MHSCMP2029P2 - My Health Skills
advertisement
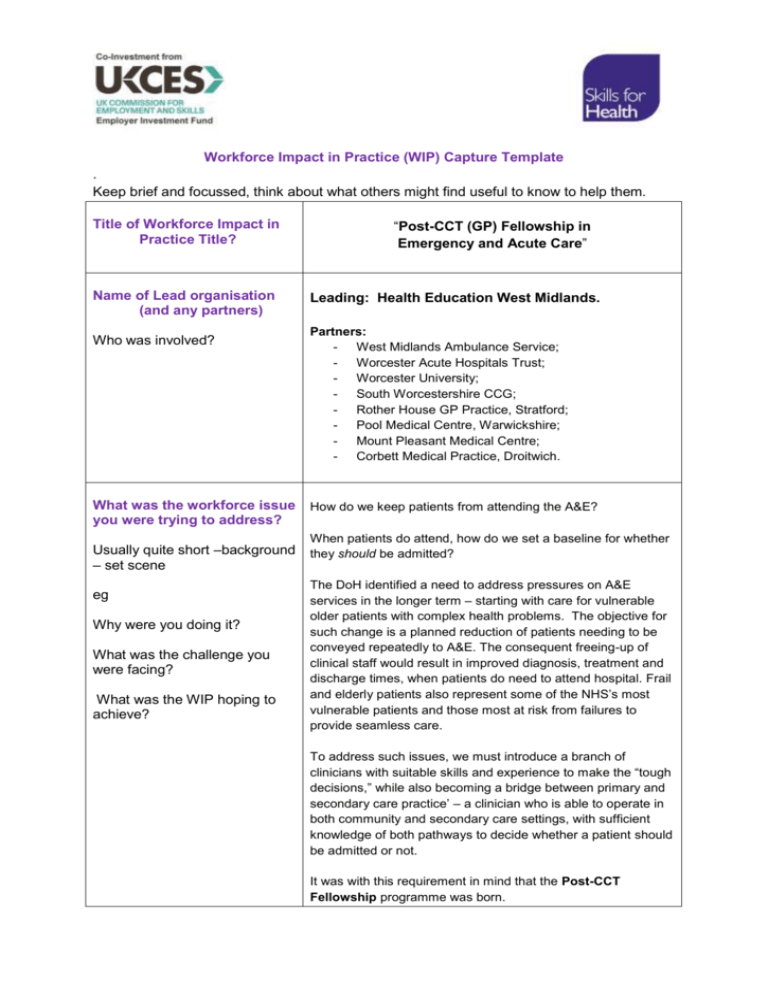
Workforce Impact in Practice (WIP) Capture Template . Keep brief and focussed, think about what others might find useful to know to help them. Title of Workforce Impact in Practice Title? Name of Lead organisation (and any partners) Who was involved? What was the workforce issue you were trying to address? Usually quite short –background – set scene eg Why were you doing it? What was the challenge you were facing? What was the WIP hoping to achieve? “Post-CCT (GP) Fellowship in Emergency and Acute Care” Leading: Health Education West Midlands. Partners: - West Midlands Ambulance Service; - Worcester Acute Hospitals Trust; - Worcester University; - South Worcestershire CCG; - Rother House GP Practice, Stratford; - Pool Medical Centre, Warwickshire; - Mount Pleasant Medical Centre; - Corbett Medical Practice, Droitwich. How do we keep patients from attending the A&E? When patients do attend, how do we set a baseline for whether they should be admitted? The DoH identified a need to address pressures on A&E services in the longer term – starting with care for vulnerable older patients with complex health problems. The objective for such change is a planned reduction of patients needing to be conveyed repeatedly to A&E. The consequent freeing-up of clinical staff would result in improved diagnosis, treatment and discharge times, when patients do need to attend hospital. Frail and elderly patients also represent some of the NHS’s most vulnerable patients and those most at risk from failures to provide seamless care. To address such issues, we must introduce a branch of clinicians with suitable skills and experience to make the “tough decisions,” while also becoming a bridge between primary and secondary care practice’ – a clinician who is able to operate in both community and secondary care settings, with sufficient knowledge of both pathways to decide whether a patient should be admitted or not. It was with this requirement in mind that the Post-CCT Fellowship programme was born. Why is this project required? - - - - - - A response to identified workforce shortages in secondary care. To reduce bed pressure by creating an effective path for triage and flow-through of patients presenting with complex co-morbidities. To understand the root causes of hospital referrals from primary care / community practice and develop strategies to avoid such referrals. To develop the role as a “safety net,” preventing unnecessary hospital admissions and re-invigorating community practice as first point of contact for patients. To allow the graduating fellow to practice equally as effectively in the Emergency Department, AMU, ambulance service or community GP Practice. To reduce costly Trust / Practice Locum spends and improve continuity of care / joined-up practice, by introducing a stable and consistent role. To follow the 2013 Hunt Recommendations for improving “joined up care, spanning GPs, social care, and A&E departments - overseen by a named GP.” The Fellowship will combine practical and didactic teaching over a twelve month period. The aim will be to create a GP practitioner who is confident in the diagnosis and treatment of patients presenting with acute and urgent conditions; conditions which would otherwise have been referred to hospital. How did you address this issue? How did you go about it? What was involved? The HEWM project team recognised that a multi-organisation team would be necessary to fully develop the model and provide a robust business case. The Project Manager brought together professionals from a range of potential user groups in Primary and Secondary care, forming a focussed and proactive project team. With input from all user groups, the Fellowship program was developed to include five distinct areas: 1) A secondary care placement in an Emergency Department (ED). 2) A secondary care placement in an Acute Medical Unit. 3) A placement period within the West Midlands Ambulance Service. 4) A “base” within a nominated GP practice, where the fellow will apply the experience gained in the secondary care phases of the Fellowship, to community medicine. 5) Collaborative working with Worcester University, to inform the development of a Post-Graduate Certificate in Emergency and Acute Care. A measure of success of this project will be that the Accreditation, clinical structures and pilot Fellows are of a standard fit for the purpose of training this first cohort. The GP Fellow will spend time on Emergency and Acute Medicine units, to gain experience in the providing of care for step-down patients in the community. There will also be time spent developing new and innovative processes for GPs to practice within their regional Ambulance Service, as well as other necessary aspects such as Paediatrics / care of acutely ill patients / end-of-life care. Optional question-Did you use any products or services to help you? Please feel free to share what you have used .If you have used Skills for Health products or services please explain. We want to see what ideas you have used Not used Skills for Health products for this project, but would consider using for future activities. What did you achieve? ie What happened? The Role Description went live in December 2013, receiving immediate support from the regional LETB, Health Education England, the Royal College of GPs, “First 5” GP group and AHSN. Such was the commercial relevance and potential of the role, that the three regional University Trusts have requested a further eighteen fellows (six each), to start in late 2014. To follow best practice, the project team elected to first use a pilot study to manage risk, identify and address practical “lessons” and “train the trainers,” in advance of a formal launch in September 2014. The September intake will be staggered into three, six-GP cohorts over a 12 month period. The pilot study commenced in January 2014, with three GPs recruited. The GPs are currently seconded to Redditch Alexandra ED, Worcester Royal Hospital AMU and West Midlands Ambulance Service (from March 3rd). The ED and AMU-based GPs are already forming plans for admissionsfocussed research work and liaising successfully with their nominated clinical supervisors, course director and GP Mentors. What was the WIPs impact? (Clear demonstration of impact of change .eg. the workforce, service delivery on patients/service users. Cost/quantity/quality, productivity, Return on Investment, staffing/clinical time saved, potential benefits. Data and any measures will be useful as will qualitative and and quantitative outcomes. A lack of qualified medical cover is identified as preventing patients from being discharged to community hospitals; the fellowship program will aim to address this by: - - Testing how the GP can effectively function within Emergency and Acute Medicine teams. Developing ways in which the GP can apply Emergency and Acute skills to support alternative care pathways in the community. Raising GP interest in Emergency Medicine career paths. Supporting and following the Hunt recommendations for improving “joined up care, spanning GPs, social care, and A&E departments - overseen by a named GP.” 1 In addition to their personal learning and development, Fellowship GPs will be expected to: - - - - Work with their host Practice and Health Education West Midlands to encourage other areas (regionally and nationally) to commission the fellowship. Develop an enhanced service locally, post-pilot. Develop ways in which a GP may respond to Emergency and Acute cases. Establish a working relationship with the ‘Virtual Ward’ model and explore models of care that offer viable alternatives to A&E admission. During practice attachments, offer direct contact by A&E staff. When patients of the host practice present at A&E with ambulatory or long-term care conditions, the Fellow will provide an assessment and management advice. Learn and enhance practical skills and interventions including: chest drains, reducing dislocations, suturing, cannulation and ultrasound use, as well as advanced life support courses and acute illness management in resuscitation. Learning outcomes for the GP Fellow will include: - - 1 To better understand the needs of patients, why they are attending A&E and how the GPs role could be adapted to improve A&E avoidance. To develop innovative ideas / share best practice of meeting the EM agenda in Primary care. https://www.gov.uk/government/news/hunt-nhs-must-fundamentally-change-to-solve-ae-problems Learning outcomes will be developed between the GP and their mentor, consistent with the operational requirements of their host and the following RCGP Curriculum guidelines: Hints and tips for others Share some of the things/insights that you think will help others trying to do the same sort of thing - Care of acutely ill people. Care of older adults. Care of children and young people. Care of people with Mental Health problems. Cardiovascular health. End of life care. Healthy People: Promoting health and preventing disease. - Crucial to success is developing a multi-organisation project team, representing the interests of all potential users. Recruiting fellows who share a desire to develop, innovate and push beyond traditional boundaries. Recognising that change starts with education of the individual. - What will you use the prize for? Please tell us how you would use the prize in your organisation In completing this template are you happy to share with the members of My Health Skills and Skills for Health Networks? Name and Contact details of person completing template To provide GP Fellows with a peer communication and information sharing resource, enabling cross-region sharing of best practice and innovation. Yes Name: Matt Aiello Title: Project Manager Organisation: Health Education West Midlands Address: St Chads Court, 213 Hagley Road, Edgbaston, Birmingham, B16 9RG Tel no: 07903 403 630 Email: matthew.aiello@wm.hee.nhs.uk Many thanks for completing this. Please return via email to myhealthskills@skillsforhealth.org.uk