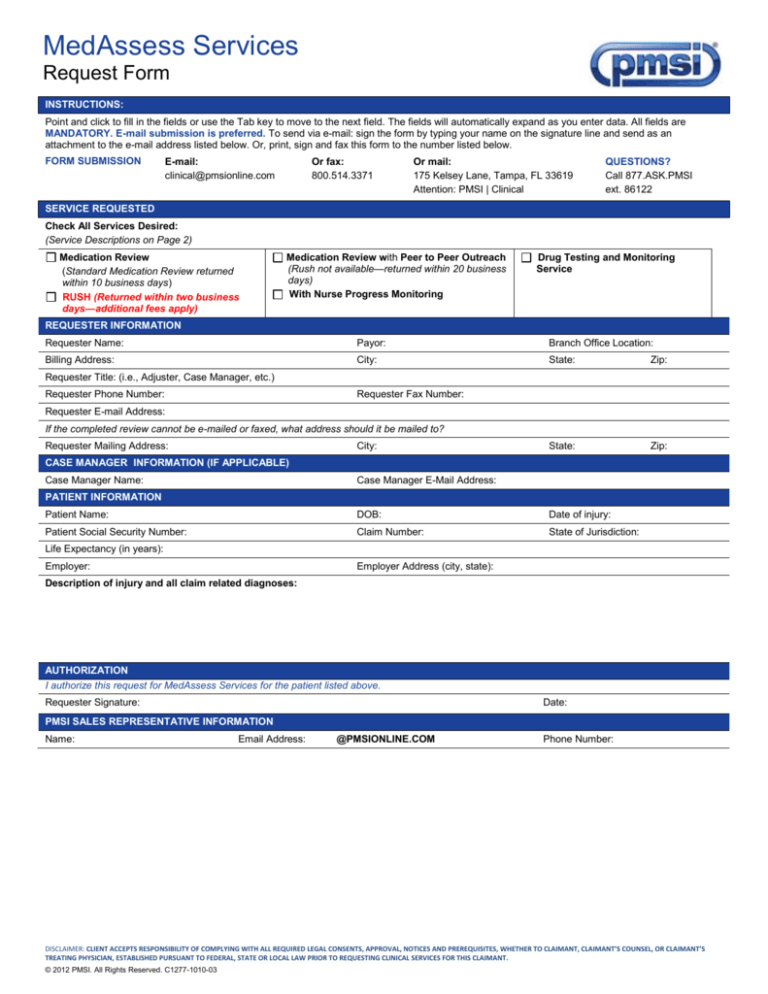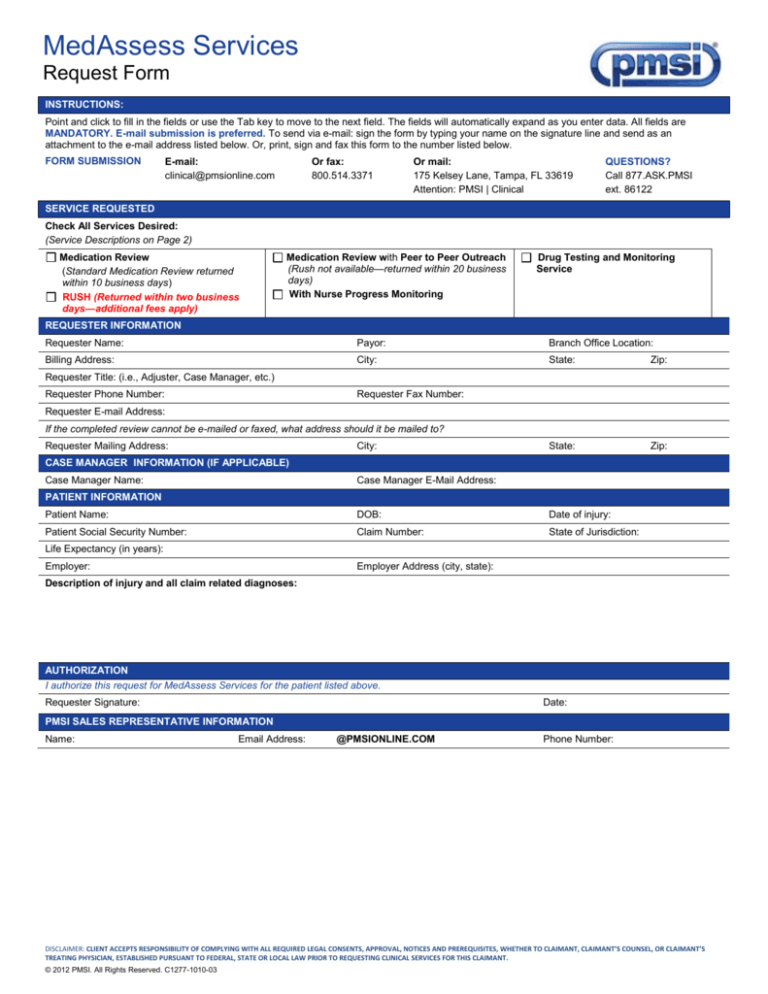
MedAssess Services
Request Form
INSTRUCTIONS:
Point and click to fill in the fields or use the Tab key to move to the next field. The fields will automatically expand as you enter data. All fields are
MANDATORY. E-mail submission is preferred. To send via e-mail: sign the form by typing your name on the signature line and send as an
attachment to the e-mail address listed below. Or, print, sign and fax this form to the number listed below.
FORM SUBMISSION
E-mail:
clinical@pmsionline.com
Or fax:
800.514.3371
Or mail:
175 Kelsey Lane, Tampa, FL 33619
Attention: PMSI | Clinical
QUESTIONS?
Call 877.ASK.PMSI
ext. 86122
SERVICE REQUESTED
Check All Services Desired:
(Service Descriptions on Page 2)
Medication Review
(Standard Medication Review returned
within 10 business days)
RUSH (Returned within two business
days—additional fees apply)
Medication Review with Peer to Peer Outreach
(Rush not available—returned within 20 business
days)
With Nurse Progress Monitoring
Drug Testing and Monitoring
Service
REQUESTER INFORMATION
Requester Name:
Payor:
Branch Office Location:
Billing Address:
City:
State:
Zip:
State:
Zip:
Requester Title: (i.e., Adjuster, Case Manager, etc.)
Requester Phone Number:
Requester Fax Number:
Requester E-mail Address:
If the completed review cannot be e-mailed or faxed, what address should it be mailed to?
Requester Mailing Address:
City:
CASE MANAGER INFORMATION (IF APPLICABLE)
Case Manager Name:
Case Manager E-Mail Address:
PATIENT INFORMATION
Patient Name:
DOB:
Date of injury:
Patient Social Security Number:
Claim Number:
State of Jurisdiction:
Life Expectancy (in years):
Employer:
Employer Address (city, state):
Description of injury and all claim related diagnoses:
AUTHORIZATION
I authorize this request for MedAssess Services for the patient listed above.
Date:
Requester Signature:
PMSI SALES REPRESENTATIVE INFORMATION
Name:
Email Address:
@PMSIONLINE.COM
Phone Number:
DISCLAIMER: CLIENT ACCEPTS RESPONSIBILITY OF COMPLYING WITH ALL REQUIRED LEGAL CONSENTS, APPROVAL, NOTICES AND PREREQUISITES, WHETHER TO CLAIMANT, CLAIMANT’S COUNSEL, OR CLAIMANT’S
TREATING PHYSICIAN, ESTABLISHED PURSUANT TO FEDERAL, STATE OR LOCAL LAW PRIOR TO REQUESTING CLINICAL SERVICES FOR THIS CLAIMANT.
© 2012 PMSI. All Rights Reserved. C1277-1010-03
Service
Description
Required Information
Fees
Medication Review
A Medication Review provides a
summary of the Clinical
Pharmacist’s findings from a
comprehensive review of the
injured worker’s prescription
medication record and medical
record. Specific clinical
recommendations regarding the
injured worker’s medication
therapy are included.
Twelve months of medical records from
the claimant’s prescribers is required
(office visit notes, discharge summary,
IME, etc.).
A standard fee will apply to
Medication Reviews. Payment is due
upon receipt of the completed
Review. Most reviews will be
completed within 10 business days of
receiving the completed request
/medical records .Final report will be
delivered via secure e-mail. If a delay
is anticipated, the requester will be
contacted.
Twelve consecutive months of
medication claims history is required
(the most recent transaction within six
months of the Review) and should
include:
Drug Name
Strength and Dosage Form
Quantity Dispensed
Dispense Date
Pharmacy Name
Prescriber First and Last Name
Patients utilizing PMSI Mail Order
Pharmacy or Tmesys® for pharmacy
services may already have complete
and up-to-date medication profiles on
file.
Medication Review requests for
claimants utilizing pharmacy services
outside of PMSI must be accompanied
by a medication claims history as
described above.
Same as Medication Review
Medication Review with Peerto-Peer Outreach
As follow-up to a Medication
Review, Peer to Peer Outreach
provides a telephonic meeting with
the treating prescriber(s) by a
specialist physician to review
therapy concerns and
recommendations from the
Medication Review in an attempt
to modify therapy.
Nurse Progress Monitoring
The Nurse Progress Monitoring is
a more intensive intervention
involving additional telephonic
interventions provided by a nurse
during the six months after the
Peer Outreach is performed. Upon
the completion of Peer Outreach, a
nurse reviews the case and
attempts initial contact with
prescriber. On a monthly basis, the
nurse will review the claimant’s
transaction history to determine if
changes to therapy have been
implemented and communicate
findings to the requestor.
Additionally, the nurse contacts the
prescriber before and after each
claimant’s appointments to discuss
any changes to therapy plan. At 6
months, a final report is generated.
Same as Medication Review with
Peer-to-peer Outreach
A standard fee will apply to the Nurse
Progress Monitoring
Drug Testing and Monitoring
Service
Enrolling an injured worker in the
service provides a Comprehensive
WC medication list to the
prescriber to assist in test
interpretation, monitoring of urine
drug tests, recommendations for
follow-up and outreach to the
prescriber and to the claims
adjustor, and a quarterly review of
all IW urine drug tests,
medications, prescribers, and
pharmacies with outreach to the
prescriber and the adjuster.
Name of urine drug testing lab used
by the client
A standard fee will apply to Drug
Testing and Monitoring.
Once PMSI receives an inconsistent
urine drug test from the client’s
laboratory of choice, the claimant
will be enrolled in the Drug Testing
and Monitoring Service
A standard fee will apply to
Medication Reviews with Peer-toPeer Outreach. Payment is due upon
receipt of the completed Review.
Most reviews will be completed within
20 business days of receiving the
completed request/medical records.
Final report will be delivered via
secure e-mail. If a delay is
anticipated, the requester will be
contacted.
Fees for urine drug tests are
negotiated by the client with their
urine drug testing laboratory of
choice and are the responsibility of
the client
DISCLAIMER: CLIENT ACCEPTS RESPONSIBILITY OF COMPLYING WITH ALL REQUIRED LEGAL CONSENTS, APPROVAL, NOTICES AND PREREQUISITES, WHETHER TO CLAIMANT, CLAIMANT’S COUNSEL, OR CLAIMANT’S
TREATING PHYSICIAN, ESTABLISHED PURSUANT TO FEDERAL, STATE OR LOCAL LAW PRIOR TO REQUESTING CLINICAL SERVICES FOR THIS CLAIMANT.
© 2012 PMSI. All Rights Reserved. C1277-1010-03