperacillin/tazobactam • For severe cases of acute cholecystitis: gentamicin with clindamycin or metronidazole with a third-generation cephalosporin • Bacteria that are commonly associated with cholecystitis include: E coli Bacteroides fragilis Klebsiella Enterococcus Pseudomonas species. ANTIBIOTICS FOR CHOLECYSTITIS Ampicillin and Sulbactam (Unasyn) • Drug combination of beta-lactamase inhibitor with ampicillin • Covers epidermal and enteric flora and anaerobes. • Not ideal for nosocomial pathogens Ampicillin • Bactericidal activity against susceptible organisms (against G(+), G(-) (improved activity) and non-β-lactamase producing anaerobes) • Effective for shigellosis • Not active against agents of nosocomial infections (Klebsiella, Enterobacter, Pseudomonas, Citrobacter, Serratia, indole (+) Proteus and G(-) aerobes • MOA: inhibit bacterial growth by interfering with the transpeptidation reaction of cell wall synthesis • Kinetics: good distribution in gall bladder Acid-stable; well absorbed after oral administration Intake of food prior to ingestion diminishes absorption T ½: 80 minutes Ampicillin appears in the bile, undergoes enterohepatic circulation, and is excreted in appreciable quantities in the feces • Important ADR: hypersensitivity • Drug Interactions: Probenecid and disulfiram elevate levels Allopurinol decreases effects and has additive effects on ampicillin rash may decrease effects of oral contraceptives Piperacillin and Tazobactam • Antipseudomonal penicillin plus beta-lactamase inhibitor. • MOA: Inhibits biosynthesis of cell wall mucopeptide and is effective during stage of active multiplication Piperacillin • has anti-pseudomonal activity • Excellent antimicrobial activity against Pseudomonas, Klebsiella, and certain other G(-) microorganisms; retains Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 3 of 8 • • • • the activity of ampicillin against G(+) cocci and L. monocytogenes In combination with a β-lactamase inhibitor (piperacillintazobactam, ZOSYN) it has the broadest antibacterial spectrum of the penicillin Kinetics: good distribution in gall bladder; high biliary concentrations are achieved Important ADR: hypersensitivity Drug Interactions: Tetracyclines may decrease effects Coadministration with aminoglycosides has synergistic effects (however, high concentrations may physically inactivate aminoglycosides) probenecid may increase levels Clindamycin • a lincosamide • for treatment of serious skin and soft tissue staphylococcal infections • also effective against aerobic and anaerobic streptococci (except enterococci) • MOA: Inhibits bacterial growth, possibly by blocking dissociation of peptidyl tRNA from ribosomes, causing RNA-dependent protein synthesis to arrest. • adjust dose in severe hepatic dysfunction • associated with severe and possibly fatal colitis by allowing overgrowth of C difficile Ceftazidime (Fortum) • Third-generation cephalosporin with broad-spectrum, gram-negative activity • lower efficacy against gram-positive organisms • higher efficacy against resistant organisms. • MOA: arrests bacterial growth by binding to one or more penicillin-binding proteins • Kinetics: distributed in most tissues including the gall bladder • Important ADR: hypersensitivity • Drug Interactions: nephrotoxicity may increase with concomitant use of aminoglycosides, furosemide, & ethacrynic acid probenecid may increase levels • • Levofloxacin For pseudomonal infections and infections due to multidrug-resistant gram-negative organisms. Contraindicated in pediatric age group (18 years and below) Gentamicin • Aminoglycoside antibiotic for gram-negative coverage. • Used in combination with both an agent against grampositive organisms and one that covers anaerobes. • Kinetics: poorly absorbed • Drug Interactions: Coadministration with other aminoglycosides, cephalosporins, penicillins, and amphotericin B may increase nephrotoxicity aminoglycosides enhance effects of neuromuscular blocking agents - prolonged respiratory depression may occur coadministration with loop diuretics may increase auditory toxicity of aminoglycosides possible irreversible hearing loss of varying degrees may occur (monitor regularly) Imipenem and Cilastatin (Tienem) • For treatment of multiple organism infections in which other agents do not have wide spectrum coverage or are contraindicated because of potential for toxicity. PAIN MANAGEMENT FOR CHOLECYSTITIS Metronidazole • imidazole ring-based antibiotic active against various anaerobic bacteria and protozoa • often used in combination with other antimicrobial agents (except Clostridium difficile enterocolitis) Ciprofloxacin • Fluoroquinolone with activity against Pseudomonas species, streptococci, MRSA, Staphylococcus epidermidis, and most gram-negative organisms • No activity against anaerobes. • MOA: Inhibits bacterial DNA synthesis through inhibition of DNA gyrase enzyme. • Important ADR: hypersensitivity Contraindicated in pediatric age group (18 years and below) Drug Interactions: Antacids, iron salts, and zinc salts may reduce serum levels Cimetidine may interfere with metabolism of fluoroquinolones Reduces therapeutic effects of phenytoin Probenecid may increase ciprofloxacin serum concentrations May increase toxicity of theophylline, caffeine, cyclosporine, and digoxin (monitor digoxin levels) May increase effects of anticoagulants (monitor PT) • • • • Pain is a prominent feature of cholecystitis Classic teaching: Morphine is NOT the agent of choice because of the possibility of increasing tone at the sphincter of Oddi Meperidine – provides adequate analgesia without affecting the sphincter of Oddi and DOC for cholecystitis pain relief Meperidine (Demerol) • Agonist activity at opioid receptors • analgesic with multiple actions similar to those of morphine. • Exerts its chief pharmacological action on the CNS and the neural elements in the bowel • Kinetics Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 4 of 8 • • • • Greater ability to enter the CNS, thereby producing analgesia at lower systemic concentrations Metabolized chiefly in the liver, t ½ of about 3 hours. Significant antimuscarinic effects, may be a contrainidication if tachycardia would be a problem Negative inotropic action on the heart produce less constipation, smooth muscle spasm, and depression of cough reflex than similar analgesic doses of morphine Other ADR: Upper airway obstruction or significant respiratory depression. Accumulation of its metabolite, normeperidine excitatory symptoms (hallucinations, tremors, muscle twitches, dilated pupils, hyperactive reflexes, convulsions, seizures) • • • Pancreatic enzyme supplements • For treatment of pancreatic enzyme insufficiency which causes steatorrhea, azotorrhea, vitamin malabsorption and weight loss • 2 major preparations: pancreatin (no longer common) and pancrelipase • Pancrelipase: enriched preparation of amylase, lipase and protease Available in enteric-coated and non-enteric coated preparations (should be given with acid suppression therapy) Dosing individualized to age and weight • Well-tolerated • Excessive doses: abdominal pain and diarrhea; hyperuricosuria and renal stones CHOLELITHIASIS Cholelithiasis o The most widely used oral bile salt compound is ursodeoxycholate, which is effective only for small, pure cholesterol stones located in a functioning gallbladder. o Despite maintenance therapy, recurrence rates are high, averaging 50-60% in most published series. CHOLESTASIS • • Also effective for prevention of gall stones in obese patients undergoing rapid weight loss therapy Dosage: 10 mg/kg/d for 12-24 months dissolution occurs in up to half of patients with small (<5-10mm) noncalcified gall stones Contraindication: documented hypersensitivity calcified cholesterol stones radiopaque stones bile pigment stones Practically free of serious adverse effects. Bile-salt induced diarrhea is uncommon. Not associated with hepatotoxicity. Patients with steatorrhea may benefit from: pancreatic enzyme supplements and fat-soluble vitamins A, D, E, and K Gallstone dissolution agents – Ursodeoxycholic acid - a naturally occurring bile acid used in the dissolution of gallstones, microlithiasis, and in primary biliary cirrhosis. Ursodiol • Naturally occurring bile acid • MOA: decreases cholesterol content of bile and bile stones probably by reducing secretion of cholesterol from the liver and the amount reabsorbed by intestines. Also appears to stabilize hepatocyte canalicular membranes, possibly through a reduction in the concentration of other endogenous bile acids or through the inhibition of immunemediated hepatocyte destruction. • Kinetics After oral administration, it is absorbed, conjugated in the liver with glycine or taurine and excreted in the bile. Conjugated ursodiol undergoes extensive enterohepatic recirculation t ½: 100 hours Unabsorbed or unconjugated ursodiol colon where it is either excreted or dehydroxylated by bacteria to lithocolic acid (potentially hepatotoxic) • Indication dissolution of small cholesterol gall stones with symptomatic gall bladder disease who refuse cholecystectomy or who are poor surgical candidates. Drug-induced Intrahepatic Cholestasis • usually reversible • Associated with: - anabolic & contraceptive steroids - most common - chlorpromazine, imipramine, tolbutamide, sulindac, cimetidine - antibiotics as: erythromycin estolate, co-trimoxazole, & penicillins (such as ampicillin, dicloxacillin, & clavulanic acid) • Chronic cholestasis has been associated with: - chlorpromazine - prochlorperazine VACCINES FOR LIVER DISEASES Vaccines are used for active immunization while immune globulins are for passive immunization. Hepatitis A Vaccine • Inactivated vaccine • Used for active immunization against disease caused by HAV. • Route: Intra-muscular • May be administered with immunoglobulin injections without affecting its efficacy • Efficacy: used for active immunization (efficacy >85%) 1˚ immunization: One dose (administered 2-4 weeks before travel to endemic areas) Booster: At 6-12 months for long-term immunity Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 5 of 8 - • • Indications: Travelers to HepA endemic areas; homosexual and bisexual men; illicit drug users; chronic liver disease or clotting factor disorders; persons with occupation risk for infection; persons living in, or relocating to endemic areas; and household and sexual contacts of individuals with acute HepA Precautions: Caution in individuals taking anticoagulant therapy Drug Interactions: May decrease effects of immunosuppressive agents Hepatitis B Immune Globulin (HBIG) • For post-exposure prophylaxis in nonimmune persons following percutaneous, mucosal, sexual or perinatal exposure • Efficacy derived from plasma passive immunization for individuals who describe recent exposure to a patient infected with HBV • Hepatitis B vaccine should also be administered RECOMMENDATIONS FOR POST-EXPOSURE PROPHYLAXIS FOR CONTACTS WITH PATIENTS POSITIVE FOR HbsAg Immune globulins • Purified preparation of gamma globulin. • Derived from large pools of human plasma and is composed of 4 subclasses of antibodies, approximating the distribution of human serum. • Used for postexposure prophylaxis or when inadequate time is available for immunization to be effective before potential exposure • Efficacy: Effective when administered within 14 days of exposure 1. 2. 3. 4. 5. Hepatitis A Immune Globulin(HAIG) • Mechanisms of Action neutralizes circulating myelin antibodies through antiidiotypic antibodies down-regulates proinflammatory cytokines, including INF-gamma blocks Fc receptors on macrophages may increase CSF IgG (10%). 6. 7. Perinatal exposure - HBIG plus vaccination at time of birth (90% effective) Sexual contact with an acutely infected patient - HBIG plus vaccination Sexual contact with a chronic carrier - Vaccination Household contact with an acutely infected patient - None Household contact with an acutely infected person resulting in known exposure – HBIG with or without vaccination Infant ( <12 mo) primarily cared for by an acutely infected patient - HBIG with or without vaccination Inadvertent percutaneous or permucosal exposure - HBIG with or without vaccination DRUGS FOR CHRONIC ACTIVE HEPATITIS • Hepatitis B Vaccine • Inactivated viral antigen, recombinant • Intramuscular route (subcutaneous if with bleeding disorders) 1˚ immunization: 3 doses (0, 1 and 6 months) Booster: Not routinely recommended • Efficacy consists of recombinant HBsAg produced in yeast low response rates have been associated with obesity, smoking, immunosuppression, and advanced age approximately 25-50% of persons who initially do not respond to the vaccine will respond to one additional vaccine dose, and 50-75% of persons will respond to a second 3-dose series • Safety HBV vaccine seems to be safe, although some questions exist regarding neurological complications For infants born to mothers with active HBV infection, a passive-active (immunoglobulin and vaccination) approach is recommended Indications: All infants; Preadolescents, adolescents and young adults; persons with occupational, lifestyle or environmental risk; hemophiliacs; hemodialysis patients; and postexposure prophylaxis • Therapy is currently recommended for patients with evidence of chronic active disease (ie, high levels of the aminotransferases, positive HBV DNA findings, HBeAg). Currently, interferon alfa (IFN-a), lamivudine, and adefovir dipivoxil are the main drugs approved globally. Interferon alfa • Protein product manufactured by recombinant DNA technology. • Efficacy Published reports show that after IFN-a treatment for 4 months, the HBV DNA levels and HBeAg become undetectable in 30-40% of patients. dose: with 5 million U/d or 10 million units 3 times per week subcutaneously MOA: not understood modulation of host immune responses enhances cytolytic T-cell activity stimulates natural killer cell activity and amplifies HLA class I protein on infected cells. • High levels of aminotransferases, a low viral load, and infection with the wild type are good prognostic factors for response to IFN-a treatment. • Special attention for patients with HBV-decompensated cirrhosis (eg, ascites, encephalopathy) who are taking IFNα because they either respond or can deteriorate further. • Elimination: mainly renal; liver metabolism and biliary excretion are minor pathways • ADRs: can be severe, even devastating: Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 6 of 8 - - Transient hepatic enzyme elevations may occur in the first 8-12 weeks flulike syndrome myelosuppression (eg, leukopenia, thrombocytopenia) nausea, diarrhea, fatigue irritability, depression, thyroid dysfunction, alopecia Contraindications: hepatic decompensation, autoimmune disease and hx of cardiac arrhythmia Abortifacient Do not give to pregnant patients! Drug interaction: increased theophylline and methadone levels; Combination with NRTI agents hepatic failure; Co-administration with zidovudine exacerbate cytopenia Lamivudine • A thymidine nucleoside analogue • Prolonged intracellular half-life on HBV cell lines lower dose and less frequent administration • Safely administered to patients with hepatic decompensation • MOA: inhibits the viral polymerase; inhibits HBV DNA polymerase and HIV reverse transcriptase by competing with dCTP for incorporation into the viral DNA resulting in chain termination • Efficacy: associated with a 4-log reduction of the viral load appears to be effective for patients who do not respond to IFN-α treatment Suppression of HBV DNA to undetectable levels in 44% of patients Seroconversion of HBeAg from positive to negative in 17% of patients shown to dramatically improve the condition of patients with decompensated disease due to HBV reactivation. Major complication: the emergence of viral variants Safety: At therapeutic doses, excellent safety profile Adefovir dipivoxil • a nucleoside analogue • Diester prodrug of adefovir (acyclic phosphonated adenine nucleotide analog) • MOA: phosphorylated by cellular kinases to active disphosphate metabolite and then competitively inhibits HBV DNA polymerase chain termination (a potent inhibitor of the viral polymerase) • Kinetics Oral BA: 59%, unaffected by meals; t ½ : 7.5 hrs Renal elimination may be given to patients with decompensated liver disease • Efficacy has been tested in HbeAg-positive, HbeAg-negative, and lamivudine-resistant patients with encouraging results. 3.5 logs reduction of HBV DNA - • • • Normalization of aspartate aminotransferase in 4872% Improvement in liver histology and fibrosis in 53-64% of patients at 48 wks Prolonged therapy higher response rates Optimal dose seems to be 10 mg/d. Higher doses are nephrotoxic. Safety: well-tolerated; may cause dose-dependent nephrotoxicity Other ADRs: headache, diarrhea, asthenia, abdominal pain Entecavir • Oral guanosine nucleoside analog • Competitively inhibits all 3 functions of DNA polymerase: base priming, reverse transcription and synthesis of positive strand • Oral BA approaches 100% but decreased by food • T ½: 15 hours; renal elimination • Efficacy compared to lamivudine Similar rates of HBeAg seroconversion Higher rates of viral DNA suppression, normalization of aspartate aminotransferase and improvement in liver histology • No primary resistance after 48 weeks of use • Safety: Well tolerated. Common ADRs: headache, fatigue, dizziness and nausea TREATMENT OF HEPATITIS C INFECTION • • Primary goal: viral eradication Current standard of treatment: once-weekly pegylated interferon alfa and daily oral ribavirin Ribavirin • Guanosine analog • Phosphorylated intracellularly by host cell enzymes • MOA: appears to interfere with synthesis of guanosine triphosphate inhibit capping of viral mRNA; inhibit viral RNA-dependent polymerase • Oral BA: 64%, increases with high fat meals and decreases with antacids • Elimination through urine • Improved response if in combination with interferon alfa but should be balanced with increased risk for toxicity • ADR: dose-dependent hemolytic anemia (10-20%), depression, fatigue, irritability, rash, cough, insomnia, nausea and pruritus • Tetatogenic and embryotoxic in animals, as well as mutagenic in mammals • Contraindications: uncorrected anemia, end-stage renal disease, ischemic vascular disease and pregnancy Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 7 of 8 SELF-TEST 1. A type of phenolic compounds used as pungent compounds of chili peppers a. Cannabinoids b. Capsaicin c. Chavibetol d. Phenol 2. An anticonvulsant that is used for the treatment of jaundice by increasing conjugation and excretion of bilirubin a. Carbamezepine b. Phenytoin c. Phenobarbital d. All of the above 3. Co administration of this substance together with you answer on number 2 will produce additive CNS effects and death. a. Theophylline b. Alcohols c. Verapamil d. Carbamezepine 4. Drugs to be avoided with G6-PD deficiency patients a. Primaquine b. Pamaquine c. Quinolones d. Only A and B e. All of the above 5. TRUE of the risk factors for drug-induced liver injury, except. a. Black and Hispanics are more susceptible to isoniazid toxicity b. More common in women c. Male patient taking Augmentin d. Female patient taking nitrofurantoin e. None of the above 6. Correct pair on signature effects of drugs in the liver, EXCEPT a. Amoxicillin – moderate rise in SGOT or SGPT levels b. Quinolones – cholestatic jaundice reported with repeated use c. Diclofenac – elevation of one or more liver test results d. Oral contraceptives - can lead to intrahepatic cholestasis e. None of the above 7. Drug that both induces CYP 1A2 and inhibits CYP2C8 a. Quinidine b. Sulfonamide c. Omeprazole d. Cimetidine 8. Initial treatment for acute cholecystitis a. Single broad spectrum antibiotic b. Narrow spectrum antibiotic c. Intermediate spectrum antibiotic d. A and C 9. TRUE on treating pain from cholecystitis, EXCEPT a. Meperidine provides analgesia b. Morphine provides analgesia c. Morphine increases the tone of sphincter of Oddi d. Meperidine has no effect on the tone of sphincter of Oddi 10. Recommendations for postexposure prophylaxis for contacts of patients positive for HBsAg, EXCEPT a. Perinatal exposure b. Sexual contact with an acutely infected patient c. Sexual contact with a chronic carrier d. Household contact with an acutely infected patient e. None of the above Answers: 1.B 2.C 3. B 4.E 5.E 6.E 7.C 8.A 9.B 10.D Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 8 of 8







