Click here
advertisement
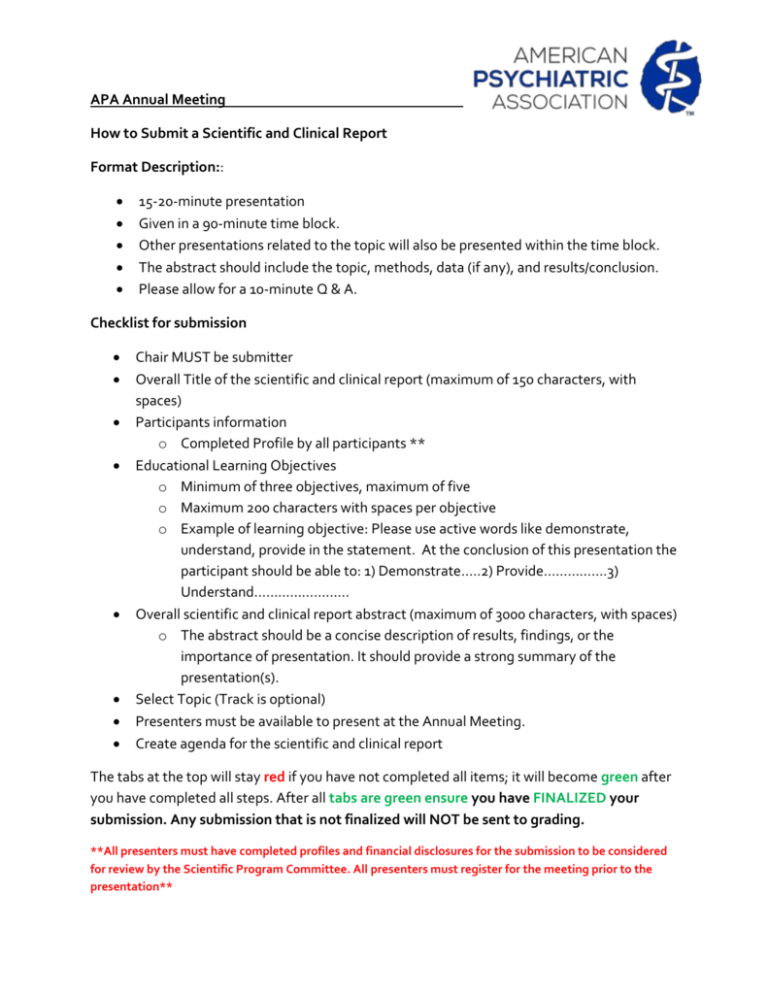
APA Annual Meeting How to Submit a Scientific and Clinical Report Format Description:: 15-20-minute presentation Given in a 90-minute time block. Other presentations related to the topic will also be presented within the time block. The abstract should include the topic, methods, data (if any), and results/conclusion. Please allow for a 10-minute Q & A. Checklist for submission Chair MUST be submitter Overall Title of the scientific and clinical report (maximum of 150 characters, with spaces) Participants information o Completed Profile by all participants ** Educational Learning Objectives o Minimum of three objectives, maximum of five o Maximum 200 characters with spaces per objective o Example of learning objective: Please use active words like demonstrate, understand, provide in the statement. At the conclusion of this presentation the participant should be able to: 1) Demonstrate…..2) Provide…………….3) Understand…………………… Overall scientific and clinical report abstract (maximum of 3000 characters, with spaces) o The abstract should be a concise description of results, findings, or the importance of presentation. It should provide a strong summary of the presentation(s). Select Topic (Track is optional) Presenters must be available to present at the Annual Meeting. Create agenda for the scientific and clinical report The tabs at the top will stay red if you have not completed all items; it will become green after you have completed all steps. After all tabs are green ensure you have FINALIZED your submission. Any submission that is not finalized will NOT be sent to grading. **All presenters must have completed profiles and financial disclosures for the submission to be considered for review by the Scientific Program Committee. All presenters must register for the meeting prior to the presentation** Example of Scientific and Clinical Reports Submission INCREASING USAGE OF SEDATIVE ANTIDEPRESSANTS IN LONG-TERM CARE HOMES AMONG ELDERLY WITH DEMENTIA: A POPULATION-BASED TIME-SERIES ANALYSIS Speaker: Akshya Vasudev, M.B.B.S., M.D. Co-Author(s): Salimah Z. Shariff, B.Math., Ph.D., Kuan Liu, M.Math., Amer M. Burhan, M.B.ChB, F.R.C.P.C., Nathan Herrmann, M.D., F.R.C.P.C., Sean Leonard, Muhammad Mamdani, Pharm.D., M.A., M.P.H. EDUCATIONAL OBJECTIVE: At the conclusion of the session, the participant should be able to: 1) To recognize the trend in usage of sedative antidepressants in patients with dementia in long-term care; 2) To learn about changes in usage of other psychotropics including benzodiazepines, antipsychotics, cognitive enhancers & anti-convulsants; 3) To appreciate extent of psychotropic polypharmacy in this vulnerable population; 4) To appreciate projection patterns of sedative antidepressants versus comparators till 2017 SUMMARY: Objective: To examine temporal changes in the prevalence of use of sedative antidepressants (mirtazapine, trazodone and triclyclics) and psychotropic polypharmacy among older adults with dementia living in long-term care homes. Design: A population-based cross-sectional time-series analysis using linked administrative databases. The study timeframe was divided into 37 intervals of 3 months (quarters) each starting from January 1, 2004 to March 31, 2013. Results were forecasted to March 31, 2017. Setting: Ontario, Canada Participants: For each quarter, older adults living in a long-term care home with a documented diagnosis of dementia within 5 years prior to the start of the quarter were identified. Main outcome measures: Prevalence rates of sedative antidepressants versus comparator agents. Results: The study population increased by 21% from n= 49,251 in the first quarter of 2004 to n= 59,785 by 2013. The prevalence of use of sedative antidepressant in the long-term care setting increased from 17% in 2004 to 31% by 2013 (p = <0.0001) and is projected to increase to 37% (95% CI 35.6% to 37.9%) by 2017. Benzodiazepine use prevalence decreased from 28% to 17% (p=<0.0001) with a projected rate of 8% (95% CI 3.1% to 12.9%) in 2017. Atypical antipsychotic use decreased from 38% to 34%(p=<0.0001) during the same period and is projected to reach 31% (95% CI 24.9% to 37.2%) in 2017. We observed a significant increase in proportion of patients on two or more psychotropics (44% to 51%, p=<0.0001)as well as those on two or more groups of psychotropics (43% to 50%, p=<0.0001) from 2004 to 2013. Conclusions: We observed an increase in use of sedative antidepressants in patients with dementia in the long-term care setting even though evidence supporting this trend remains weak and is contentious. Example of Scientific and Clinical Reports Submission REDUCING PSYCHIATRIC SYMPTOM SEVERITY IN PATIENTS WITH EPILEPSY AND NONEPILEPTIC SEIZURES Speaker: Jasper J. Chen, M.D., M.P.H. EDUCATIONAL OBJECTIVE: At the conclusion of the session, the participant should be able to: 1) Recognize the extent of psychiatric comorbidity, and comorbid depression in particular, in patients with epilepsy and patients with non-epileptic seizures; 2) Treat severe symptoms of comorbid depression in patients with epilepsy and patients with non-epileptic seizures; 3) Identify the benefits of colocating psychiatric services within epilepsy and neurology clinics in order to both reduce psychiatric symptom severity and better coordinate mental health care. SUMMARY: Rationale: Patients with epilepsy (PWE) and patients with non-epileptic seizures (PWNES) constitute particularly vulnerable patient populations and have high rates of psychiatric comorbidities. This potentially decreases quality of life and increases health care utilization and expenditures. However, lack of access to care or concern of stigma may preclude referral to outpatient psychiatric clinics. Furthermore, the optimal treatment of NES includes longitudinal psychiatric management. No published literature has assessed the impact of colocated psychiatric services within outpatient epilepsy clinics. We therefore evaluated the colocation of psychiatric services within a level 4 epilepsy center. Methods: From July 2013 to June 2014, a psychiatrist was co-located in the DartmouthHitchcock Epilepsy Center outpatient clinic one afternoon per week (0.1 FTE) to provide medication management and time-limited structural psychotherapeutic interventions to all patients that scored greater than 15 on the Neurological Disorders Depression Inventory for Epilepsy (NDDI-E) and who agreed to the referral. Psychiatric symptom severity was assessed at baseline and follow-up visits using validated scales including NDDI-E, Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder-7 (GAD-7), and cognitive subscale items from Quality of Life in Epilepsy-31 (QOLIE-31) scores. Results: Forty-three patients (18 male; 25 female) were referred to the clinic over a one-year period; 27 (64.3%) were seen in follow-up with a median of 3 follow-up visits (range 1 to 7). 37% of patients had NES exclusive of epilepsy, and 11% of patients had a dual diagnosis of epilepsy and NES. Psychiatric symptom severity decreased in 84%, with PHQ-9 and GAD-7 scores improving significantly from baseline (4.6 ± 0.4 SD improvement in PHQ-9 and 4.0 ± 0.4 SD improvement in GAD-7, p-values <0.001). NDDI-E and QOLIE-31 cognitive sub-item scores at their most recent visit were significantly improved as compared to nadir scores (3.3 ± 0.6 SD improvement in NDDI-E and 1.5 ± 0.2 SD improvement in QOLIE-31, p-values <0.001). These results are moreover clinically significant-defined as improvement by 4-5 points on PHQ-9 and GAD-7 instruments-and are correlated with an overall improvement as measured by NDDI-E and cognitive subscale QOLIE-31 items. Conclusion: A co-located psychiatrist demonstrated a reduction in psychiatric symptoms of PWE and PWNES, as well as an improvement in psychiatric access and streamlining of their care. Epileptologists were able to dedicate more time to managing epilepsy as opposed to psychiatric comorbidities. As integrated models of collaborative and co-located care are becoming more widespread, mental health care providers located in outpatient neurology clinics may provide significant benefit for both patients and providers. PREDICTIVE VALUES OF SCREENING QUESTIONS FOR LIFETIME AND PAST 12-MONTHS DIAGNOSIS OF MAJOR DEPRESSIVE DISORDER Speaker: Venkat Bhat, M.D. Co-Author(s): Aihua Liu, Ph.D., Jean Caron, Ph.D., Gustavo Turecki, Ph.D EDUCATIONAL OBJECTIVE: At the conclusion of the session, the participant should be able to: 1) To understand the predictive values of the two screening questions for Major Depressive Disorder for lifetime and past 12 month diagnoses; 2) To appreciate epidemiological and numeric perspectives in the depression diagnosis algorithm from the screening questions to final diagnosis; 3) To recognize the nature of symptom distribution when subjects meet or fail to meet the final list of 9 symptoms of Major Depressive Disorder. SUMMARY: Introduction: The sensitivity, specificity and predictive values of the two screening questions (first is being sad, empty or distressed, second is being discouraged) have been examined in various contexts and comorbidities for diagnosis of Major Depressive Episode (MDE). However, the predictive values of the two screening questions have not been studied in the context of last 12 month and lifetime diagnosis of Major Depressive Disorder (MDD). Further, this predictive value has not been examined in a population that is random and representative, and in the context of the nature of final distribution of individual symptoms. This study aimed to examine predictive values and symptom distribution by examining the algorithmic flow of numbers from the screening questions to final diagnosis of MDE during the last 12 months and lifetime. Methods: The Montreal Epidemiological Catchment Area Study (ECA) is a longitudinal project currently underway at the Douglas Institute. The ECA study under the form of a community survey includes a randomly selected sample of 2434 individuals between 15 and 65 years of age (T1); 1823 agreed to be re- interviewed two years later (T2). Mental disorders were identified with the Canadian Community Health Survey (CCHS 1.2) version of the Composite International Diagnostic Interview. This study specifically examined the MDD algorithm in the context of last 12 month and lifetime MDD diagnosis. Further, the symptom distribution was studied in the context of lifetime diagnosis of depression. Results: For lifetime MDD diagnosis among 2433 subjects, 1401 answered affirmatively for the first screening question and among the remaining 1032 subjects, 145 answered affirmatively for the second screening question. For the first screening question, 550 subjects had a final diagnosis of MDD (PPV-0.39) and for the second question, 22 subjects had a final MDD diagnosis. For the last 12 months MDD diagnosis among 1823 patients, 143 subjects had a final MDD diagnosis among 473 who answered affirmatively to the first question (PPV-0.30), and 4 had a final MDD diagnosis among 77 who answered affirmatively to the second question. Among patients with lifetime MDD diagnosis, feelings of worthlessness and psychomotor symptoms were the least frequently reported symptoms. In addition, most people who reported episodes of being sad, empty or distressed, also reported being discouraged in the detailed symptom review. Conclusion: The important finding is that most of the final diagnosis of MDD (both with lifetime and last 12 month) is captured by the first screening question and there is then a significantly lower yield for the second question, and this is because of the high correlation in the symptoms covered by the two screening questions. The study is from a representative population and suggests that worthlessness and psychomotor symptoms are the least prevalent among subjects with final lifetime diagnosis.