ARAMCHOL*
Chemical Name: Cholan-24-oic acid, 7, 12-dihydroxy-3-[(1-oxoeicosyl)
amino]-, (3β, 5β, 7α, 12 α).
As presented at The Liver Meeting – the 65th Annual
Meeting of the American Association for the Study of
Liver Diseases
November 7-11, 2014
Boston, MA
Compilation produced by Galmed Pharmaceuticals Ltd.
*Caution –ARAMCHOL is Limited to Investigational Use by the FDA
Table of Content
Abstracts
1. Treatment of preestablished diet-induced fatty liver by oral fatty acid-bile acid
conjugatesirodents….................................................................................................3
2. ABCA1-dependent but apoA-I-independent cholesterol efflux mediated by fatty acidbile acid conjugates (FABACs).................................................................................4
3. Fatty acid bile acid conjugate inhibits hepatic stearoyl coenzyme A desaturase and is
non-atherogenic.........................................................................................................5
4. The Fatty Acid-Bile Acid Conjugate Aramchol Reduces Liver Fat Content in Patients
With Nonalcoholic Fatty Liver Disease.....................................................................6
Posters
1. Inhibition Of Stearoyl Coenzyme A Desaturase (SCD1) Activity By Aramchol Reduces
Liver Fat And Presents A New Therapeutic Option In NAFLD And NASH.............8
2. A Phase-II, Randomized, Double Blind, Placebo-controlled Trial of Aramchol for the
Treatment of Non Alcoholic Fatty Liver Disease (NAFLD & NASH)......................9
2
Eur J Gastroenterol Hepatol. 2008 Dec;20(12):1205-13. doi: 10.1097/MEG.0b013e3282fc9743.
Treatment of preestablished diet-induced fatty liver by oral fatty acidbile acid conjugates in rodents.
Leikin-Frenkel A1, Goldiner I, Leikin-Gobbi D, Rosenberg R, Bonen H, Litvak A, Bernheim J,
Konikoff FM, Gilat T.
1
Minerva Center for Cholesterol Gallstones and Lipid Metabolism in the Liver, Tel-Aviv
University, Tel-Aviv, Israel.
Abstract
BACKGROUND:
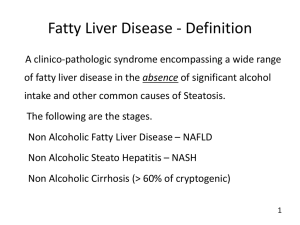
Nonalcoholic fatty liver disease (NAFLD) is the most common chronic liver disease in
industrialized countries. It has no accepted medical therapy. Fatty acid-bile acid conjugates
(FABACs) were proven to prevent diet-induced NAFLD in rodents.
AIM:
This study was undertaken to test whether oral FABACs are also effective in reducing liver fat in
preestablished diet-induced NAFLD.
METHODS:
NAFLD was induced in mice and rats by a high-fat diet and maintained by various proportions
thereof. The FABACs used were conjugates of cholic acid with either arachidic or stearic acids.
RESULTS:
FABAC therapy reduced liver fat in all four series of experiments. The rapidity of the effect was
inversely proportional to the concentration of fat in the maintenance diet. In mice on a 25%
maintenance diet FABACs decreased total liver lipids by about 30% in 4 weeks (P<0.03).
Diglycerides (P<0.003) and triglycerides (P<0.01) were the main neutral liver lipids that decreased
during FABAC therapy. Both FABACs tested reduced liver fat in NAFLD at doses of 25 and 150
mg/kg/day. High-fat diet increased, whereas FABAC therapy decreased plasma 16 : 1/(16 : 0+16 :
1) fatty acid ratio - a marker of stearoyl CoA desaturase activity. In HepG2 cells FABACs decreased
de-novo fatty acid synthesis dose dependently.
CONCLUSION:
Oral FABAC therapy decreased liver fat in preestablished NAFLD in mice and rats. Inhibition of
stearoyl CoA desaturase activity and fatty acid synthesis are mechanisms that may contribute to this
decrease. FABACs may be potential therapeutic agents for human NAFLD.
3
Biochem J. 2006 Jun 15;396(3):529-36.
ABCA1-dependent but apoA-I-independent cholesterol efflux mediated
by fatty acid-bile acid conjugates (FABACs).
Goldiner I1, van der Velde AE, Vandenberghe KE, van Wijland MA, Halpern Z, Gilat T, Konikoff
FM, Veldman RJ, Groen AK.
Author information
1
AMC Liver Centre, Academic Medical Centre, Amsterdam, The Netherlands.
Abstract
FABACs (fatty acid-bile acid conjugates) are synthetic molecules that are designed to treat a range
of lipid disorders. The compounds prevent cholesterol gallstone formation and diet-induced fatty
liver, and increase reverse cholesterol transport in rodents. The aim of the present study was to
investigate the effect of FABACs on cholesterol efflux in human cells. Aramchol (3betaarachidylamido-7alpha,12alpha,5beta-cholan-24-oic acid) increased cholesterol efflux from human
skin fibroblasts in a dose-dependent manner in the absence of known efflux mediators such as apoAI (apolipoprotein A-I), but had little effect on phospholipid efflux. An LXR (liver X receptor)
agonist strongly increased Aramchol-induced cholesterol efflux; however, in ABCA1 (ATPbinding cassette transporter A1)-deficient cells from Tangier disease patients, the Aramchol effect
was absent, indicating that activity of ABCA1 was required. Aramchol did not affect ABCA1
expression, but plasma membrane levels of the transporter increased 2-fold. Aramchol is the first
small molecule that induces ABCA1-dependent cholesterol efflux without affecting transcriptional
control. These findings may explain the beneficial effect of the compound on atherosclerosis.
Arch Med Res. 2010 Aug;41(6):397-404. doi: 10.1016/j.arcmed.2010.09.001.
4
Fatty acid bile acid conjugate inhibits hepatic stearoyl coenzyme A
desaturase and is non-atherogenic.
Leikin-Frenkel A1, Gonen A, Shaish A, Goldiner I, Leikin-Gobbi D, Konikoff FM, Harats D, Gilat
T.
Author information
1
Minerva Center for Cholesterol Gallstones and Lipid Metabolism in the Liver, Tel-Aviv
University, Tel-Aviv, Israel.
Abstract
BACKGROUND AND AIMS:
Suppression of stearoyl-coenzyme A desaturase (SCD) activity leads to reduction of obesity, fatty
liver as well as of insulin resistance. It was, however, recently reported to enhance atherogenesis.
The aim of the present study was to investigate whether inhibition of SCD by Aramchol, a fatty acid
bile conjugate with known hypocholesterolemic effects, will affect atherogenesis and how.
METHODS:
Aramchol was tested in vitro in cultured cells and in vivo in rodents.
RESULTS:
Aramchol, at very low concentrations, reduced SCD activity in liver microsomes of mice. Aramchol
enhanced cholesterol efflux from macrophages more than twofold. In vivo it increased fecal sterol
output and decreased markedly plasma cholesterol levels in mice. In ApoE(-/-), LDRL(-/-) and
C57Bl6 mice, the effects of Aramchol on atherogenesis were non-atherogenic.
CONCLUSIONS:
Aramchol reduces SCD activity and is non-atherogenic. It may offer a means to obtain the desirable
hepatic metabolic effects of SCD inhibition without the deleterious atherogenic effect.
Copyright © 2010 IMSS. Published by Elsevier Inc. All rights reserved.
Clin Gastroenterol Hepatol. 2014 May
10.1016/j.cgh.2014.04.038. [Epub ahead of print]
5
9.
pii:
S1542-3565(14)00673-9.
doi:
The Fatty Acid-Bile Acid Conjugate Aramchol Reduces Liver Fat
Content in Patients With Nonalcoholic Fatty Liver Disease.
Safadi R1, Konikoff FM2, Mahamid M3, Zelber-Sagi S4, Halpern M5, Gilat T6, Oren R7; FLORA
Group.
Collaborators (23)
Safadi R, Konikoff FM, Hershkovitz A, Gilat T, Halpern M, Rosenthal-Galili Z, Zuckerman E,
Abu-Mouch S, Fich A, Sikuler E, Issachar A, Assy N, Baruch Y, Lurie Y, Graif M, Stern N, Yaron
M, Blank A, Ben Bashat D, Zelber-Sagi S, Mahamid M, Mizrahi M, Oren R.
Author information
1
Liver and Gastroenterology Unit, Division of Medicine, Hadassah University Medical Center,
Jerusalem; Holy Family Hospital, Nazareth. Electronic address: safadi@hadassah.org.il.
2
Department of Gastroenterology and Hepatology, University of Tel Aviv, Meir Medical Center,
Kfar Saba.
3
Holy Family Hospital, Nazareth.
4
Department of Gastroenterology, Tel Aviv Sourasky Medical Center, Tel-Aviv; School of Public
Health, Faculty of Social Welfare and Health Sciences, University of Haifa, Haifa.
5
Galmed Medical Research, Limited, Tel-Aviv, Israel.
6
Department of Gastroenterology, Tel Aviv Sourasky Medical Center, Tel-Aviv; Galmed Medical
Research, Limited, Tel-Aviv, Israel.
7
Liver and Gastroenterology Unit, Division of Medicine, Hadassah University Medical Center,
Jerusalem; Department of Gastroenterology, Tel Aviv Sourasky Medical Center, Tel-Aviv.
Abstract
BACKGROUND & AIMS:
We investigated the effects of the fatty acid-bile acid conjugate 3β-arachidyl-amido, 7α-12αdihydroxy, 5β-cholan-24-oic acid (Aramchol; Trima Israel Pharmaceutical Products Ltd, Maabarot,
Israel) in a phase 2 trial of patients with nonalcoholic fatty liver disease (NAFLD).
METHODS:
We performed a randomized, double-blind, placebo-controlled trial of 60 patients with biopsyconfirmed NAFLD (6 with nonalcoholic steatohepatitis) at 10 centers in Israel. Patients were given
Aramchol (100 or 300 mg) or placebo once daily for 3 months (n = 20/group). The main end point
was the difference between groups in the change in liver fat content according to magnetic
resonance spectroscopy. The secondary end points focused on the differences between groups in
alterations of liver enzyme levels, levels of adiponectin, homeostasis model assessment scores, and
endothelial function.
6
RESULTS:
No serious or drug-related adverse events were observed in the 58 patients who completed the study.
Over 3 months, liver fat content decreased by 12.57% ± 22.14% in patients given 300 mg/day
Aramchol, but increased by 6.39% ± 36.27% in the placebo group (P = .02 for the difference
between groups, adjusted for age, sex, and body mass index). Liver fat content decreased in the 100mg Aramchol group, by 2.89% ± 28.22%, but this change was nonsignificant (P = .35), indicating
a dose-response relationship (P for trend = .01). Groups given Aramchol had nonsignificant
improvements over time in endothelial function and levels of alanine aminotransferase and
adiponectin, but homeostasis model assessment scores did not change. The appropriateness of a
single daily dose was confirmed by pharmacokinetic analysis.
CONCLUSIONS:
Three months' administration of the fatty acid-bile acid conjugate Aramchol is safe, tolerable, and
significantly reduces liver fat content in patients with NAFLD. The reduction in liver fat content
occurred in a dose-dependent manner and was associated with a trend of metabolic improvements,
indicating that Aramchol might be used for the treatment of fatty liver disease. ClinicalTrials.gov
number: NCT01094158.
Copyright © 2014 AGA Institute. Published by Elsevier Inc. All rights reserved
7