presentation
advertisement
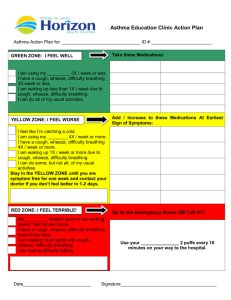
Common Paediatric Emergency Referrals Mark Anderson Consultant Paediatrician Great North Children’s Hospital Case 1 Archie, 18 months Unwell for 2 days with runny nose and cough Felt hot Difficulty breathing & wheezy today Archie, 18 months Examination Coryzal Mild subcostal recession Quiet wheeze throughout chest Differential diagnosis? Differential diagnosis Viral induced wheeze (VIW) – episodic wheeze 1st presentation “asthma” – multi-trigger wheeze (Bronchiolitis) How to differentiate VIW from “asthma”? How to differentiate VIW from “asthma”? Can be difficult! Asthma more likely if Multiple triggers for wheeze Interval symptoms Personal or family history of atopy Absence of virus (!) Specific Therapy? Specific therapy Inhaled bronchodilator Salbutamol Ipratropium bromide ?Steroids Steroids in preschool VIW Little evidence for efficacy 120 children aged 1-5y given prednisolone or placebo No effect on parental reported respiratory symptom score at 7 days 700 preschool children given prednisolone or placebo No effect on duration of hospitalisation No effect on respiratory symptom score in first 24 hours Steroids in preschool VIW Short burst therapy probably should be reserved for clinical features suggestive of atopic asthma History of multi-trigger wheeze Severe eczema Family history of atopy What determines need for admission? What determines need for admission? Oxygen requirement (SpO2 <93%) Respiratory effort Hydration concerns Social complications Take home points Preschool wheeze appears to have multiple phenotypes Short burst oral steroids no longer the cornerstone of management for all preschool wheeze Questions? Case 2 Micah, 2 years Unwell for 2 days with runny nose and cough Feels hot Mum noticed lump in neck What do you want to know? What do you want to know? Well/unwell Location Size Heat Other lymphadenopathy Spleen/liver Micah, 2 years 4-5cm diameter firm swelling in upper cervical chain Non-fluctuant A few other small lymph nodes No swallowing issues Well otherwise Plan of action? Plan of action? Do nothing? Investigations? Oral antibiotics? Intravenous antibiotics? Causes of acute cervical lymphadenopathy “Reactive” Infection Bacterial Atypical mycobacterium TB Other Plan(s) of action Fluctuant node Incision & drainage/excision Well Oral antibiotics for 7-10 days – review in 48-72h Unwell IV antibiotics Investigations probably only indicated for persistent adenitis (>2 weeks) Take home points Acute adenitis If collection suspected, needs I&D Oral antibiotics & review appropriate for the majority of well children Questions? Case 3 Bethany, 6 years Awoke complaining of left hip and thigh pain Previously fit and well apart from an upper respiratory tract infection 7 days previously What else do you want to know? What else do you want to know? Characteristics of the pain Systemic features Recent travel or systemic illness Medication history (Trauma) Bethany, 6 years Refused to weight bear Became very distressed at attempted examination Temperature 38.7 Flushed & tachycardic Differential diagnosis of the limping child? Differential diagnosis of the limping child Transient synovitis/ ”reactive” arthritis Septic arthritis/osteomyelitis Perthes’ disease Slipped Upper Femoral Epiphysis JIA Malignancy Abdominal/testicular pathology Discitis, Lyme disease, NAI Red flags Severe & unremitting pain Complete non-weight bearing Pseudoparalysis Night pain Fever Back pain Features of malignancy Bethany, 6 years Differential diagnosis Septic arthritis Reactive arthritis Investigations? Investigations White cell count 11.5 x 109/L CRP 30mg/L ESR 15 mm/h Plain X-ray normal Urgent ultrasound – hip effusion Kocher’s clinical prediction rule Factors Fever >38 Unable to weight bear ESR>40mm/hr in the first hour Serum WCC >12x106/L Probability of septic arthritis No factors present <0.2% 2 factors present 40% 3 factors present 93% 4 factors present >99% Bethany, 6 years Presumptive diagnosis septic arthritis Joint aspiration & wash out Gran stain negative >50,000 white cells/mm3 on microscopy IV antibiotics for 2 weeks, oral for 4 weeks Take home points Limping is a common presentation Limping is not a diagnosis Not all children need excessive investigation All children need clear follow up plans Thank you!