Timothy He 2
advertisement
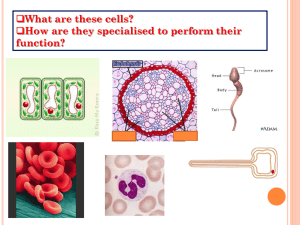
Timothy He When a body's organs fail, a person supposedly will not live much longer. With the recent discovery of organ transplantation though, organs, most importantly the heart, kidney, liver, lungs, or small intestine, can be replaced by donated organs. Organs can be damaged in various ways. The most popular are by hurting a developing embryo, being infected by disease, or gradual damage to delicate proteins. The largest problem after transplantation is rejection. This is when the human immune system recognizes the transplanted organ as a foreign body and tries to attack it. The lymphocytes and antibodies usually can recognize a bodiy's own organs through receptors on proteins, but since foreign organs have different receptors, they are counted as invaders. Ways currently employed to prevent rejection include matching blood type and using immunosuppressive drugs. Xenotransplantation and stem cell research are new areas of study. Xenotransplantation is the use of animal organs for transplantation. This will help with the issue of whether a donor is truly dead or still alive when their organs are taken. Stem cell is the use of the cells from a developing embryo to create an organ. Stem cells are unspecialized and therefore, will avoid the problems of rejection and can easily be controlled to grow into any organ. The problem with this is ethnic controversy. A new way also is needed to test for rejection. The current method, the biopsy, is very accurate, but invasive and can only be used infrequently. The immune system consists of white blood cells and smaller proteins called antibodies. It is designed to attack foreign microbes to protect the body from viruses, bacteria, parasites, and fungi. The immune system first distinguishes the type of invader, then fights it and "remembers" how it fought the invader. The immune system recognizes the organs in its own body, supposedly not attacking itself. However, organ transplants are considered foreign bodies and are susceptible to rejection. Leukocytes, the white blood cells, challenge foreign bodies at the first stage of invasion. Lymphocytes develop into T-cells in the thymus, producing helper T cells, suppressor T cells, effector T cells, and natural killer cells. Helper and suppressor T cells control how the others fight the microbes. Effector T cells use enzymes to kill foreign bodies while natural killer T cells engulf and kill by phagocytosis. There are also B cells which mature into plasma cells and produce antibodies to kill. Antibodies bond to bonding sites on the antigens, preventing them to adhere to any surface and to affect any part of the body. Sepsis is the body's response to invasion of foreign bodies. Sepsis is dangerous when its effects lead to a state of excessive immunity or immune paralysis, the lack of iIIlI ll;unity to foreign bodies. Both lead to apoptosis and then major organ failure. The immune system is composed of a group of cells, molecules, and tissues help to defend the body against diseases and other harmful invaders is called immune system (Richmond, 2007). Immune system protect body from damaging substances invade the body. One of the key feature of the immune system is to destroy foreign invaders while leaving the body's own healthy tissue alone. When body has injury or infection, inflammation occurs. Inflammation causes redness, swelling, heat and pain. It could impair the function of the affected organ or tissue. The inflammation brings white blood cells called leukocytes, which are paI1 ofthe body's immune system, to the infected area. Inflammation with the immune system removes infectious organisms and begins healing. Leukocytes release chemicals called chemokines and cytokines to organize the body's inflammation response. Inflammation also occurs when the blood supply to an organ or tissue is interrupted. Sepsis begins with the recognizing of foreign bodies by toll-like receptors (TLR), especially TLR2 and TLR4. This triggers interleukin-I (IL-I), IL-6, and Tumor Necrosis Factor Alpha (TNFa), leading to the activation of aT-cell response and a cytokine release. Bacteria are usually the foreign bodies. When recognition receptors are exposed to bacterialligands or pathogen-associated molecular patterns (PAMPs), cascades are triggered that activate an immuno-response. The main role of sepsis-associated inflammation is to promote leukocyte transport to the site of infection. This causes local vasodilatation. This slows blood flow in the area and allows a larger volume of blood carrying leukocytes and cytokines to function in the infected area. The results of this response can be positive at first, but aftereffects may be deadly. Cytokines may cause vascular leakage of fluid due to damage to blood passageways. There may be hypoperfusion of tissue due to the focusing of blood in one area. A sudden drop in blood pressure can lead to organ failure. Damage to the endothelium may also lead to disseminated intravascular coagulation, which can be induced by triggering of receptors by triggers in pathogen cell walls and membranes or cytokines. This promotes thrombus and clot formation, leading to ischaemia, a deficiency of blood supply, and impaired perfusion to critical organs. The cytokine storm is a major cause of multiple organ dysfunction syndrome (MODS), which is in turn, a major cause of morbidity and mortality in intensive care units. It is the result of an acute inflammatory response. Expression of cytokine activity, upregulation of adhesion molecules in vascular areas, and density and potency of inflammatory cells in an area determine severity of organ dysfunction. MODS occurs in two phases: the Early Phase (First cytokine storm) and the Later Phase (Second cytokine storm). In the first phase, there is overproduction of inflammatory mediatories resulting in leukocyte and endothelial cell activation, increased endothelial permeability, and polymorphonuclear neutrophil (PMN) adhesion and migration. Cells in the spleen, liver, and bloodstream trigger the first cytokine storm. Initially, a release of cytokines interleukin-l Beta and Tumor necrosis factor alpha is triggered. Then adhesion of secondary inflammatory mediators is increased and cytokines, neurophil-generated reactive oxygen species (ROS), and cytolytic T lymphocytes contribute to an acute inflammatory response and induce endothelial damage. Damage is because of swelling, necrosis, and apoptosis. In the later stage, intrinsic inflammatory cells amplify inflammation. In organs with many lymphocytes and microphages, there are high concentrations of cytokines that trigger neutrophil infiltration. High concentrations of certain cytokines are also proven to be directly toxic to some parenchyma like the heart and skeletal muscle. After reentering the bloodstream, cytokines still may be dangerous if they activate intrinsic inflammatory cells in remote organs. The biopsy is a medical technique by which living tissue is obtained for examination under the microscope is call biopsy. A lot of information can be obtained through biopsy. It is usually used to diagnose disease or malfunction in tissues. When the tissue is examined under a microscope, it can be determined if the tumor is benign or malignant. The doctor bases on this information in order to determine how to complete the operation. The analysis of cells and tissues are important in determining the condition of the body. The examination is the study of cytology. The techniques preformed go under the category of a biopsy. For very delicate and protected organs, the excisional biopsy is needed, a surgical cutting of tissue. For larger biopsies, hospitalization, general anesthesia, and a period of recovery are needed. Firstly, and xray and then a CT scan are done in order to identify the problem region. The skin is cleaned by antiseptics and the surgical area is draped with sterile towels. Local anesthetic in injected directly under the skin, and then a second is injected deeper into the muscle so that the entrance area is numb. A catheder is inserted with either a clamp or needle at the end and is guided to the area of operation in the body. This is controlled using CT, ultrasound, and fluoroscopic guidance by radiologist and helpers. Cells are either sucked up by the needle or cut by the clamp (biotome). The tissue is placed on slides and sent to a pathologist. The operated area remains sore and black or blue for a short amount oftime where the tissue was damaged. There is a chance of excessive blood loss. The biopsy cannot be repeated for some time, is expensive, and invasive. Yet, it is currently the most accurate and efficient way for testing condition of organs. After cardiac transplantation, the goal of physicians is to prevent allograft rejection while minimizing immunosuppressive side effects. The current method of rejection surveillance is the endomycardial biopsy (EMB), which is invasive, expensive, subject to sampling error, interobserver variability (3-5) and has a morbidity rate of 0.5% to 1.5%. Deng et al. developed the AlloMap test based on recent studies that show that gene expression in peripheral blood mononuclear cells (PBMC) correlate to cardiac allograft rejection. 97 candidate genes in leukocytes were discovered to have some correlation with rejection. An additional 155 genes found to be related to the 97 genes were included in the gene set to test for rejection. Future research would include more extensive gene discovery using whole-genome-based array approaches, more specific analysis of pathways of specific genes during allograft rejection, and the role of AlloMap in other organ transplantations. The mitochondria are the powerhouse of the cell. They oxidize products of aytoplasmic metabolism to create the energy stored in adenosine triphosphate (ATP). Mitochondria also have the ability to synthesize their own proteins and lipids. They also have their own DNA (genetic material). The endosybiont hypothesis states that mitochondria may have evolved from bacteria into cells as a symbiotic relationship. Cells have provided mitochondria with a stable and safe environment and the mitochondria provide the cell with energy. If this is true, then studying the activity of the mitochondria can tell the activity of a cell by how much energy a mitochondrion produces. Smart et al. noticed that in higher plants, mitochondrial function must be developing to meet the respiration need of A TP. Mutations are the causes of many advancements in the structure f biological systems. However, mitochondrial function and gene expression pathways are new research and have not been looked into excessively. During meiosis in sunflower anthers, mitochondrial gene expression was characterized. The sunflower (H. annuus) was used for this experiment. Six stages of meiosis were identified and investigated. By the pachtene stage, abnormalities were detected in the meiocyte walls. Expression fthe atpA Locus and eMS phenotype was concluded. Expression begins at the tetrad stage. In conclusion, the mitochondrial genes were expressed in higher levels first in the meiocyte cells ofthe anther, then later, the tapetal cells. This shows that mitochondrial activity may show an impact on general cellular activity.