Autonomics_02
advertisement

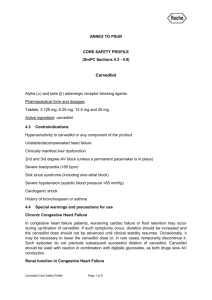
Autonomic Pharmacology II. Cardiovascular System. Trachte. 9.28.09. Katelyn Rogers. Sketch Biosynthesis of Catecholamines Pathways & Locations: amphetamine, Sketch: normetanephrine, catecholamines, ephedrine Sketch Slide 5: Sympathetics NTs: Adrenergic Amines Synthesis Storage Release Termination Receptors Drugs/Catecholamines Tyrosine Hydroxylase (cyto) is ratelimiting – blocked by -methyl tyrosine. In granules w/ ATP Normal: -Release of Dopamine beta-hydroxylase, NE & ATP (lose protein) -induced by stimulation of Nic rec depol (Na+ influx) & Ca2+ influx. -NE inhibs own release – 2-NEG FEEDBACK SYST. Removal: -uptake -dilution & diffusion -degradation: COMTcyto or MAOmito 1 EpiNE>>isoproterenol Indirectly-acting sympathomimetics: -Release of NE. -Tachyphylaxis (desens) – can amt released. -TYRAMINE, AMPHETAMINE, EPHEDRINE -Reverse direction of axoplasmic transporter -Inactive when+ IMIPRAMINE or COCAINE (drugs that inhib the axoplasmic pump symp) PARGYLINE (MAOi) EPINEPHRINE: Vasoconstricts (1), can vasodilate (2), directly HR & F, but reflex suppresses HR. Contraind: hyperthyroidism, HTN Tx: hypersens (BP & bronchospasm), w/ anesthetics vasocons prevents diffusion. NOREPINEPHRINE: Vasoconstricts (1), HR & F (1), but reflex suppresses HR. Contraind: Hyperthyroidism, anesthesia, pregnancy Tx: HypoT, shock. ISOPROTERENOL: Vasodilates (2) & tachycardia (1). Only COMT met! Tx: cardiac stimulant. PNMT is confined to adr med (may be in brain & vesicle). Enzymes are non-specific. Dihydroxyph enylserine can be converted to NE by DOPA Axoplasmi c uptake (1/5) Granular uptake (4/5) RESERPINE: inhibs granular pump catecholamines in vesicles (results in depletion of them) –depression/suicidal GUANETHIDINE: induce release from vesicle, Inactivation: Vanillylmandelic acid is predominant urinary product. Normetanephrine is next. 2 EpiNE>>isoproterenol prejxnal nerve terminal, platelets, gut, med-obl – site of action. 1 isoproterenol>Epi=NE in heart, JG apparatus, fat 2 isoproterenol>Epi>>NE hyperglycemia is best stimulus Dopamingergic rec + DA Dilates renal/mesenteric vasc. (for shock) Sketch receptors on the Non-catecholamines, sympathomimetics Are phenyethylamines that are indirectly acting (release NE from nerves by reversing the axoplasmic pump) that distribute even into the brain. Only MAO met! AMPHETAMINE: release NE from nerves, BP (1) Toxicity: tachycardia & hyperthermia Tx: narcolepsy, hyperkinetic synd, obesity. EPHEDRINE: releases NE & has direct effects (BP/vasocons)-1 &1 & vasodilates (2) & less of an affect on CNS). slow acting, depletes NE stores, resp to symp stim, inactive when + PARGYLINE (MAOi) or inhibitors of axoplasmic transporters (COCAINE) both leading to symp. For PARGYLINE avoid foods w/ TYRAMINE or could lead to HTN crisis. decarboxylas e. following eqn: BP= HR x SV x TPR Those on top inc BP, those on bottom dec BP. Vascular effects always win over heart effects, bc of r4! DOPAMINE: F (1), vasodilator in renal & mesenteric vasc at low doses (dopaminergic), vasoconstricts at higher doses (1). DOBUTAMINE: “Do b #1” Selective B1 agonist, F Contraind: A Fib Tx: Emergency only for CHF/MI Toxicity: ~ to combo of Epi & Amph. Tx:Cold Meds PSEUDOEPHEDRINE: Tx: Nasal congestion Sympathetic Receptors & Drugs that Act Upon Them: receptors receptors Non-selective Agonists: EPINEPHRINE NOREPINEPHRINE Non-selective Agonists: ISOPROTERENOL EPINEPHRINE Non-selective Antagonists: Mech: Block 1 rec leading to TPR & BP & block 2 rec to NE release from nerves ( tachycardia) Actions: HypoT, Bld Flow, mucosal stiffness Side effects: postural hypoT (blocks venoconst), nasal stiffness, tachycardia (BP is caused by need to HR (ie. Turn on symp) and the BP does this reflexively + NE release). PHENTOLAMINE Comp inhib of & SE rec Tx: Pheochromocytoma, shock, hypertensive crisis w/ MAOis. PHENOXYBENZAMINE: Noncomp inhib of -rec (irreversible binding – shifting dose resp curve down) Non-selective Antagonists: Mech: Comp blockade of 1 & 2 in the system & braindepr. Actions: HR (1) & Epi-induced vasocons (2)CO. Prevents Epi-induced hyperglycemia (2)-dangerous in diabetics. airway R (2)- dangerous in asthmatics. Renin release (1) Q. If you take a drug and have an asthmatic attack, what drug is it? It is a -blocker. Absorption/Tx: oral, metabolized first pass liver. HTN – by CO, angina, arrythmias, pheochromocytoma-induced tachycardia, hyperthyroidism, migraine prophylaxis, MI, glaucoma, CHF (blocks actions of catecholamines giving beneficial effect over long term, not acute). Side effects: Bradycardia (1), bronchoconstriction (2), vasopasm in Raynaud’s (2), sex dysfxn, depression (NOT ATENOLOL), blocks hyperglycemic resp to Epi (2)- too much insulin, can’t crank glucose up, in vasculature Epi-induced contractions (2). PROPRANOLOL Not used for glaucoma. Tx: Angina, arrhythmias, HTN. TIMOLOL Tx: HTN, MI, Wide angle glaucoma (aq humor formation) PINDOLOL Tx: HTN Partial agonist less bradycardia LABETALOL 1 & antagonist Tx: pheochromocytoma, HTN, & CLONIDINE withdrawal. Side effect: MORE ORTHOSTATIC HYPOTENSION CARVEDILOL -blocker & 1-antagonist Tx: milder forms of CHF & HTN 1 2 1 2 Agonists Antagonists Agonists Antagonists Agonists Antagonists Agonist DOPAMINE (at high doses) ANTIHYPERTENSIVE Mech: Block 1 rec to TPR & BP. CLONIDINE “we’re clowing around us 2.” -METHYLDOPA (converted to methyl-NE by DA-- ANTIHYPERTENSIVE No essential ones! Yohimbine approved clinically. Penetrates BBB. NOREPINEPHRINE DOPAMINE DOBUTAMINE BEST PROFILE OF ACTIVITY FOR BLOCKING. ANTIHYPERTENSIVE Actions: HR, F of Selective METAPORTERENOL, TERBUTALINE, ALBUTEROL, RITODINE, SALMETEROL PHENYLEPHRINE Tx: reverse HypoT COMP 1 ANTAG: Antagonists & PSVT, decongestant, topical vasoconst Tx: Don’t actually prevent CHF or stroke, even though BP. SO NOT FIRST LINE FOR HTN ANYMORE. PRAZOSIN Comp inhib on capacitance (venules) & resistance (arterioles) vessels. Side effects: Central drowsiness. hydoxylase & safe in pregnancy) GUANABENZ Uses: antihypertensive, act on med obl & symp activity w/o interfering w/ reflex. Side effects: Depr, sex dysfxn, dry mouth, & bradycardia cont & Renin release. Bc no blockage of 2 they are less likely to bronchoconstrict, block hyperglycemic action of Epi, or Epiinduced vasoconst. Tx: HTN & arrhythmias METOPROLOL Liver met, also txs angina & CHF. ATENOLOL TERAZOSIN: No t liver met, long Long acting PRAZOSIN duration, also txs Tx: benign prostatic angina. Best profile. hyperplasia ESMOLOL Short-acting, IV, used DOXAZOSIN: for MI, HTN, & Long-acting PRAZOSIN. supravent tachyarrhy, switch to LABETALOL CARVEDILOL other drug, only short (CHF) term. Note: only actions that differ from “non-selectives” are included in “selectives”. Selectives have same actions, with more specificity. Tx: Asthma, delay labor (RITODRINE, TERBUTALINE) Side effects: Tachycardia & palpitations, tremor (skel musc B2 stim) & headache (B2 vasodil) CV effect w/ IV: vasodilation, but never used! Ganglionic Agents: First group of antihypertensives, NOT USED/MANUFACTURED ANYMORE. Ganglionic Nic Rec Blockade Block ganglionic transmission – mediated by ACh released from pregang fiber acting on Nic Rec on postgang fiber. Nic Rec ing ganglions differs from skeletal muscle. Actions: Inhibits all autonomic neurotransmission. -Dilates vessels bc no NE release (1) -Tachycardia bc blocks ACh release (M) -Block autonomic reflexes -Block release of NE & Epi from adr med. Ganglionic Stimulator NICOTINE- activates postgang n & adr med via Nic Rec (influx Na). CNS stim, HR & BP, gut motility, tx toxicity w/ emetic, maintain respiration. Competitive Gang Nic Rec Antagonists: TRIMETHAPHAN Rapid metab, can cause histamin release, so use w/ caution in asthmatics & those w/ allergies. Clinical use: HypoT in surgery ( bld loss), HTN in acute dissecting aortic aneurysm or hypertensive crisis emergency. Side effects: orthostatic hypoT; vision; constipation; sex dysfxn. HEXAMETHONIUM Not approved for clinical use. Q. WHAT DRUG WOULD WIPE OUT THE EFFECTS OF NICOTINE? LABETERALOL OR CARVEDILOL. QUESTIONS: 1. 2. 3. 4. 5. 6. 7. 8. 9. Which of the following receptors when activated lead/s to an increase in BP? (Can choose more than one.) a. 1 b. Muscarinic c. 1 d. 2 e. 2 Sketch out as many charts as possible identifying Drug X as Epi, Isoproterenol, NE, 1/2/1/2-agonists & antagonists, & Trimethaphan/Nicotine. (Sarah, maybe this is something we can do for one another, make up graphs and then have the other interpret them to compare our understanding? I will try to make some over the weekend.) Write out his equation for BP & the receptors. All of the following drugs cause vasoconstriction except? (There may be more than one answer.) a. Epi b. NE c. Isoproterenol d. Dopamin e. Dobutamine f. Ephedrine Which class/es of drugs decrease TPR & BP? List some drugs in this/these category/ies. Which drug has the best antihypertensive profile? Why? Which of the following drugs would be best for treating CHF? a. Doxazosin b. Carvedilol c. Metropolol d. Esmolol e. Albuterol Do -blockers increase or decrease the release of renin? Why? What does this result in? Which drug is most likely to portray orthostatic hypotension as a side effect? ANSWERS: 1. 2. 3. 4. 5. 6. 7. 8. 9. a (cAMP) & c(IP3-Ca) See sketches. See sketch. C & e. Non-selective -blockers or 1-antagonists. “–azosin”, Labetalol, Carvedilol, Phentolamine, Phenoxybenzamine. Atenolol- most direct acting effect and less side effects. Plus, it does not get into the brain. B & c. Decrease. They dec symp stimulation, which is required to increase renin release. This results in increased U.O. Labetalol.