Sample Protocol: Cytogenomic Microarray Data ONLY
advertisement
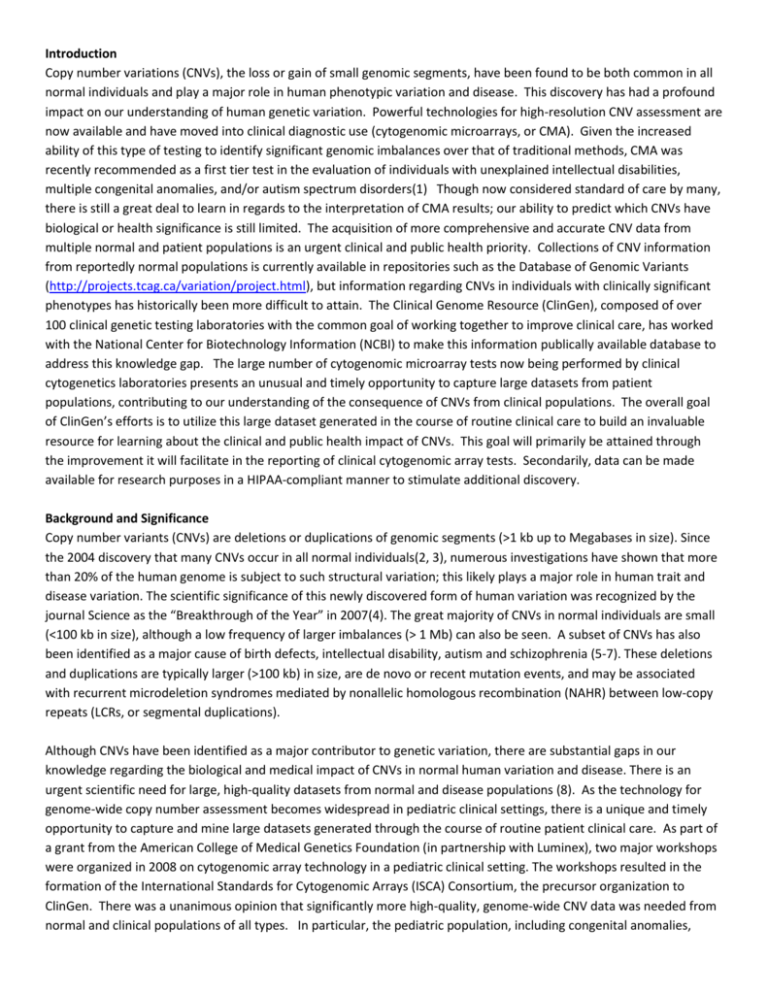
Introduction Copy number variations (CNVs), the loss or gain of small genomic segments, have been found to be both common in all normal individuals and play a major role in human phenotypic variation and disease. This discovery has had a profound impact on our understanding of human genetic variation. Powerful technologies for high-resolution CNV assessment are now available and have moved into clinical diagnostic use (cytogenomic microarrays, or CMA). Given the increased ability of this type of testing to identify significant genomic imbalances over that of traditional methods, CMA was recently recommended as a first tier test in the evaluation of individuals with unexplained intellectual disabilities, multiple congenital anomalies, and/or autism spectrum disorders(1) Though now considered standard of care by many, there is still a great deal to learn in regards to the interpretation of CMA results; our ability to predict which CNVs have biological or health significance is still limited. The acquisition of more comprehensive and accurate CNV data from multiple normal and patient populations is an urgent clinical and public health priority. Collections of CNV information from reportedly normal populations is currently available in repositories such as the Database of Genomic Variants (http://projects.tcag.ca/variation/project.html), but information regarding CNVs in individuals with clinically significant phenotypes has historically been more difficult to attain. The Clinical Genome Resource (ClinGen), composed of over 100 clinical genetic testing laboratories with the common goal of working together to improve clinical care, has worked with the National Center for Biotechnology Information (NCBI) to make this information publically available database to address this knowledge gap. The large number of cytogenomic microarray tests now being performed by clinical cytogenetics laboratories presents an unusual and timely opportunity to capture large datasets from patient populations, contributing to our understanding of the consequence of CNVs from clinical populations. The overall goal of ClinGen’s efforts is to utilize this large dataset generated in the course of routine clinical care to build an invaluable resource for learning about the clinical and public health impact of CNVs. This goal will primarily be attained through the improvement it will facilitate in the reporting of clinical cytogenomic array tests. Secondarily, data can be made available for research purposes in a HIPAA-compliant manner to stimulate additional discovery. Background and Significance Copy number variants (CNVs) are deletions or duplications of genomic segments (>1 kb up to Megabases in size). Since the 2004 discovery that many CNVs occur in all normal individuals(2, 3), numerous investigations have shown that more than 20% of the human genome is subject to such structural variation; this likely plays a major role in human trait and disease variation. The scientific significance of this newly discovered form of human variation was recognized by the journal Science as the “Breakthrough of the Year” in 2007(4). The great majority of CNVs in normal individuals are small (<100 kb in size), although a low frequency of larger imbalances (> 1 Mb) can also be seen. A subset of CNVs has also been identified as a major cause of birth defects, intellectual disability, autism and schizophrenia (5-7). These deletions and duplications are typically larger (>100 kb) in size, are de novo or recent mutation events, and may be associated with recurrent microdeletion syndromes mediated by nonallelic homologous recombination (NAHR) between low-copy repeats (LCRs, or segmental duplications). Although CNVs have been identified as a major contributor to genetic variation, there are substantial gaps in our knowledge regarding the biological and medical impact of CNVs in normal human variation and disease. There is an urgent scientific need for large, high-quality datasets from normal and disease populations (8). As the technology for genome-wide copy number assessment becomes widespread in pediatric clinical settings, there is a unique and timely opportunity to capture and mine large datasets generated through the course of routine patient clinical care. As part of a grant from the American College of Medical Genetics Foundation (in partnership with Luminex), two major workshops were organized in 2008 on cytogenomic array technology in a pediatric clinical setting. The workshops resulted in the formation of the International Standards for Cytogenomic Arrays (ISCA) Consortium, the precursor organization to ClinGen. There was a unanimous opinion that significantly more high-quality, genome-wide CNV data was needed from normal and clinical populations of all types. In particular, the pediatric population, including congenital anomalies, intellectual disabilities, and autism, was thought to be a very important population in which to gain an understanding of pathogenic CNVs in the human population as a whole. Approximately 3% of all children are born with a major congenital abnormality or significant developmental disability (e.g., developmental delay, intellectual disability, autism, epilepsy). The primary genetic laboratory test for this group of children has been the G-banded karyotype, capable of detecting deletions, duplications or other rearrangements of ~510 Mb in size. The yield of standard karyotype analysis is ~3% (excluding Down syndrome and other easily recognizable chromosomal syndromes); recent studies with cytogenomic array technologies have demonstrated a yield of almost 1520% in the same pediatric populations, greatly increasing the number of children and families who benefit from a precise diagnosis, improved prognostic information, and accurate genetic counseling regarding recurrence risks(9). As such, CMA is now considered a first-tier diagnostic test in the evaluation of individuals with unexplained intellectual disability, multiple congenital anomalies, and/or autism spectrum disorders(1). Since several hundred thousand cytogenetic studies are performed each year on a clinical basis, the potential dataset size from clinical studies in the U.S. is quite large. Capturing this data from clinical laboratories presents a unique opportunity to collect and mine the large datasets generated through the course of routine patient care. To do this, ClinGen supports the development of a publically available database, ClinVar (housed within the National Center for Biotechnology Information (NCBI) within the National Institute of Health (NIH)), in which clinical laboratories from around the world deposit deidentified CNVs found during routine clinical CMA testing. The advantages of obtaining data from clinical testing centers through a coordinated multi-centered approach include 1) reduced costs, as the array data is already generated as part of patient care; 2) access to large numbers of samples; tens of thousands of cytogenomic array cases are currently being done on a clinical basis; and 3) pooling data across many clinical labs will rapidly accelerate our understanding of pathogenic vs. benign CNVs in the human genome. A multi-centered collaboration is now practical since all technologies provide genome-wide data with imbalances defined and reported in the universal language of human genome sequence coordinates. Our limited knowledge regarding the potential clinical impact of CNVs currently causes substantial uncertainty in both pediatric and prenatal settings in regards to interpretation of lab results. It is difficult to effectively counsel families regarding the potential causal relationship of CNV to disease phenotype when little information is available about the particular CNV. A large, centralized database of genotype and phenotype information will greatly accelerate our ability to interpret CNV findings, and will be invaluable in improving patient care. High-quality data is released publicly on an ongoing basis through public genome browsers and commercial vendors, with efforts to develop “clinician-friendly” user interfaces to search for data on cases similar to their own patients. Both patients and society will benefit from the knowledge obtained from this project. Improved counseling based on more precise information will be possible for patients, and clinicians will be able to describe the spectrum of anticipated impact with increased precision. Most importantly, detailed information about the etiology of specific developmental disorders should lead to the adoption of the most appropriate treatment approaches. This information will also allow for the most appropriate use of these technologies in prenatal testing. Experience from other currently participating clinical laboratories demonstrates that it is feasible and desirable for clinical labs to submit array data to the ClinGen project. As a central repository for genotype and phenotype data, these very large datasets from clinical cytogenetics laboratories are initially received in dbGaP (the database of Genotypes and Phenotypes at NCBI/NIH), where scientific definition checks are performed and summary tables prepared. A process for expert curation is in development for further data quality improvement, and public data releases of the data into ClinVar and other NCBI resources are made on a quarterly basis. Development of “clinician-friendly” web portals and tools to visualize and search this large dataset will greatly enhance the ability to determine the clinical significance of any individual CNV and will be a rapidly improving tool in clinical decision-making. Study Design Methods This study is designed as an international, publically available database. Sample Subjects will be identified if their physician orders cytogenomic microarray testing at XXX Laboratory. Sample size at this center will be commiserate with the number of CMA tests we perform per year, which is approximately XXX (# of males, # of females), ages 0-100 years. Currently, the ISCA Clinical CNV database has information on over 30,000 cases. The ordering physician or genetic counselor will be the person primarily responsible for informing the patient of the laboratory’s participation in the ClinGen project. The laboratory will be contacting each clinician who orders testing routinely to discuss this new database, provide resources, and answer any questions. It will also be discussed when communicating equivocal or abnormal test results by phone as part of standard laboratory practice. Information about the database and how an individual can opt-out of participation will be included anywhere information about cytogenomic array testing is available: test requisition forms and systems, test reports, and laboratory websites. Inclusion Criteria: Any individual who has clinical cytogenomic array testing through the XXX Cytogenetics Laboratory. Exclusion Criteria: None Research Procedures Design of ClinGen Project: Geisinger Health System serves as one of the coordinating center for the ClinGen Project; the project in its entirety has been approved by the IRB of Geisinger Health System (IRB #2013-0367). NCBI Collection of Data into dbVar: The data submitted to the project will be hosted by NCBI at the NIH. The database will collect two types of data: 1. Retrospective data (CNV calls only): This type of data will consist of the phenotypic information supplied to the laboratory at the time of testing, as well as the CNVs reported in the clinical report. The CNVs will be described by genomic location and clinical significance as determined by the submitting laboratory (i.e. pathogenic, benign, uncertain, etc.). Information will also be collected regarding the inheritance of each CNV (i.e. maternally inherited, paternally inherited, de novo), if available. If additional CNVs were present for an individual (though not reported clinically) this will be indicated by an asterisk, but these additional findings will not be available. Raw data will not be accessible. All information will be completely deidentified. This type of “calls-only” data is stored in the publically accessible dbVar – database of Genomic Structural Variation (through NCBI/NIH) (http://www.ncbi.nlm.nih.gov/dbvar/studies/nstd37/). Curated data will also be made available through ClinVar (http://www.ncbi.nlm.nih.gov/clinvar/). 2. Prospective data (CNV calls AND raw data files): This type of data will consist of the CNV call data described above as well as de-identified raw data files generated in the course of clinical testing. Cases with raw data files available are stored in the controlled-access dbGaP (http://www.ncbi.nlm.nih.gov/projects/gap/cgibin/study.cgi?study_id=phs000205.v2.p1); the CNV call information is also stored in dbVar and, if curated, in ClinVar, as above. Controlled-Access data from dbGaP may be made available to researchers after they receive appropriate authorization. Researchers are required to submit all research intentions and protocols to a Data Access Committee (DAC), which is responsible for considering and approving access based on research protocols and the consent processes in place for them. Data available at the Controlled-Access level will still be de-identified but raw data will be available. We are seeking IRB approval to contribute both retrospective (cases performed through our laboratory PRIOR to the initiation of opt-out consent, as described below) AND prospective limited datasets (cases performed through our laboratory AFTER the initiation of opt-out consent) generated through routine clinical care to this database. We are also requesting a letter of certification be sent to the NIH as assurance that this approval has been granted. A sample letter of certification has been provided (see supporting documents). De-identification of Data: Although this is not a GWAS database, the ISCA Consortium is following the guidelines for de-identification of data outlined by NIH Points to Consider (see supporting documents). All HIPAA-identifiers will be removed from the data before submission. The laboratory will code all results with a Submission ID before sending data to NCBI. This Submission ID will not be the patient accession number or laboratory ID used for clinical testing. NCBI will then re-code the data with a separate ID so that the testing laboratory will also be de-identified. The laboratory alone will retain the key linking the codes to the complete clinical file that is maintained as part of the routine clinical care provided. Privacy procedures consistent with standard clinical care, including password-protected computers, locked files, and HIPAAtrained staff, will be upheld at all times. The repository staff and secondary data users will not be able to identify the patient or the ordering physician in any way. Additionally, we are requesting that a letter of certification be sent by the IRB to the NIH as assurance that we are complying with these recommendations. A sample letter has been provided (see supporting documents). Data Submission: The following schematic provides a general outline of how the datasets from the contributing laboratories will be curated and deposited into the database. ClinGen Workgroups are standardizing the formats and definitions of the contribution of genotypic and phenotypic data. Genotypic data derived from cytogenomic array studies includes information on chromosomal gains and losses, many of which are surprisingly common in the general population. The nature of this data is clearly distinct from data generated through genome-wide association studies (GWAS) and does not pose the same risk of re-identification. It is important to note that the ISCA Clinical CNV Database is not a GWAS database. Phenotypic data contributed to the database will be the information provided to the laboratory by the referring physician. While one of the goals of the database is to improve our understanding of genotype-phenotype relationships, we will not be providing highly-detailed phenotype information. Generally, the information we are provided with is a general description such as developmental delay, seizures, or heart defect. There would not be enough detailed phenotypic information available through this database to ever re-identify an individual. To further generalize the phenotype information deposited in the ISCA Clinical CNV Database, all phenotype information will be converted into specific Human Phenotype Ontology (HPO) terms(10). Data will be deposited from YOUR LAB’S NAME on a routine basis to NCBI. No patient-identifiers will ever accompany the data. Additionally, no biological specimens will be shared in any way. The following schematic is provided to help illustrate the process of data submission. In Physician Practice Patient Physician Order test (Opt-out information discussed) In Testing Lab RESULTS: Perform aCGH test POSITIVE (Contact physician, discuss results and opt-out) Opt-Out? NEGATIVE (Report includes opt-out information) YES No data deposited NO Deposit data At NCBI CNV Atlas of Human Development Data Analysis Data will consist of deidentified CNVs identified during the course of routine clinical cytogenomic testing, their clinical interpretations (benign, pathogenic, etc.), and phenotype information generalized to HPO codes. This data is stored within a publically available database, dbVar, maintained by NCBI and the NIH. Any additional deidentified raw data files that are collected as part of this study are maintained in a controlled-access database, dbGaP, maintained by NCBI and the NIH. Researchers with an IRB-approved protocol may apply for access to the data in dbGaP; a separate Data Access Committee within NCBI reviews these applications and grants access as appropriate. The intent of this database is to serve as an ongoing resource to both the clinical and research communities. No specific data analysis is planned. Periodically, the data may be summarized by ClinGen using descriptive measures (i.e. how many pathogenic CNVs have been identified amongst patients referred for autism). Simple comparative statistics may also be used (i.e. has a particular CNV been classified as “pathogenic” a statistically significant number of times more than it has been called “uncertain,” etc.). Independent researchers who utilize the data are responsible for conducting their own analyses. Adverse Events and Data Monitoring Committee As no interventions are taking place, no adverse events are anticipated. The risk that an individual could be identified by the data reported to this database is low. Should an adverse event occur, it will be recorded and reported to the IRB per standard procedures. A Data Monitoring Committee will not be used, as there are no anticipated risks to patient safety. Consent “Opt-Out” Model: A waiver of elements of informed consent is being requested for this study for the following reasons: 1. The research involves no more than minimal risk. The risk that a person could be identified by the information being submitted to the database is low. There are no other anticipated risks associated with participation in this study. 2. Waiving full informed consent is not believed to adversely affect the rights or welfare of the study participants. 3. Information will be provided to the study participants through the laboratory test requisition form, test results, and laboratory website as described below. 4. This study could not feasibly take place without waiver of informed consent. The laboratory provides cytogenomic array testing to a large volume of patients (about xxx in [previous year]). The laboratory is not always provided with patients’ personal contact information. Because of this, it would not be feasible to contact each patient and obtain a traditional signed informed consent form prior to participation. This barrier to the collection of large datasets has been recognized by the NIH and an “opt-out” model has been developed as a way to insure that patients are aware of the laboratory’s participation in the ClinGen project and are given the option to have their data removed from the database. This “opt-out” model was developed by the Collaboration, Education, and Test Translation (CETT) Program, sponsored by the NIH Office of Rare Diseases Research and has been successfully utilized to improve clinical testing for a number of genetic conditions (Cornelia de Lange syndrome, autosomal recessive microcephaly, Cherubism, epimerase deficiency, Joubert syndrome, primary ciliary dyskinesia, and more). The process of “opt-out” was discussed with multiple privacy experts at NIH and accepted as reasonable as long as information about the process and information about how to remove one’s data were provided to clinicians and patients and families. In compliance with this model, information about opting-out will be provided in multiple locations including 1) clinical laboratory websites, 2) test ordering materials 3) test reports, and 4) a supplemental information flyer made available to the ordering physician to discuss before ordering testing and while providing test results. These materials are provided for review. There are multiple ways a patient can communicate with the laboratory to opt-out of participation: 1) A box will be provided on the test requisition form and the patient can request that this be checked if he or she would like to opt-out. 2) Each cytogenomic array test report will include a box that the patient can check if requesting to opt-out and the report can be faxed to the laboratory. A toll-free fax number is available. 3) Patients can call the laboratory and speak to a genetic counselor about opting-out. A toll-free phone number is available. Possible Recontact for Research: The primary purpose of ClinGen is to improve clinical care by providing a resource to laboratories and clinicians to improve cytogenomic array testing, genetic counseling, and patient care management. However, upon approval by a Data Access Committee, researchers may request that a patient be informed of their specific research project and have the opportunity to participate. Separate IRB-approval at the researcher’s institution would be required. If this approval is granted, the researcher would be allowed to contact the laboratory to make this request. The laboratory would determine if this request is reasonable and appropriate and could decide to contact the ordering physician to discuss. The ordering physician would also then determine if this request seems reasonable and appropriate and could decide to pass on the researcher’s contact information to the patient. The patient would then be able to contact the researcher directly if he or she is interested in participating or to obtain additional information about the study. Full informed consent would be obtained for such studies by the research team. At no time will any researchers have access to patient or ordering physician contact information. This model provides two additional opportunities (the laboratory and the physician) to screen the research protocol proposed and to determine if it is appropriate to share with a patient or family. Researchers will not be permitted to request DNA or other specimen retained in the laboratory after clinical testing is completed for any patient. Furthermore, we anticipate that the individuals or families who may be of interest to a researcher at some time in the future would be the patients with equivocal or abnormal cytogenomic array results, rather than a patient with a normal result. Patient advocacy groups who provided input to the CETT Program have shared that the majority of these families welcome such contact and may be seeking out such opportunities to participate in research. The following schematic is provided to help illustrate the process for a request by a researcher. In Physician Practice NO No further action Patient/family chooses to participate NO No further action Physician review YES Contacts Researcher In Testing Lab YES Send Researcher’s information to Physician NO No contact Request contact with Physician Lab Review At NCBI Submit request to DAC DENIED No data released Researcher GRANTED Data made available References 1. Manning M, Hudgins L. Array-based technology and recommendations for utilization in medical genetics practice for detection of chromosomal abnormalities. Genet Med 2010: 12: 742-745. 2. Sebat J, Lakshmi B, Troge J et al. Large-scale copy number polymorphism in the human genome. Science 2004: 305: 525-528. 3. Iafrate AJ, Feuk L, Rivera MN et al. Detection of large-scale variation in the human genome. Nat Genet 2004: 36: 949-951. 4. Pennisi E. Breakthrough of the year. Human genetic variation. Science 2007: 318: 1842-1843. 5. Sebat J, Lakshmi B, Malhotra D et al. Strong association of de novo copy number mutations with autism. Science 2007: 316: 445-449. 6. Cook EH, Jr., Scherer SW. Copy-number variations associated with neuropsychiatric conditions. Nature 2008: 455: 919-923. 7. Baldwin EL, Lee JY, Blake DM et al. Enhanced detection of clinically relevant genomic imbalances using a targeted plus whole genome oligonucleotide microarray. Genet Med 2008: 10: 415-429. 8. Itsara A, Cooper GM, Baker C et al. Population analysis of large copy number variants and hotspots of human genetic disease. Am J Hum Genet 2009: 84: 148-161. 9. Miller DT, Adam MP, Aradhya S et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet 2010: 86: 749764. 10. Robinson PN, Kohler S, Bauer S et al. The Human Phenotype Ontology: a tool for annotating and analyzing human hereditary disease. Am J Hum Genet 2008: 83: 610-615.