Blue-J-PSW-editorial-v3 - Spiral
advertisement

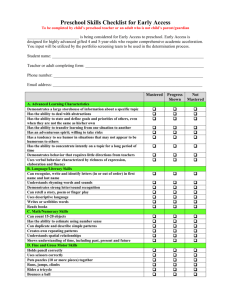
Onset of structural airway changes in preschool wheezers: a window and target for secondary asthma prevention? Sejal Saglani1, Andrew Bush1 1 Leukocyte Biology and Respiratory Paediatrics, National Heart and Lung Institute, Imperial College and Royal Brompton Hospital, London Correspondence to: Dr Sejal Saglani Reader in Respiratory Paediatrics 368 Sir Alexander Fleming Building Imperial College London London SW7 2AZ Tel: 0044 2075943167 Fax: 0044 2075943119 Email: s.saglani@imperial.ac.uk Funders: SS is an NIHR Career Development Fellow, AB is an NIHR Senior Investigator Running title: Preschool wheeze and remodelling Data from birth cohort studies shows convincingly that lung function is reduced in the early preschool years in children who develop asthma1-3. The loss in lung function is maximal by school age and tracks to adulthood without recovery4, 5. We also have evidence from biopsy studies in very young children that suggests although the pathological abnormalities of asthma (eosinophilic inflammation and a specific feature of airway remodelling, increased reticular basement membrane (RBM) thickness) were not present in infants with respiratory symptoms and reversible airflow obstruction at a median age of 1 year6, they were present in preschool children with severe recurrent wheeze aged 3 years7, 8. Interestingly, the increased RBM thickness was not yet maximal at preschool age, but by school-age (median age 12 years) was equivalent to that seen in adults with asthma9. Combined, the biopsy studies to date suggested a gradual development of airway remodelling in symptomatic children with severe wheezing between infancy and school-age, reflecting the lung function data from longitudinal birth cohorts. Acknowledging these data are from several different studies, and the biopsy studies are only cross-sectional, it has been proposed that the majority of structural airway changes in asthma develop early in life, in the first 5 years in parallel with the abnormalities of lung function, and subsequently remain10. These changes may also explain the irreversible loss of lung function that is sustained through adulthood. In addition to RBM thickness, other features of airway remodelling that have been reported in preschool wheezers include angiogenesis and epithelial shedding, both increased compared to agematched, non-wheezing controls8. Airway smooth muscle (ASM) has only been reported in one study of preschool children with severe recurrent wheeze, and was not different in amount between wheezers and controls (median age 3 years)11. The most interesting finding was that early airway smooth muscle was the only predictor of future asthma development, not RBM thickness nor eosinophilic inflammation. It has become apparent that abnormal structural airway wall changes occur early in children with wheeze, however, to date, studies have predominantly grouped together all children between 1 and 5 years old. Even this relatively small time period is likely to be too large to appreciate when abnormal changes begin since the period of rapid airway growth in healthy children is in the first 2-3 years, and indeed it has been shown that normal development of the RBM is maximal in the first year of life12. In this regard, the manuscript by Guillaume et al [add as reference] adds significantly to our knowledge of the early development of structural airway wall changes in children with severe wheeze. 49 preschool children were split into those aged ≤36 months (n=20) or 37-59 months (n=29). RBM thickness was lower in the younger group, and although there was a lot of overlap between groups, this confirms the previous findings that the abnormal thickening develops during the preschool years. Importantly, inflammation was not related to any marker of airway remodelling, thus suggesting anti-inflammatory therapies are unlikely to modify structural changes. Moreover, markers of airway remodelling were not different between multiple trigger and episodic viral wheezers, suggesting clinical wheeze phenotypes cannot be used as a surrogate to determine the presence of airway remodelling, and supports the proposition that prediction of disease outcome by school-age cannot be based solely on clinical preschool wheeze phenotypes. An intriguing novel finding included the presence of increased ASM in atopic compared to nonatopic preschool wheezers [Guillaume et al]. In contrast, other markers of remodelling including RBM thickness, increased vessels and epithelial loss have previously found to be similar in atopic and non-atopic preschool wheezers8. These data suggest a closer relationship between ASM muscle and atopy than any of the other structural airway changes. However, in contrast to RBM thickness, the amount of ASM was not different between younger and older preschool wheezers. Bearing in mind ASM is the only structural cell that has been reported as a predictor of future asthma, these new findings suggest functional characteristics of ASM in atopic children with severe recurrent wheeze that are likely to develop asthma may be altered early. ASM remodelling is also the only change that has been convincingly associated with alterations in lung function in paediatric asthma.13 The relationship between increased ASM and atopy in preschool wheezers found here may therefore explain the early abnormalities in lung function reported from birth cohorts in atopic children that develop asthma. ASM mass was greater by school-age in children with established disease compared to preschool wheezers, suggesting a window between preschool and school-age during which an intervention targeted to prevent ASM dysfunction, specifically in atopic severe preschool wheezers may allow disease modification. The challenges of performing biopsy studies in very young children cannot be under estimated, and for this reason, non-wheezing controls could not be included in this study. This does mean that the findings need to be interpreted with caution, since they may simply reflect normal developmental changes, especially since we do not know which, if any of the children included will develop asthma, and assessments of lung function were not made. However, allowing for this limitation, when these data are put into the context of findings from the relatively few other biopsy studies that have been performed in preschool children with severe wheeze, we now have some really interesting direction towards an optimal time period for intervention (early preschool age), and also the likely optimal airway cell that perhaps should be targeted, in the context of atopy, to allow us to achieve the ultimate goal of secondary prevention in asthma (Figure 1). Legend for figure: Figure 1. Relationships between lung function, structural airway changes and atopic sensitisation in preschool wheeze. Preschool children with recurrent wheeze that develop asthma by school-age have an early reduction in lung function that develops between birth and 6 years. Structural airway changes develop in parallel between 1 and 6 years in preschool wheezers, and the changes in airway smooth muscle are specifically increased in those that have evidence of early atopic sensitisation. Combined, the pathophysiological data suggest a window between 1 and 3 years during which an intervention may minimise reduction in lung function and allow disease modification. Reference List 1. Lowe,L. et al. Specific airway resistance in 3-year-old children: a prospective cohort study. Lancet 359, 1904-1908 (2002). 2. Lowe,L.A. et al. Wheeze phenotypes and lung function in preschool children. Am J Respir Crit Care Med. 171, 231-237 (2005). 3. Morgan,W.J. et al. Outcome of Asthma and Wheezing in the First Six Years of Life: Follow-up through Adolescence. Am J Respir Crit Care Med. 172, 1253-1258 (2005). 4. Sears,M.R. et al. A longitudinal, population-based, cohort study of childhood asthma followed to adulthood. N. Engl. J Med. 349, 1414-1422 (2003). 5. Tai,A. et al. The association between childhood asthma and adult chronic obstructive pulmonary disease. Thorax 69, 805-810 (2014). 6. Saglani,S. et al. Airway remodeling and inflammation in symptomatic infants with reversible airflow obstruction. Am J Respir Crit Care Med. 171, 722-727 (2005). 7. Saglani,S. et al. Early detection of airway wall remodeling and eosinophilic inflammation in preschool wheezers. Am J Respir Crit Care Med. 176, 858-864 (2007). 8. Turato,G. et al. Nonatopic children with multitrigger wheezing have airway pathology comparable to atopic asthma. Am J Respir Crit Care Med. 178, 476-482 (2008). 9. Payne,D.N. et al. Early thickening of the reticular basement membrane in children with difficult asthma. Am J. Respir Crit Care Med. 167, 78-82 (2003). 10. Jackson,D.J., Hartert,T.V., Martinez,F.D., Weiss,S.T., & Fahy,J.V. Asthma: NHLBI Workshop on the Primary Prevention of Chronic Lung Diseases. Ann. Am. Thorac. Soc. 11 Suppl 3, S139-S145 (2014). 11. O'Reilly,R. et al. Increased airway smooth muscle in preschool wheezers who have asthma at school age. J. Allergy Clin. Immunol.(2012). 12. Tsartsali,L. et al. Development of the bronchial epithelial reticular basement membrane: relationship to epithelial height and age. Thorax 66, 280-285 (2011). 13. Regamey,N. et al. Increased airway smooth muscle mass in children with asthma, cystic fibrosis, and non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 177, 837843 (2008).