Liver Abscess - Dis Lair
advertisement

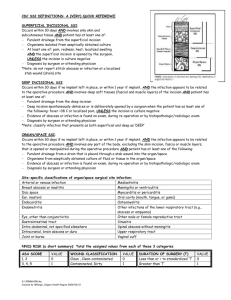
Liver Abscess Introduction Background Bacterial abscess of the liver is relatively rare. It has been described since the time of Hippocrates (400 BC), with the first published review by Bright appearing in 1936. In 1938, Ochsner's classic review heralded surgical drainage as the definitive therapy; however, despite the more aggressive approach to treatment, the mortality rate remained at 6080%. Computed tomography (CT) scan findings of liver abscess are shown. A large, septated abscess of the right hepatic lobe is revealed. Abscess was successfully treated with percutaneous drainage and antimicrobial therapy. Computed tomography scan findings of liver abscess are shown. A large anterior abscess involving the left hepatic lobe is revealed. Abscess was successfully treated with percutaneous drainage and antimicrobial therapy. The development of new radiologic techniques, the improvement in microbiologic identification, and the advancement of drainage techniques, as well as improved supportive care, have decreased mortality rates to 5-30%; yet, the prevalence of liver abscess has remained relatively unchanged. Untreated, this infection remains uniformly fatal. The 3 major forms of liver abscess, classified by etiology, are as follows: 1. Pyogenic abscess, which is most often polymicrobial, accounts for 80% of hepatic abscess cases in the United States. 2. Amebic abscess due to Entamoeba histolytica accounts for 10% of cases. 3. Fungal abscess, most often due to Candida species, accounts for less than 10% of cases. Pathophysiology The liver receives blood from both systemic and portal circulations. Increased susceptibility to infections would be expected given the increased exposure to bacteria. However, Kupffer cells lining the hepatic sinusoids clear bacteria so efficiently that infection rarely occurs. Multiple processes have been associated with the development of hepatic abscesses; their relative frequencies are listed in the image below. Appendicitis was traditionally the major cause of liver abscess. As diagnosis and treatment of this condition has advanced, its frequency as a cause for liver abscess has decreased to 10%. Biliary tract disease is now the most common source of pyogenic liver abscess (PLA). Obstruction of bile flow allows for bacterial proliferation. Biliary stone disease, obstructive malignancy affecting the biliary tree, stricture, and congenital diseases are common inciting conditions. With a biliary source, abscesses usually are multiple, unless they are associated with surgical interventions or indwelling biliary stents. In these instances, solitary lesions can be seen. Infections in organs in the portal bed can result in a localized septic thrombophlebitis, which can lead to liver abscess. Septic emboli are released into the portal circulation, trapped by the hepatic sinusoids, and become the nidus for microabscess formation. These microabscesses initially are multiple but usually coalesce into a solitary lesion. Microabscess formation can also be due to hematogenous dissemination of organisms in association with systemic bacteremia, such as endocarditis and pyelonephritis. Cases also are reported in children with underlying defects in immunity, such as chronic granulomatous disease and leukemia. Approximately 4% of liver abscesses result from fistula formation between local intra-abdominal infections. Despite advances in diagnostic imaging, cryptogenic causes account for a significant proportion of cases; surgical exploration has impacted this minimally. These lesions usually are solitary in nature. Penetrating hepatic trauma can inoculate organisms directly into the liver parenchyma, resulting in pyogenic liver abscess. Nonpenetrating trauma can also be the precursor to pyogenic liver abscess by causing localized hepatic necrosis, intrahepatic hemorrhage, and bile leakage. The resulting tissue environment permits bacterial growth, which may lead to pyogenic liver abscess. These lesions are typically solitary. Pyogenic liver abscess has been reported as a secondary infection of amebic abscess, hydatid cystic cavities, and metastatic and primary hepatic tumors. It is also a known complication of liver transplantation, hepatic artery embolization in the treatment of hepatocellular carcinoma, and the ingestion of foreign bodies, which penetrate the liver parenchyma. Trauma and secondarily infected liver pathology account for a small percentage of liver abscess cases. The right hepatic lobe is affected more often than the left hepatic lobe by a factor of 2:1. Bilateral involvement is seen in 5% of cases. The predilection for the right hepatic lobe can be attributed to anatomic considerations. The right hepatic lobe receives blood from both the superior mesenteric and portal veins, whereas the left hepatic lobe receives inferior mesenteric and splenic drainage. It also contains a denser network of biliary canaliculi and, overall, accounts for more hepatic mass. Studies have suggested that a streaming effect in the portal circulation is causative. Frequency United States The incidence of pyogenic liver abscess has essentially remained unchanged by both hospital and autopsy data. Liver abscess was diagnosed in 0.7%, 0.45%, and 0.57% of autopsies during the periods of 1896-1933, 1934-1958, and 1959-1968, respectively. The frequency in hospitalized patients ranges from 8-16 cases per 100,000 persons. Studies suggest a small, but significant, increase in the frequency of liver abscess. Mortality/Morbidity Untreated, pyogenic liver abscess remains uniformly fatal. With timely administration of antibiotics and drainage procedures, mortality currently occurs in 5-30% of cases. The most common causes of death include sepsis, multiorgan failure, and hepatic failure.2 Sex While abscesses once showed a predilection for males in earlier decades, no sexual predilection currently exists. Males have a poorer prognosis from hepatic abscess than females. Age 1. Prior to the antibiotic era, liver abscess was most common in the fourth and fifth decades of life, primarily due to complications of appendicitis. With the development of better diagnostic techniques, early antibiotic administration, and the improved survival of the general population, the demographic has shifted toward the sixth and seventh decades of life. Frequency curves display a small peak in the neonatal period followed by a gradual rise beginning at the sixth decade of life. 2. Cases of liver abscesses in infants have been associated with umbilical vein catheterization and sepsis. 3. When abscesses are seen in children and adolescents, underlying immune deficiency, severe malnutrition, or trauma frequently exists. Clinical History 1. See the image below for the presenting symptoms and signs in 715 patients described in the literature. 2. The most frequent symptoms of hepatic abscess include the following: o Fever (either continuous or spiking) o Chills o Right upper quadrant pain o Anorexia o Malaise 3. Cough or hiccoughs due to diaphragmatic irritation may be reported. 4. Referred pain to the right shoulder may be present. 5. Individuals with solitary lesions usually have a more insidious course with weight loss and anemia of chronic disease. With such symptoms, malignancy often is the initial consideration. 6. Fever of unknown origin (FUO) frequently can be an initial diagnosis in indolent cases. Multiple abscesses usually result in more acute presentations, with symptoms and signs of systemic toxicity. 7. Afebrile presentations have been documented. Physical 1. Fever and tender hepatomegaly are the most common signs. 2. A palpable mass need not be present. 3. Mid epigastric tenderness, with or without a palpable mass, is suggestive of left hepatic lobe involvement. 4. Decreased breath sounds in the right basilar lung zones, with signs of atelectasis and effusion on examination or radiologically, may be present. 5. A pleural or hepatic friction rub can be associated with diaphragmatic irritation or inflammation of Glisson capsule. 6. Jaundice may be present in as many as 25% of cases and usually is associated with biliary tract disease or the presence of multiple abscesses. Causes Polymicrobial involvement is common, with Escherichia coli and Klebsiella pneumoniae being the 2 most frequently isolated pathogens. Reports suggest that K pneumoniae is an increasingly prominent cause.3 The image below lists the common etiologic agents. 1. Enterobacteriaceae are especially prominent when the infection is of biliary origin. Abscesses involving K pneumoniae have been associated with multiple cases of endophthalmitis. 2. The pathogenic role of anaerobes was underappreciated until the isolation of anaerobes from 45% of cases of pyogenic liver abscess was reported in 1974. Since that time, increasing rates of anaerobic involvement have been reported, likely because of increased awareness and improved culturing techniques. The most frequently encountered anaerobes are Bacteroides species, Fusobacterium species, and microaerophilic and anaerobic streptococci. A colonic source is usually the initial source of infection. 3. Staphylococcus aureus abscesses usually result from hematogenous spread of organisms involved with distant infections, such as endocarditis. S milleri is neither anaerobic nor microaerophilic. It has been associated with both monomicrobial and polymicrobial abscesses in patients with Crohn disease, as well as with other patients with pyogenic liver abscess. 4. Amebic liver abscess is most often due to E histolytica. Liver abscess is the most common extraintestinal manifestation of this infection. 5. Fungal abscesses primarily are due to Candida albicans and occur in individuals with prolonged exposure to antimicrobials, hematologic malignancies, solid-organ transplants, and congenital and acquired immunodeficiency. Cases involving Aspergillus species have been reported. 6. Other organisms reported in the literature include Actinomyces species, Eikenella corrodens, Yersinia enterocolitica, Salmonella typhi, and Brucella melitensis. Differential Diagnoses Biliary Disease Hydatid Cysts Cholecystitis Pneumonia, Bacterial Empyema, Pleuropulmonary Gastritis, Acute Hepatocellular Carcinoma Other Problems to Be Considered Hepatitis, nonviral Metastatic disease of the liver Workup Laboratory Studies 1. CBC count with differential o Anemia of chronic disease o Neutrophilic leukocytosis 2. Liver function studies Hypoalbuminemia and elevation of alkaline phosphatase (most common abnormalities) Elevations of transaminase and bilirubin levels (variable) 3. Blood cultures are positive in roughly 50% of cases. 4. Culture of abscess fluid should be the goal in establishing microbiologic diagnosis. 5. Enzyme immunoassay should be performed to detect E histolytica in patients either from endemic areas or who have traveled to endemic areas. Imaging Studies 1. The advancement in radiologic techniques has been credited with the improvement in mortality rates. 2. Computed tomography (CT) scan evaluation with contrast and ultrasonography remain the radiologic modalities of choice as screening procedures and also can be used as techniques for guiding percutaneous aspiration and drainage. 3. With advancements in multidetector CT scan technology, image quality has improved dramatically, allowing for improved detection. 4. CT scan (sensitivity 95-100%; see images below.) Lesions on CT evaluation are well-demarcated areas hypodense to the surrounding hepatic parenchyma. Peripheral enhancement is seen when IV contrast is administered. Gas can be seen in as many as 20% of lesions. CT scan is superior in its ability to detect lesions less than 1 cm. This technique also enables the evaluation for an underlying concurrent pathology throughout the abdomen and pelvis. Indium-labeled WBC scans are somewhat more sensitive in this regard. 5. Ultrasonography (sensitivity 80-90%) Ultrasonographic evaluation reveals hypoechoic masses with irregularly shaped borders. Internal septations or cavity debris may be detected. Ultrasonography allows for close evaluation of the biliary tree and simultaneous aspiration of the cavity. The major benefits of this technique are its portability and diagnostic utility in patients who are too critical to undergo prolonged radiologic evaluation or to be moved out of monitored setting. Operator dependence affects its overall sensitivity. 6. Gallium and technetium radionuclide scanning (sensitivity 50-90%) The initial studies are used in diagnosis. These techniques use the fact that the radiopharmaceuticals share the same uptake, transport, and excretion pathways as bilirubin and, thus, are effective agents in evaluating liver disease. Sensitivity varies with the radiopharmaceutical utilized, technetium (80%), gallium (50-80%), and indium (90%). Limitations include a delay in diagnosis and the need for confirmatory procedures; thus, they offer no benefit over other imaging modalities. 7. Chest radiographic findings of basilar atelectasis, right hemidiaphragm elevation, and right pleural effusion are present in approximately 50% of cases; before advancements in radiologic technique, these served as diagnostic clues. Pneumonias or pleural diseases often are initially considered because of the radiographic findings. Procedures 1. Percutaneous needle aspiration Under CT scan or ultrasound guidance, needle aspiration of cavity material can be performed. Needle aspiration enables rapid recovery of material for microbiologic and pathologic evaluation. Needle aspiration can be performed with the initial diagnostic procedure. 2. Percutaneous catheter drainage Percutaneous drainage has become the standard of care and should be the first intervention considered for small cysts. For cysts greater than 5 cm, ruptured cysts, and multiloculated cysts, surgical drainage is generally recommended over percutaneous intervention. Advantages include reduced costs, recovery time, and postprocedure recovery rate; it eliminates the need for general anesthesia. This also allows for gradual, controlled drainage. A catheter is placed under ultrasound or CT guidance using the Seldinger or trocar techniques. The catheter is flushed daily until output is less than 10 cc/d or cavity collapse is documented by serial CT scanning. 4. Medical Care 1. An untreated hepatic abscess is nearly uniformly fatal due to complications that include sepsis, empyema, or peritonitis from rupture into the pleural or peritoneal spaces, and retroperitoneal extension. Treatment should include drainage, either percutaneous or surgical. 2. Antibiotic therapy as a sole treatment modality is not routinely advocated, though it has been successful in a few reported cases. It may be the only alternative in patients too ill to undergo invasive procedures or in those with multiple abscesses not amenable to percutaneous or surgical drainage. In these instances, patients are likely to require many months of antimicrobial therapy with serial imaging and close monitoring for associated complications. 3. Antimicrobial treatment is a common adjunct to percutaneous or surgical drainage. Surgical Care Surgical drainage was the standard of care until the introduction of percutaneous drainage techniques in the mid 1970s. With the refinement of image-guided techniques, percutaneous drainage and aspiration have become the standard of care. 1. Current indications for the surgical treatment of pyogenic liver abscess are for the treatment of underlying intra-abdominal processes, including signs of peritonitis; existence of a known abdominal surgical pathology (eg, diverticular abscess); failure of previous drainage attempts; and the presence of a complicated, multiloculated, thick-walled abscess with viscous pus. 2. Shock with multisystem organ failure is a contraindication to surgery. 3. Open surgery can be performed by 2 approaches. A transperitoneal approach allows for abscess drainage and abdominal exploration to identify previously undetected abscesses and the location of an etiologic source. For high posterior lesions, a posterior transpleural approach can be used. Although this allows easier access to the abscess, the identification of multiple lesions or a concurrent intra-abdominal pathology is lost. Until cultures are available, the choice of antimicrobial agents should be directed toward the most commonly involved pathogens. Regimens using beta-lactam/betalactamase inhibitor combinations, carbapenems, or secondgeneration cephalosporins with anaerobic coverage are excellent empiric choices for the coverage of enteric bacilli and anaerobes. Metronidazole or clindamycin should be added for the coverage of Bacteroides fragilis if other employed antibiotics offer no anaerobic coverage. Amebic abscess should be treated with metronidazole, which will be curative in 90% of cases. Metronidazole should be initiated before serologic test results are available. Patients who do not respond to metronidazole should receive chloroquine alone or in combination with emetine or dehydroemetine. Systemic antifungal agents should be initiated if fungal abscess is suspected and after the abscess has been drained percutaneously or surgically. Initial therapy for fungal abscess is currently amphotericin B. Lipid formulations may offer some benefit in that the complexing of drug to lipid moieties Multiple abscesses have been drained successfully by this method. Failure to respond to catheter drainage is the main reported complication and is also an indication for surgical intervention. Other complications reported (rarely) are bleeding at the catheter site, perforation of hollow viscus, and peritonitis from intraperitoneal spillage of cavity fluid. Contraindications include coagulopathy; a difficult access path to the cavity; peritonitis; and/or a complicated, multiloculated, thick-walled abscess with viscous pus. Treatment A laparoscopic approach is also commonly used in select cases. This minimally invasive approach affords the opportunity to explore the entire abdomen and to significantly reduce patient morbidity. A growing literature is defining the optimal population for this mode of intervention. 5. A retrospective chart review compared surgery versus percutaneous drainage for liver abscesses greater than 5 cm. The morbidity was comparable for the 2 procedures, but those treated with surgery had fewer secondary procedures and fewer treatment failures. 6. Postoperative complications are not uncommon and include recurrent pyogenic liver abscess, intra-abdominal abscess, hepatic or renal failure, and wound infection. Consultations 1. Interventional radiology: Obtain a consultation as soon as the diagnosis is considered to allow rapid collection of cavity fluid and the potential for early therapeutic drainage of abscess. 2. General surgery Immediately seek a consultation with a general surgeon if the source of the abscess is a known underlying abdominal pathology or in cases with peritonitis. In cases undergoing percutaneous drainage, seek the involvement of a general surgeon if drainage of the abscess cavity is unsuccessful. 3. Gastroenterology involvement may be useful after successful drainage to evaluate for underlying gastrointestinal disease using colonoscopy or endoscopic retrograde cholangiopancreatography (ERCP). 4. Infectious disease consultation should be considered in complicated cases and when the involved pathogens are unusual or difficult to treat, such as in fungal abscesses. Medication allows for concentration in hepatocytes. Further investigation is required for definitive proof. Cases of successful fluconazole treatment after amphotericin failure have been reported; however, its use as an initial agent is still being studied. Ultimately, the organisms isolated and antibiotic sensitivities should guide the final choice of antimicrobials. Duration of treatment has always been debated. Short courses (2 wk) of therapy after percutaneous drainage have been successful in a small series of patients; however, most series have reported recurrence of abscess even after more prolonged courses. Currently 4-6 weeks of therapy is recommended for solitary lesions that have been adequately drained. Multiple abscesses are more problematic and can require up to 12 weeks of therapy. Both the clinical and radiographic progress of the patient should guide the length of therapy. Antibiotics Empiric antimicrobial therapy must be comprehensive and should cover all likely pathogens in the context of the clinical setting. Meropenem (Merrem) Bactericidal broad-spectrum carbapenem antibiotic that inhibits cell-wall synthesis. Effective against most grampositive and gram-negative bacteria. Has slightly increased activity against gram negatives and slightly decreased activity against staphylococci and streptococci species compared to imipenem. Adult 1.0 g IV q8h Pediatric 40 mg/kg IV q8h Imipenem and cilastatin (Primaxin) For treatment of multiple organism infections in which other agents do not have wide-spectrum coverage or are contraindicated due to potential for toxicity. Adult Base initial dose on severity of infection, and administer in equally divided doses; dose may range from 250-500 mg IV q6h for maximum of 3-4 g/d Alternatively, 500-750 mg IM q12h or intra-abdominally Pediatric <12 years: Not established; 15-25 mg/kg/dose IV q6h suggested for > 3 months Fully susceptible organisms: Not to exceed 2 g/d IV Infections with moderately susceptible organisms: Not to exceed 4 g/d Cefuroxime (Ceftin) Second-generation cephalosporin maintains gram-positive activity that first-generation cephalosporins have; adds activity against Proteus mirabilis, Haemophilus influenzae, Escherichia coli, Klebsiella pneumoniae, and Moraxella catarrhalis. Condition of patient, severity of infection, and susceptibility of microorganism determine proper dose and route of administration. Adult 500 mg PO bid for 20 d Pediatric Children: 250 mg PO bid for 20 d Adolescents: Administer as in adults Cefotetan (Cefotan) Second-generation cephalosporin indicated for infections caused by susceptible gram-positive cocci and gram-negative rods. Dosage and route of administration depends on condition of patient, severity of infection, and susceptibility of causative organism. Adult 1-2 g IV/IM q12h for 5-10 d Pediatric 20-40 mg/kg/dose IV/IM q12h for 5-10 d Cefoxitin (Mefoxin) Second-generation cephalosporin indicated for gram-positive cocci and gram-negative rod infections. Infections caused by cephalosporin-resistant or penicillin-resistant gram-negative bacteria may respond to cefoxitin. Adult 1-2 g IV q6-8h Pediatric Infants and children: 80-160 mg/kg/d IV divided q4-6h; higher doses for severe or serious infections; not to exceed 12 g/d Cefaclor (Ceclor) Second-generation cephalosporin indicated for infections caused by susceptible gram-positive cocci and gram-negative rods. Determine proper dosage and route based on condition of patient, severity of infection, and susceptibility of causative organism. Adult 250-500 mg PO q8h Pediatric 20-40 mg/kg/d PO divided q8-12h; not to exceed 2 g/d Clindamycin (Cleocin) Lincosamide for treatment of serious skin and soft tissue staphylococcal infections. Also effective against aerobic and anaerobic streptococci (except enterococci). Inhibits bacterial growth, possibly by blocking dissociation of peptidyl t-RNA from ribosomes causing RNA-dependent protein synthesis to arrest. Adult 150-450 mg/dose PO q6-8h; not to exceed 1.8 g/d 600-1200 mg/d IV/IM divided q6-8h, depending on degree of infection Pediatric 8-20 mg/kg/d PO as hydrochloride and 8-25 mg/kg/d as palmitate divided tid/qid 20-40 mg/kg/d IV/IM divided tid/qid Metronidazole (Flagyl) Imidazole ring-based antibiotic active against various anaerobic bacteria and protozoa. Used in combination with other antimicrobial agents (except for Clostridium difficile enterocolitis). Adult Loading dose: 15 mg/kg or 1 g for 70-kg adult IV over 1 h Maintenance dose: 6 h following loading dose; infuse 7.5 mg/kg or 500 mg IV for 70-kg adult over 1 h q6-8h; not to exceed 4 g/d Pediatric 15-30 mg/kg/d PO divided bid/tid for 7 d, or 40 mg/kg once; do not exceed 2 g/d Antifungal agents Their mechanism of action may involve an alteration of RNA and DNA metabolism or an intracellular accumulation of peroxide that is toxic to the fungal cell. Amphotericin B (AmBisome) Produced by a strain of Streptomyces nodosus; can be fungistatic or fungicidal. Binds to sterols, such as ergosterol, in the fungal-cell membrane, causing intracellular components to leak with subsequent fungal-cell death. Adult 3-5 mg/kg/d IV of liposomal amphotericin B over approximately 120 min Pediatric Administer as in adults Fluconazole (Diflucan) Synthetic oral antifungal (broad-spectrum bistriazole) that selectively inhibits fungal cytochrome P-450 and sterol C-14 alpha-demethylation. Adult 150 mg PO once or 400 mg/d, depending on severity of infection Pediatric 3-6 mg/kg/d PO for 14-28 d or 6-12 mg/kg/d, depending on severity of infection Follow-up Further Inpatient Care 1. Aggressively seek an underlying source of the abdominal pathology. 2. Perform weekly serial CT scans or ultrasound examinations to document adequate drainage of abscess cavity. 3. Maintain drains until the output is less than 10 cc/d. 4. Monitor fever curves. Persistent fever after 2 weeks of therapy may indicate the need for more aggressive drainage. 5. For patients with an underlying malignancy, definitive treatment, such as surgical removal of the mass, should be pursued if at all possible. Further Outpatient Care 1. Patients will require prolonged parenteral antimicrobial therapy that may continue after discharge. Monitoring of medication levels, renal function, and blood counts may be needed. Enteral nutrition is the preferred route unless it is clinically contraindicated. 2. Drain care may be required. 3. Continue radiologic evaluation to document progress of therapy after discharge. Complications 1. Sepsis 2. Empyema resulting from contiguous spread or intrapleural rupture of abscess 3. Rupture of abscess with resulting peritonitis 4. Endophthalmitis when an abscess is associated with K pneumoniae bacteremia Prognosis 1. If a liver abscess is left untreated, the prognosis is uniformly fatal. 2. Indicators of a poor prognosis have been described since 1938 and include multiplicity of abscesses, underlying malignancy, severity of underlying medical conditions, presence of complications, and delay in diagnosis.2 3. Indicators of a poor prognosis in amebic abscess include a bilirubin level of greater than 3.5 mg/dL, encephalopathy, hypoalbuminemia (ie, serum albumin level of <2 g/dL), and multiple abscesses; all are independent factors that predict poor outcome. 4. An underlying malignant etiology and an Acute Physiology and Chronic Health Evaluation (APACHE II) score greater than 9 increases the relative mortality by 6.3-fold and 6.8-fold, respectively. 5. Chen et al examined prognostic factors for elderly patients with pyogenic liver abscess. 4 Results from the study, which included 118 patients aged 65 years or older and 221 patients below age 65 years, indicated that age and an APACHE II score of 15 or greater at hospital admission were risk factors for mortality. The evidence ultimately suggested that outcomes for older patients with pyogenic liver abscess are on a par with those for younger patients. The investigators also found that in the younger patient group, there was greater frequency of males suffering from alcoholism, a cryptogenic abscess, and K pneumoniae infection.