File - Brandi Malsy, CRNP
advertisement

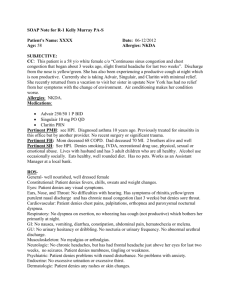
S- Subjective Data: S.M. - new visit, established patient at Calhoun County Health Department 20 y/o African American female, single History obtained from patient CC: “I’m here for my yearly pelvic exam and to get more birth control pills. I’ve also been having a white vaginal discharge for 3 days.” HPI: Patient presents to the Calhoun County Health Department for her yearly pelvic exam. Patient complains of having a thick, white vaginal discharge x 3 days with external and internal vaginal itching. Patient denies vaginal pain. Denies difficulty or painful urination. Denies any aggravating factors. Patient has used Vagisil x one day (one application) with minimal relief of itching Past Medical History: Vaginal yeast infection- June 2013 Medications: Ortho Cyclen PO daily Allergies: Penicillin- since 2004, causes rash Prior Illnesses/Injuries: MVC 2004- broken left hip Chicken pox- 2000 Previous Operations: Left hip pinning- April 2004 due to MVC Previous Hospitalizations: April 2004- left hip pinning due to fracture- denies complications during hospital stay. Flu vaccine: October 2014 Gardasil- October 2013 PPD Test- April 2014- negative findings Tetanus- June 2011 Family History: Mother- age 40- no medical problems Father- age 41- no medical problems Maternal Grandmother- age 59- HTN Maternal Grandfather- age 61- HTN Paternal Grandmother- Age 62- Type II Diabetes Paternal Grandfather- Age 62- no medical problems Social History: Patient is single and lives with her parents, three members of household. Pt is currently unemployed. She is a full-time college student at Jacksonville State Community College. Pt has an optimal support system. Patient has Alabama Medicaid/Family Planning. Patient states she sees a physician at Quality of Life clinic in Anniston when she is sick. Last dental visit- 2014. Pt denies use of alcohol or tobacco. Denies past or present use of recreational drugs. Nutrition: Pt eats a regular diet. Pt eats three meals daily, once in the morning, once at lunch, and once in the evening. Patient states she snacks throughout the day usually consuming 2 snacks daily, mainly consisting of sodas and potato chips or crackers. States she drinks 2-3 caffeinated beverages and 1-2 glasses of water a day. Review of Symptoms: 1. Constitutional: Patient denies fatigue or weakness, recent weight loss or gain, denies fever. 2. Eyes: Patient denies vision changes, blurry vision, eye drainage/tearing, eye pain/itching or eye redness. Denies photophobia. Last eye exam done at Quality of Life- January 2014 with no abnormal findings. Does not wear glasses or contacts. 3. ENMT: Patient denies vertigo, hearing loss, tinnitus, or use of assistive hearing devices. Denies ear pain, ear drainage. Denies nasal discharge or nosebleeds. Denies difficulty smelling. Pt denies facial/sinus pain or sinus drainage. Denies dental pain. Last dental visit at Sarrell Dental Clinic in Anniston, AL- September 2014 with normal findings. Patient states she brushes her teeth twice daily with fluoride toothpaste and flosses daily. Denies bleeding of gums, mouth odor, ulcers, or sores of the tongue. Denies sore throat, hoarseness, or difficulty swallowing. 4. Cardiovascular: Patient denies chest pain, changes in blood pressure, palpitations, or peripheral edema. Denies claudication or cyanosis of extremities. Denies leg redness or tenderness. 5. Respiratory: Patient denies SOB at rest or upon exertion, orthopnea, or dyspnea. Denies cough or wheezing. Reports exposure to second-hand smoke on a daily basis. Last CXR- January 2014 with normal findings. 6. Gastrointestinal: Patient denies any episodes of abdominal pain, nausea, vomiting, or diarrhea. Reports regular, daily BM’s. Last normal BM was today. Denies blood in stool, rectal bleeding, hemorrhoids, or constipation. Denies hematemesis. Denies heartburn. Reports normal appetite with no food intolerances. 7. Genitourinary: Patient denies dysuria, burning, urgency, hematuria, or frequency. Denies flank pain or suprapubic pain. Denies recent urinary tract or bladder infections. Complains of internal and external vaginal itching. Complains of a thick, white vaginal discharge x 3 days. Menarche at 11 years of age. LMP- 10/20/2014. Menstrual cycle lasts 4-6 days with light to moderate flow. No history of pregnancy. First sexual encounter was at 16 years of age. Reports 5 lifetime partners. Sexually active at present with one partner x 9 months. Preferred method of birth control is condoms and birth control pills. Uses condoms on a regular basis. Last sexual encounter was 4 days ago. Denies prior history of STD’s or dyspareunia. 8. Musculoskeletal: Patient denies body aches, muscle or joint pain, swelling, or stiffness. Denies recent injury or trauma. Denies muscle cramps or muscle weakness. Reports she is physically active on a daily basis and exercises four times a week. Denies neck pain or stiffness. Denies changes in range of motion of upper and lower extremities. 9. Skin: Patient denies skin lesions, rash, itching, moles, hair loss, or dryness. Reports daily sun exposure, but uses sunscreen when working outdoors. Denies any changes in skin condition. Denies doing selfbreast examinations on a regular basis. Denies any breast pain, dimpling, or nipple discharge. 10. Neurologic: Patient denies headaches, dizziness, or vertigo. Denies syncopal episodes, fatigue, or weakness. Denies muscle tremors, numbness, involuntary movements, or tingling. Denies sleep disturbances. 11. Psychiatric: Patient denies decrease in memory or recent mood changes. Denies history of depression, anxiety, hallucinations, or paranoia. 12. Endocrine: Patient denies intolerance to heat or cold, excessive sweating, thirst, or hunger. Denies any unexplained changes in weight. 13. Hematologic/Lymphatic: Patient denies excessive bleeding, bruising, or history of anemia. Denies any previous blood transfusions. Denies swollen lymph nodes or lymph node tenderness. Denies previous history of blood clots. 15. Allergic/Immunologic: Patient denies history of seasonal allergies. Denies previous allergy testing. Denies hives, rashes, or itchy, watery eyes. No exposure to blood or body fluids. Denies history of immunosuppression. O- Objective Data: 1. Constitutional/General appearance: Patient appears in no acute distress, well-developed, wellnourished 20 year old female. Appears stated age. Dressed appropriately and behaving in an appropriate manner. Alert and oriented x 3. Vital Signs: T- 98.6 oral, BP- 122/74 mm/Hg, HR-79 bpm, Respirations- 20/ minute, unlabored, Oxygen sat- 100% on room air, Height- 63 inches, Weight- 138 lbs, BMI- 24.44 Physical Examination: 2. Eyes: Sclera normal. No drainage or tearing noted from eyes, no redness. PERRLA. 4 mm bilaterally. 3. ENT/Mouth: Tympanic membranes normal, no bulging or redness noted, light reflex present. Hearing intact to whispered voice. Nasal turbinates normal, no nasal drainage noted, no deviated septum, no lesions noted. Maxillary and frontal sinuses nontender upon light palpation. Oral cavity mucosa pink and moist. No dental caries noted. Oropharynx clear with no exudate visualized, tonsils present and normal, uvula midline. No evidence of bleeding of gums or foul odor, no ulcers or sores. Cardiovascular: Apical pulse normal. Regular rate and rhythm noted. Normal S1 and S2. No S3 or S4. No murmurs, clicks, or gallops. Peripheral pulses with normal rate and rhythm. No JVD. No carotid bruits auscultated. No edema noted to upper or lower extremities. Capillary refill brisk, < 3 seconds. No discoloration noted to extremities. No varicose veins. Respiratory: Equal rise and fall of chest visualized. No tenderness upon palpation. Patient with normal rate and effort. Normal tactile fremitus. No hyperresonnance or dullness noted upon palpation. Normal breath sounds auscultated in upper and lower lobes bilaterally. No rhonchi or wheezing auscultated. No clubbing noted. Abdomen: Abdomen soft and nondistended. Bowel sounds normal in all four quadrants. No tenderness noted upon light or deep palpation. No guarding. Genitourinary: No CVA tenderness present. No suprapubic tenderness noted upon palpation. Normal hair distribution noted. Labia majora reddened, nontender. No swelling or lesions noted. Labia minora reddened, nontender, no lesions or swelling noted. Normal appearing skin of perineum and anus with no visible lesions. Speculum exam done without difficulty. Reddened vaginal mucosa noted. No edema noted to vagina or vaginal wall. Vagina nontender, no masses or nodularity noted. Thick, curd-like white discharge noted from vagina. No odor noted. Cervix midline; nulliparous cervical os visualized, pink with smooth, normal mucosa, no visible lesions noted on cervix. PAP performed. BME reveals no evidence of adnexal mass or tenderness. Uterus is midline, normal shape and size, mobile, no masses palpated, nontender upon exam. Bilateral adenexae without masses or tenderness palpated. Rectovaginal exam performed. Normal sphincter tone. Rectovaginal septum without masses, nodularity, or tenderness. Rectum without masses, nodularity, induration, or tenderness. Fecal occult blood testing performednegative. Musculoskeletal: Normal ROM noted in upper and lower extremities. Pt denies pain upon movement. Patient denies calf tenderness. Normal muscle strength in upper and lower extremities. No abnormal curvature of spine. Skin: Skin warm, dry, pink. No bruising noted. No discolored or uneven moles, open wounds, no redness or rashes noted. Breast exam done with fibrocystic changes noted in breasts bilaterally. No masses, nipple discharge, skin changes, or dimpling noted Neurological: Patient is alert and oriented x 3. Hand grips strong and equal bilaterally. Speech is clear. No tremors or involuntary movements. Psychiatric: Pt is calm, cooperative, behaving in an appropriate manner, answering questions appropriately. Normal affect. Hematologic/Lymphatic/Immunologic: No bruising noted. No enlarged lymph nodes palpated. Patient denies tenderness upon palpation of thyroid. Diagnostic Tests Performed at visit: 83020- Hemoglobin- 13.5- within normal range 81000- Urinalysis- normal findings 81025- Pregnancy test- negative 87621- PAP smear A- Assessment/Analysis: Level of Visit: Level 3- 99313 Diagnoses: 1. V72.3 Gynecological Exam 2. 112 Candidiasis (vaginal) 3. 616.1 Vaginitis and vulvovaginitis P- Plan: The following plan has been discussed and agreed upon by S.M. for the diagnoses including: 1. V72.3 Gynecological Exam a. Follow-up in one year- will call with PAP results. Patient to schedule appointment for her next yearly exam before leaving the clinic. b. Thirteen packs of Ortho Cyclen and twelve condoms given to patient. c. Patient informed to take Ortho Cyclen on a daily basis without skipping pills. d. Education on importance of practicing safe sex in order to prevent sexually transmitted diseases and unwanted pregnancy provided for patient. e. Patient instructed on how to properly perform self-breast examinations (SBE). Instructed patient to perform SBE on a monthly basis, preferably when she starts a new pack of birth control pills. 2. 112 Candidiasis a. Rx given for Diflucan (Fluconazole) 150 mg PO x one dose, dispense one, refill x one in one week; product selection permitted. Patient is instructed to repeat Diflucan 150 mg PO dose in one week. b. Instructed patient to return to clinic if no improvement after second dose of Diflucan. c. Encouraged patient to consume live culture yogurts or Acidophilus tablets to assist with alleviating symptoms. 3. 616.1 Vaginitis and Vulvovaginitis a. Informed patient Diflucan will help alleviate symptoms of vaginitis and vulvovaginitis. b. Stressed importance of taking Diflucan as prescribed. c. Educated patient on methods to prevent vaginal irritation such as avoiding tight fitting clothing, avoid bubble baths, and avoid nylon underwear. d. Educated patient on importance of not douching and no sexual intercourse until symptoms subside. e. Avoid tampons until symptoms subside. F. Good perineal hygiene. Diflucan (Fluconazole) - prescribed for this patient for treatment of vulvovaginal candidiasis and vaginitis. MOA- Interferes with cytochrome P450 activity, decreasing ergosterol synthesis (principal sterol in fungal cell membrane) and inhibiting cell membrane formation. Usual dosage- 150 mg tablet as one time dose and/or repeated 150 mg dose in one week from first dose. Available as name brand, Diflucan. Also available as generic, Fluconazole. Cost for two (2) doses of 150 mg Target Anniston, AL- Generic: $8.00; Brand: $4.26 Publix Oxford, AL- Generic: $18.50; Brand: $28.96 Wal-Mart Anniston, AL- Generic: $8.00; Brand: $4.98