Prevention of subatmospheric DCI
advertisement
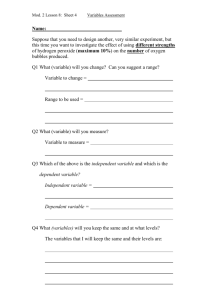
DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 Subatmospheric decompression sickness —DCI INTRODUCTION = Group of effects produced by exposure to altitude that are not due to expansion of trapped or enclosed gas. The main manifestations are: o Bends: limb pain o Chokes: respiratory disturbances o Creeps: skin irritations o Staggers: various CNS disturbances o Syncope: cardiovascular collapse. These symptoms virtually always subside or disappear during descent to ground level. However, recovery may not occur after recompression and the severity of symptoms may increase, leading to post-descent collapse. CAUSE OF DCI Basic mechanism = supersaturation of the tissues with nitrogen N2. o The body contains ≈ 1000 ml STPD N2. o ➪Pre-oxygenation with 100% O2 before exposure to altitude will wash out N2. o As PiN2 with ascent to altitude, ➪N2 is carried by the blood to the lungs, where it leaves the body in the expired gas. o N2 has a low solubility in blood ➪tissues become supersaturated with N2. ➪Possible formation of bubbles of gas. Supersaturation ratio = (Tension of inert gas in tissue) / (ambient pressure) Bubbles grow in size by diffusion Bubbles may be carried by the circulation to another organ ➪Venous Gas Embolism VGE, which can be detected by echocardiodoppler. o Grade 0 Bubble signal absent o Grade 1 Occasional bubbles discernible o Grade 2 < ½ of cardiac cycles contain bubbles o Grade 3 Most of cardiac cycles contain bubbles o Grade 4 Continuous bubble signals throughout cardiac cycle. No correlation between the presence of bubble and the occurrence of symptoms. Bubbles will not form in the blood unless suitable nuclei are present. They have to grow to a critical size. ➪The rate of production of DCI is very low immediately after ascent. The peak is at 20-60 minutes The driving pressure for bubble formation in a fluid is the difference between the partial pressure of the gas dissolved in the fluid and the absolute hydrostatic pressure. PRESENTATION OF DCI DCI may arise: o In flight o During exposure to reduced Patm in an hypobaric chamber. Altitude threshold @ 18000 ft o Low incidence between 18-25000 ft. o Physical activity contributes to the development of bubbles and symptoms. ©Jean-Michel Ferrieux-2011 1 DAvMed 44 Decompression sickness — 7/129 & 50/757 Clinical manifestations KCL 2011 Joint and limb pains Bends. o Most common symptom o Pain usually ill-localized and deep-seated o ≥ 1 site can be involved. o Knees o Shoulders o Elbows o Wrists & hands o Ankles & feet A mild pain often encourages the individual to move or rub the aching part, which will tend to increase the pain. Application of local pressure (e.g. with a bandage) will tend to relieve the pain. Almost always disappear during descent (recompression) May be present without in the absence of radiological changes. VGE can be detected in ≈ ⅓ of symptom-free individuals, and in almost all people with symptoms. Skin disturbances Creeps o Itching (démangeaisons) o Tingling (picotements) o Formication (fourmillements) o Usually transient o The itching may rarely be severe with hyperaesthesia o Commonly accompanied by chest bluish-red patches: cutis marmorata Respiratory disturbances Chokes o = Serious manifestation of DCI o Sense of lower chest constriction, often with tight feeling in epigastrium Increased with deep breath (inspiratory snatch). o General feeling of malaise o Cough @ any attempt to take a deep breath If exposure to altitude is maintained ➪the chokes will progress to collapse. The symptoms may persist several hours after descent and may be precipitated by tobacco smoke of deep aspiration. Part of the reflex response to irritation of the pulmonary tissues caused by the occlusion of pulmonary arterioles and capillaries by gas bubbles. Neurological disturbances Staggers (tournis - vertige) o Rare in aviation DCI o Paralysis, paraesthesia, anaesthesia and convulsions may be present in a wide variety of clinical pictures. ©Jean-Michel Ferrieux-2011 2 DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 Visual disturbances Blurring of vision Scotomata Fortification patterns Hemianopsia Often associated with other symptoms such as headache and could be mistaken for migraine. Collapse General feeling of malaise, anxiety and diminished consciousness. o Pallor o Restlessness o Cold and sweaty hands and face o Vomiting and headache are commonly seen. Descent is usually followed by a rapid recovery. Post-decompression collapse Very rare complication The symptoms may persist after return to ground level, and become worse. Occurs in ≈ 1/2500 unprotected exposures above 30000 ft . Almost never occurs in an exposure to altitude where symptoms have been present. There may be a "free interval" of several hours between return to ground level and appearance of symptoms. o The patient becomes anxious, with a frontal headache and feels sick o Facial pallor and cold sweaty extremities o Nearly always cyanosis with raised Ht up to 55-65% o General and focal signs of neurological involvement o Coma. Very rare recovery @ that stage. INCIDENCE OF DCI General factors Altitude threshold ≈ 18000 ft. Exercise @ altitude: @ rest @ exercise Occurs in 10% 35000 ft 30000 ft Occurs in 20% 37500 ft 33000 ft Increased risk if diving > 10m (2 atm.) within 12 hours before exposure to altitude ➚ rate of ascent ➪➚ risk of DCI DCI does not appear immediately on exposure to altitude: peak @ 20-60 minutes exposure. Repeated exposures may increase the risk Cold T° and hypoxia may increase susceptibility to DCI (and severity if hypoxia). Personal factors Individual susceptibility ➚ susceptibility with ➚ age (++ if > 42 years old) ➚ BMI ➪➚ risk. However, previously obese individuals do not show a decrease in risk of DCI. No sex ratio After-effects of alcohol Intercurrent infection or disease ©Jean-Michel Ferrieux-2011 3 DAvMed 44 Decompression sickness — 7/129 & 50/757 Patent Foramen Ovale PFO. KCL 2011 CLASSIFICATION OF DCI Golding classification: o Type 1: Bends & creeps o Type 2: Staggers, chokes & cardiovascular manifestations RAF classification: o Primary o Secondary. PREVENTION OF SUBATMOSPHERIC DCI Limiting the reduction of environmental pressure o Maximum cabin altitude 22000 ft (fast-jet) Limiting the duration of exposure to low pressure Washing out N2 from tissues and body fluids, prior to exposure o Pre-oxygenation (= denitrogenation), ideally ≥ 1 hour: o A 30-minute pre-ox will ensure no DCI during a short-duration exposure to 48000 ft, if the total time above 25000 ft is ≤ 10 minutes. Staged decompression for preparation of astronauts for an EVA (Extra-Vehicular Activity). ©Jean-Michel Ferrieux-2011 4 DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 Clinical management of DCI INTRODUCTION EVOLVED GAS DISEASE Humans are capable of tolerating a certain amount of bubble load. Venous bubbles are filtered from the circulation by the lung. Lung capacity to filter bubbles is finite. A right-to-left shunt may allow bubbles to bypass the pulmonary filter. o ≈ 25% of general population have a PFO ARTERIAL GAS EMBOLISM (AGE) 2d method of bubble generation results of expansion of trapped gas (Boyle's law): o Subcutaneous emphysema o Pneumomediastinum o Gas may also enter the pulmonary veins and be carried to the left heart, causing an AGE. 2 target organs for an AGE: o Brain o Heart EBULLISM Exposure to 63000 ft: o Pamb = 47 mmHg ≡ saturated water vapour pressure @ 37°C o ➪Spontaneous boiling and degassing of body fluids and tissues Involvement of the cardiovascular system commences with bubble formation in the low-pressure areas of the circulation (ie) venous & capillary beds. o Massive pulmonary damage (haemorrhage and atelectasis) in post-mortems. Successful short-term exposures to altitudes > 63000 ft possible using partial-pressure assemblies that increase intrapulmonary pressure and provide counter-pressure to certain areas of the body. DIAGNOSIS OF DCI No highly sensitive or specific diagnostic investigations for DCI. Key facts that must be established: o Nature of the symptoms o Evolution and severity o Timing of onset, relative to exposure to altitude o Maximum altitude experienced o Rate of altitude exposure o Response of symptoms to O2 o Response of symptoms to descent Rapid onset of symptoms is suggestive of AGE, ++ if rapid decompression Delayed symptoms are more suggestive of evolved gas disease. PRESENTATION OF DCI Type 1 - mild DCI Type 2 - serious DCI ©Jean-Michel Ferrieux-2011 5 DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 Evolution Describes the development of symptoms before descent or recompression. DCI is a dynamic condition: o Initially progressive o Then static o And may be spontaneously improving o May also relapse. Manifestations Pain Bends. cf. above Deep aching pain May migrate from joint to joint (niggles) May worsen Often no objective signs on examination Girdle or back pain Neurological Staggers cf. above May range from the subtle, multifocal presentations of mild evolved gas disease to the catastrophic presentation of severe cerebral AGE. Both CNS and PNS may be involved o Alterations of higher functions o Altered level of consciousness o Seizure activity o Impaired coordination o Dysfunction of special senses o Loss of sphincter control… Cardiopulmonary 2 distinct processes of lung involvement: o Decompression pulmonary barotrauma o Cardiopulmonary consequences of massive venous gas embolism Cardiac involvement: o Coronary artery AGE Shared symptoms: o Dyspnoea & Tachypnoea o Chest pain o Cough o Haemoptysis o Cyanosis o (Shock). Cutaneous Creeps cf. above Cutaneous manifestations often occur at altitude Usually transient o Itching ± cutis marmorata o Tingling o Formication ©Jean-Michel Ferrieux-2011 6 DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 Constitutional Non-specific symptoms: o Headache o Malaise o Fatigue o Nausea o Anorexia o Anxiety. Rapid recovery often follows descent. DIFFERENTIAL DIAGNOSIS Intercurrent illness Rare in the well-screened aircrew population o Limb pain o Viral illnesses o CAD o Cerebrovascular disease Environmental flight stresses Hypoxia o Rapidly reversed by the administration of an increased PO2. o Will also respond to descent. GI gas distension o Can cause stretching of the visceral walls o Significant abdominal pain is uncommon @ altitudes below 40000 ft. +Gz related atelectasis o Resemblance to cardiopulmonary DCI. Alternobaric vertigo o Is likely to occur @ lower altitudes, where the pressure changes are greater, and generally below the threshold for DCI. Hyperventilation o Not uncommon in conjunction with altitude exposure. o Usually easy to recognise by the rate and depth of respoiration. MANAGEMENT OF DCI First aid FiO2 100% Minimize activity Lie the patient flat or in recovery position, if severe symptoms or impaired consciousness. Increase ambient pressure and/or descent to ground level as soon as possible. In flight, a PAN call should be made, declaring a physiological emergency. The vast majority of cases will have resolved completely on return to ground level. Management on the ground Initial treatment in order to stabilize the patient along conventional trauma management guidelines. All patients should be rehydrated at the earliest opportunity: ©Jean-Michel Ferrieux-2011 7 DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 o Oral fluids if conscious o IV crystalloid solutions if altered consciousness. Consider hyperbaric recompression if symptoms have not subsided. Take advice from a diving medicine specialist. Role of hyperbaric recompression Recompression remains the definitive treatment for dysbaric disorders. Will reduce the volume of any remaining gas bubbles in the tissues. Bubble size reduction is not linear, but asymptotic and will also depend on bubble shape. Hyperbaric O2: o Enhances the wash-out of N2 from any remaining bubbles, o Increases the blood O2 content and, hence, the delivery, o Reduces endothelial dysfunction, o Lessens the consequences of reperfusion injury. Recompression schedules Royal Navy treatment table 61 Royal Navy treatment table 62 Royal Navy treatment table 66 Specifically developed for the treatment of patients requiring hyperbaric oxygen therapy. ©Jean-Michel Ferrieux-2011 8 DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 Adjunctive measures Recommended in order to optimize the patient's condition before transfer to more distant recompression facilities. Fluids o Compromised microcirculation in DCI. Endothelial damage Platelet thrombi formation. o Fluids containing 60mM Na and 80-120mM glucose have been used successfully. o Oral intake of 1-2 litres per hour is safe and tolerable (if conscious). o If significant symptoms are present, IV fluids are preferred: Oral intake interrupts 100% O2 breathing Need to sit up to swallow for most people Increased risk of vomiting Isotonic IV fluids are preferred. Accurate fluid-balance recording is essential. Lidocaine o @ therapeutic (non-toxic) levels: Preservation of neuroelectrical function Reduction of infarct size Preservation of brain blood flow Reduction of brain oedema Reduction of intracranial pressure. o Should be considered as an adjuvant to first-aid O2 therapy and hyperbaric recompression. It's not an alternative to recompression, unless recompression is not obtainable. Aspirin and NSAID drugs o No evidence that they may significantly influence the outcome. PREVENTION OF DCI Risk factors o Exposure profile o Recent diving or hyperbaric exposure o Increasing age o Areas of anatomical change (++ tissue scarring) o Gender: no sex ratio, but ♀ have a proportionally higher body fat content. o Poor aerobic fitness and obesity o Presence of a right-to-left shunt (PFO…) o Repeat exposures o Physical exertion before or during exposure Strategies to reduce the risk of DCI o Standard schedules and procedures for altitude exposure o Pre-exposure denitrogenation by breathing FiO2 100% o Decompression staging where possible o Adequate protection against hypoxia o Adequate thermal protection o Identification and correction of any specific correctable factors ©Jean-Michel Ferrieux-2011 9 DAvMed 44 Decompression sickness — 7/129 & 50/757 KCL 2011 FLYING AFTER DIVING AND AIR TRANSPORT OF THE DIVING CASUALTY Pre-flight surface interval: o 12 hours after less than 2 hours of no-stop diving in the preceding 48 hours o 24 hours for multi-day or unlimited diving o 48 hours after decompression dives If a casualty with DCI needs to be transportable by air ➪advice should be obtained from the diving medicine specialist managing the case. ©Jean-Michel Ferrieux-2011 10