Pharmacology Overview for PALS
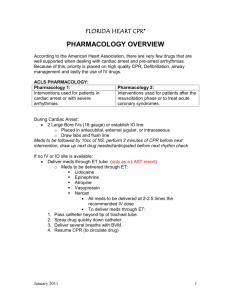
advertisement

FLORIDA HEART CPR* Pharmacology for PALS According to the American Heart Association, there are very few drugs that are well supported when dealing with cardiac arrest and pre-arrest arrhythmias. Because of this, priority is placed on high quality CPR, Defibrillation, airway management and lastly the use of IV drugs. : The following interventions should be used for patients in cardiac arrest or with severe arrhythmias. Establish IV or intraosseous (IO) access. Draw labs and flush line IVP meds must be followed by 10cc of normal saline Perform 2 min. of CPR before next intervention Draw up next drug needed before next rhythm check If no IV or IO site is available: Deliver meds through ET tube only as a last resort! Meds that can be delivered through ET: Lidocaine Epinephrine Atropine Narcan All meds to be delivered at 2-2.5 times the recommended IV dose, except epinephrine. The recommended endotracheal dose of epinephrine is 10 times the IV dose. To deliver meds through ET: 1. 2. 3. 4. 5. Remove needle from syringe if necessary Pass catheter beyond tip of tracheal tube. Spray drug quickly down catheter. Deliver several breaths with BVM. Resume CPR (to circulate drug) 1 Pharmacology for PALS The following are pharmacologic agents that may be relevant during resuscitation of pediatric cardiac arrest. Be advised that your PALS textbook offers a more detailed version of this list and you should refer to the text prior to your PALS course for further information. VASOPRESSORS EPINEPHERINE Classification: Catecholamine, vasopressor, inotrope Indications: Cardiac Arrest, anaphylaxis, asthma, symptomatic bradycardia Croup, hypotensive shock, toxins/overdose Positive β effects (increased heart rate, contractility and automaticity) Positive α effects (peripheral vasoconstriction) IVP IV every 3-5 minutes (see Broselow tape for exact weight based doses) IV/IO push Tachycardia Hypertension PVC’s Palpitations Increased myocardial O2 demand Actions: Dosage: Route: Adverse Effects: The α-adrenergic-mediated vasoconstriction of epinephrine increases aortic diastolic pressure and thus coronary perfusion pressure, a critical determinant of successful resuscitation. Although epinephrine has been used universally in resuscitation, there is little evidence to show that it improves survival in humans. Both beneficial and toxic physiologic effects of epinephrine administration during CPR have been shown in animal and human studies. Current studies show no survival benefit from routine use of high dose epinephrine and it may be harmful, particularly in asphyxia arrest. High dose epinephrine may be considered for special resuscitation circumstances. (Chapter 9 PALS text) **REFER TO THE BROSELOW TAPE FOR EXACT DOSES!** 2 ANTIARRHYTHMICS AMIODARONE Indications: Actions: Dosage: Route: Adverse effects SVT, Ventricular tachycardia with pulses, Pulseless arrest (VF and Pulseless V-Tach. Prolongs the action potential duration and effective refractory period, slows sinus rate, prolongs PR and QT intervals and noncompetitively inhibits α-adrenergic and β-adrenergic receptors VF/VT= Cardiac arrest: 5mg/kg IVP for first dose and up to 15mg/kg max dose (see Broselow tape for exact weight based doses) For SVT and V-Tach with pulses 5mg/kg IV/IO over 2060 minutes (max dose 300mg) Upon ROSC: See JHACO Guidelines for infusions IV/IO Hypotension, Bradycardia, SA node dysfunction, sinus arrest, CHF, torsades, pulmonary fibrosis, ARDS Amiodarone may be considered as part of the treatment of shock-refractory or recurrent VF/VT. Amiodarone has α-adrenergic and β-adrenergic blocking activity; affects sodium, potassium, and calcium channels; slows AV conduction; prolongs the AV refractory period and QT interval; and slows ventricular conduction (widens the QRS). Adult studies showed increased survival to hospital admission but not to hospital discharge when amiodarone was used compared to lidocaine. One study in children demonstrated the effectiveness of amiodarone for life-threatening ventricular arrhythmias, but there have been no published studies on the use of amiodarone for pediatric cardiac arrest. 3 LIDOCAINE Classification: Indications: Anti-arrhythmic Ventricular Fibrillation, Pulseless Ventricular Tachycardia, Rapid sequence intubation (RSI) i.e. ICP protection Actions: Depresses ventricular irritability and automaticity Increases fibrillation threshold Dosage: V-Tach with a pulse or VF/Pulseless VT: see Broselow tape for weight based doses. MAINTENANCE INFUSION upon ROSC: see JHACO infusion protocol. Route: IVP, IO or IV Infusion Adverse Muscle tremors, heart block, myocardial depression, Effects: hypotension, seizures, cardiac arrest in bradycardias. Lidocaine continues on next page. Lidocaine has long been recommended for the treatment of ventricular arrhythmias in infants and children because it decrease automaticity and suppresses ventricular arrhythmias. Data from a study of shock-refractory VT in adults showed that lidocaine was inferior to amiodarone, so lidocaine has been recommended as a second line drug in shock-refractory cardiac arrest only when amiodarone is not available. Its indications in the treatment of other ventricular arrhythmias are uncertain. There have been no published studies on the use of lidocaine in pediatric cardiac arrest. MAGNESIUM SULFATE Classification: Indications: Actions: Dosage: Adverse Effects: Electrolyte, bronchodilator Hypomagnesemia Torsades de Pointes Asthma (refractory status asthmaticus) Smooth muscle relaxer Exerts antiarrhythmic action Cardiac arrest due to torsades: IV/IO route 25-50mg/kg; 25-50 mg/kg over 10-20 minutes for VT with pulses associated with torsades or hypomagnesemia; 25-50mg/kg by slower infusion (15-30 minutes) for treatment of status asthmaticus. Mild bradycardia, hypotension, hypermagnesemia, respiratory depression, weakness, heart block, and cardiac arrest may develop with rapid administration. Contraindications: renal failure Magnesium Sulfate should be administered for the treatment of torsades de pointes or hypomagnesemia. There is insufficient evidence to recommend for or against the routine use of magnesium in pediatric cardiac arrest. 4 OTHER AGENTS ATROPINE Classification: Indications: Actions: Dosage: Route: Adverse Effects: Anticholinergic Symptomatic bradycardia (usually secondary to vagal stimulation; Toxins (organophosphate overdose, carbamate); rapid sequence intubation (i.e. when using succinylcholine) Increases heart rate and cardiac output by blocking vagal stimulation; blocks acetylcholine and other muscarinic agonists 0.5 mg IVP in bradycardic patient. NOT TO EXCEED 3.0 mg IV or IO Tachycardia, dilated pupils, blurred vision, headache, dysuria, weakness, bradycardia if used in smaller than recommended doses. **Document clearly if used for patients with head injury, because atropine will distort pupillary exam by causing pupil dilation. **Special considerations: Use drug in any child with bradycardia at time of endotracheal intubation. Consider using drug to prevent bradycardia when succinylcholine is used in an infant or young child, especially in the presence of hypoxia and acidosis. Atropine is indicated for the treatment of bradyarrythmias. There are no published studies suggesting its efficacy for treatment of cardiac arrest in pediatric patients. (See PALS text for complete discussion) CALCIUM CHLORIDE Classification: Indications: Actions: Dosage: Adverse Effects: Calcium ion (electrolyte) Hypocalcaemia, hyperkalemia, consider for hypomagnesaemia and treatment of calcium channel blocker overdose. Needed for maintenance of nervous, muscular, skeletal systems, enzyme reactions, normal cardiac contractility, and blood coagulation. 20 mg/kg IO/IV slow push during cardiac arrest if hypocalcemia is known or suspected; may repeat if documented or suspected clinical indication persists. Infuse over 30-60 minutes for other indications Hypotension, bradycardia, asystole, heart block, cardiac arrest, arrhythmias, venous thrombosis, necrosis upon infiltration, hypercalcemia 5 SODIUM BICARBONATE Classification: Indications: Alkalinizing agent, electrolyte, buffer Metabolic acidosis from an unknown cause or suspected acidosis from confirmed prolonged down time, sodium channel blocker overdose (e.g.Tricyclic antidepressant) Hyperkalemia Actions: Increases plasma bicarbonate, which buffers H+ ion (reversing metabolic acidosis) forming carbon dioxide; elimination of carbon dioxide via the respiratory tract increases pH. Dosage: 1mEq/kg IV push, can be repeated as ordered by clinician in cardiac arrest Route: IV/IO **Special considerations: Do not administer via endotracheal route; Irrigate IV/IO tubing with NS before and after infusions or use another line to administer. Sodium bicarbonate is recommended for the treatment of symptomatic patients with hyperkalemia, Tricyclic antidepressant overdose, or an overdose of other sodium channel blocking agents. Routine use of sodium bicarbonate in cardiac arrest is not recommended. After you have provided effective ventilation and chest compressions and administered epinephrine, you may consider sodium bicarbonate for prolonged cardiac arrest. ADENOCARD/ADENOSINE Classification: Indications: Dose: Actions Antiarrhythmic SVT IV/IO Rapidly: Exact weight based doses on Broselow tape Briefly blocks conduction through AV node and interrupts pathways through AV node. Allows return of NSR in patients with SVT, including SVT associated with WPW. Depresses sinus node automaticity. ******Note: This is NOT a complete list of drugs used in the PALS course. Please consult your PALS textbook for a complete list of drugs including classifications, indications, doses and actions of each drug. 6