D2 East Induction Pack
advertisement

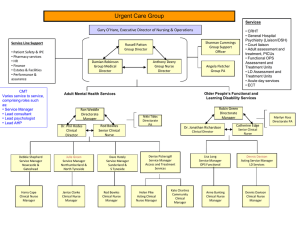
D2E STUDENT PACK The Royal Gwent Hospital We would like to welcome you to D2E. We hope to provide you with an enjoyable working environment. D2E Vision "Our aim is to provide high quality care to our patients and their relatives. We aim to provide a clean, organised and efficient department with happy, friendly and supportive staff" Introduction Welcome to D2E, the ward serves care of the elderly public living in South Gwent. D2E operates under the Directorate of Care of the Elderly (medicine). Our Directorate Manager is Rachel Cartwright and our Senior Nurse is David Timmins. The Ward Manager is Hannah Blackaby and Deputy Manager is Heidi Jones. Katie and Anne-Marie are our OTs who will assist you in facilitating safe discharges for our patients. The Unit based pharmacist is James and the technician is Dawn Ball. The Pharmacy team provide morning support and are a fantastic resource to the nursing staff. Afternoon cover is also sometimes provided but if there is no cover we can contact the pharmacy department. D2E consists of 21 beds male and female (however at any times can be made all female/male beds) depending on patient demand. We have three cubicles within the 21 beds. Our consultant is Dr Hedge and he has a supporting Holly Hanson CT2 And Farrah Fp2 Shift Pattern The Units shift pattern is 12 hour shifts, and but there may be occasions when the shifts have to be split into 6 hours to cover the demands of the service. All staff will be required to do internal rotation. The Daily Staff consists of Nurse in charge, three staff nurses and two NA’s. Night staff is two qualified staff and one NA. Admission Standard and Philosophy "Our aim is to provide high quality care to our patients and their relatives. We aim to provide a clean, organised and efficient department with happy, friendly and supportive staff" Admission Process Our patients are transferred via A&E and MAU acutely unwell and need 24-48 hr discharge plan that allows patient to return to their permanent residence within the community. With the assistance of OT and Physiotherapy and FOPAL services we aim for discharge on admission. These patients can often be unwell on arrival and will need regular observations. However once patient is stable and the nurse and doctor are happy the patient can go onto twice a day observations. As the patients are elderly we must continually assess waterlow scores and skin integrity, regularly updating risk assessments. Regular pressure relief should also be adhered to. There is great importance also in promoting independence with our patient’s e.g. if they are able to mobilise to the toilet with a Zimmer frame then help them to do so. Please do not use incontinence products unless patient is incontinent and only inserts to be used (not wrap around pads) when using incontinence products please ensure you have patients consent and full assessment has been made. Observations should be taken depending on patient’s definition. Always check with a qualified nurse prior to commencing shift to specify which patient’s need observation at what time interval. Patients awaiting social input i.e. care package and are medically fit need twice a day (BD) anyone scoring 3 or above on the news needs 1 hrly observations and acutely unwell patients need to be done every four hours. This can be established by the nurse each morning at start of shift. There are many learning opportunities for you e.g. OT , Outreach, Ward rounds, Complex discharge team, Frailty/Fopal team and we will help you with any other areas you wish to experience. I wish you well in your placement on D2E and if there is anything we can help you with please do not hesitate to contact us. Hannah & Heidi Ward rountine Handover and SPI takes place in the office. We handover in full in the office using PCR and MDT sheet At the start of each shift please ensure you sign in all the patients notes you will be looking after, clearly printing your name and position. All patients require observations to be taken a minimum of 6 hourly during the first 48 hours, more if triggering on NEWS. If stable after this period the qualified nurse may review the patient and reduce the observations to twice a day. We usually take observation at 0600, 1200 if needed, between 1600 & 1800 and at 2200. If any patients are scoring on the NEWS 3 or more or appear unwell please inform the qualified nurse straight away. NEWS 6 or above or a 3 in a red box needs reviewing by a doctor. Blood sugars are usually monitored at 0600 pre meals and at 2200. If the patient has unstable blood sugars or on a sliding scale this will be more frequently usually every 2 hours. If a patient has a blood sugar of less than 4mmol please inform qualified staff straight away. If a patient is at high risk of developing a pressure sore (bed sore) they will be on a skin bundle. These patients will need assistance to change their position every 4 hours. When repositioning patients it is important to check any areas at risk of damage such as sacrum, heels, elbows and any bony areas are checked and any damage (redness) documented and reported to the qualified nurse. When documenting in the patients notes we use the ICARE template, please see attachment. This needs to be completed every 2 hours. If you are having any difficulties please discuss with Sr Blackaby or Deputy Sr Jones. Quiet time is between 13:30 and 15:00, during which time we dim the lights so patients can have a rest. This is a good opportunity to complete the daily cleaning. Please don’t forget to sign the cleaning rota once completed. Please familiarise yourself with the documentation i.e. NEWS, insulin charts, skin bundles etc. We hope this is helpful if you have any further questions please ask. Checklist- (you will receive training on each) Resus trolley and emergency buzzers Staff toilet Cleaning scheldules PSAG board Employee on line access Abreviations for handover! SOB - shortness of breath CABG – Coronary heart bypass graft IHD – ischaemic heart disease CHD – coronary heart disease TYPE 2 DIABETIC – diabetic – diet controlled or tablet controlled can also be on insulin TYPE 1 DIABETIC – diabetic on insulin SVD – small vessel disease – a diagnosis from CT usually age related damage AF – atrial fibrillation – an irregular heartbeat which is high risk of throwing of a clot from the heart. The blood can pool as the heart is not beating regularly. This is why patients are given blood thinners such as warfarin. Patient’s taking warfarin are VERY high risk of bleeding. NSTEMI – Non ST elevation myocardial infarction (heart attack that doesn’t show on ECG) STEMI – ST elevation myocardial infarction (heart attack that shows on ECG changes MI – heart attack STENT – a procedure to open arteries in the heart, liver any organ that has a blockage CVA – stroke GORD – reflux COPD – chronic obstructive pulmonary disorder also known as COAD (A-airway) HYPERTENSION – high blood pressure CCF – heart failure also known as heart failure CKD – chronic kidney disease (there are different stages of kidney disease which is referred to as 1,2,3 and 4 UTI – urine infection CIWA – alcohol withdrawal treatment using diazepam every 90 minutes to dampen symptoms MFFD – medically fit for discharge (usually awaiting social input) TROP (TROPONIN) – a cardiac enzyme taken in the blood to show heart muscle damage MDT – a meeting for all staff and family to discuss the best way socially for a patient’s transfer/discharge BIM – best interest meeting (designed for patient’s that don’t have capacity to make a decision for their own best interest LRTI – chest infection GI Bleed – an internal bleed generally from the gastrointestinal tract (stomach, bowel, oesophageal) LTOT – long term oxygen therapy (home oxygen) SEPSIS – when infection has gone widespread and starts to effect organs POC – package of care BD – twice a day QDS – four times a day TDS – three times a day ANGIO – angiogram (a catheter is put into an artery with a camera to observe any blockages in the heart) ECHO – echocardiogram – a ultra sound scan of the heart ASPIRATION – when somebody has taken food or drink and it has gone into the lungs e.g delayed swallow PT – physio OT – occupational therapy DKA – Diabetic ketoacidosis (when blood sugars are irratic and the body starts to produce ketones, this then causes the blood to become to acidic) Patient’s that have this need regular blood sugars and ketones. PLEURAL EFFUSION – a collection of fluid in the lung PE – a clot of blood in the lung DVT – a clot in a vessel ALD – alcoholic liver disease LIVER CIRRHOSIS – liver damage COMPLEX DISCHARGE – discharge is going to be difficult without involvement of social services e.g needs a package of care INFARCT – death of muscle, cells etc AKI – acute kidney injury DIABETIC – need 4x day BM for insulin (morning, lunchtime, teatime and bedtime) need 2 x day BM for tablet controlled need once a day BM for diet controlled sliding scale need hourly BM KIDNEY INJURY – 1 hourly urine monitoring and input and output chart updated strictly