Skill Sheet – Patient Assessment/BATH
advertisement

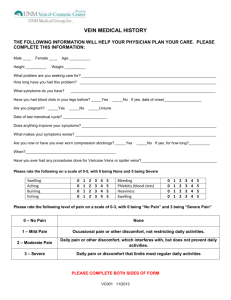
Skill Sheet – Patient Assessment/BATH Learning Objective: Demonstrate the proper technique and sequence for performing a rapid patient trauma assessment using the BATH acronym. References: TECC/TCCC guidelines, ALERRT instruction Evaluation Method: Students will be evaluated as a Pass/Fail (P/F). The instructor will verify the accuracy of the student’s ability to explain and perform a patient trauma assessment utilizing the BATH acronym. Materials: Student checklist Instructor Guidelines: 1. Provide each student with a student checklist 2. Ensure student has all student-required materials 3. Read the learning objective and the evaluation method to the student 4. Explain the grading of the exercise 5. Have student explain/perform a patient assessment 6. Use “notes” section to insure consistency in evaluating Performance Steps: 1. Explain when the patient assessment is performed 2. Explain use of BATH acronym for completing a patient assessment 3. Demonstrate placing patient into supine position for assessment 4. Demonstrate proper approach and sequence for completing “B”, explain “plus 1” rule 5. Explain when and how bleeding injuries found during “B” assessment are treated 6. Demonstrate/Explain “A” assessment; Look, Listen, Feel 7. Explain treatment for compromised airway in unconscious and conscious patients 8. Explain evaluation of “T”, when tension pneumothorax is likely to occur, and field treatment by non-medical personnel 9. Explain “H” evaluation, complications of hypothermia for the trauma patient, and treatment/prevention. Patient Assessment/BATH Task 1st 1. 1. Explains when the patient assessment is performed Completed 2nd 3rd P / F P / F P / F P / F P / F P / F P / F P / F P / F 4. Demonstrates proper approach, sequence and technique for completing “B”, explains “plus 1” rule P / F P / F P / F 5. Explains when and how bleeding injuries found during “B” assessment are treated 6. Demonstrates/Explains “A” assessment P / F P / F P / F P / F P / F P / F 7. Explains treatment for compromised airway in unconscious and conscious patients P / F P / F P / F 8. Explains evaluation of “T”, when tension pneumothorax is likely Applies pressure and secures windlass) personnel to occur, and (tightens field treatment by non-medical P / F P / F P / F P / F P / F P / F P / F P / F P / F 2. Explains use of BATH acronym for completing a patient assessment 3. Demonstrates placing patient into supine position for assessment 9. Explains “H” evaluation, complications of hypothermia for the trauma patient, and treatment/prevention. 10. Overall Grade Critical Criteria: ____ Did not perform patient assessment utilizing BATH acronym ____ Did not complete initial bleeding assessment before stopping to perform treatment ____ Did not roll patient to assess back of legs or back Evaluator’s comments: NOTES: 1. Completed on initial Pt contact during Phase 2 (Indirect Threat) or 3 (Evac Care), NOT Phase 1 (Direct Threat). Can be re-accomplished following any patient movement. 2. Used to rapidly assess treatable life threatening injuries, initial bleeding sweep should take no more than 30 seconds 3. First step is to place any critically injured patient supine (on their back). Verbalize C-spine precautions are not required for penetrating injuries and should not delay a rapid and effective BATH assessment. 4. Approach from feet of patient, assess legs front and back, neck, arms – treat major bleeds then assess trunk front and back, proper technique involves touching (with closed fingers) and seeing all areas of the patient (seeing where you are placing your hands, clothes are not removed at this stage), patient must be rolled to assess back of legs and trunk, legs are assessed from groin and buttocks to feet, neck is assessed for major bleeding in the area of the carotid arteries and jugular veins, arms are assessed from arm pits and shoulders to hands. Initial bleeding sweep focuses on extremities, neck, and areas of the body amenable to direct pressure/wound packing; groin, buttocks, armpits, subclavian (shooting pocket). 5. If alone complete initial bleeding sweep (legs, neck, arms) before any treatment is performed, if you have help you can direct others to provide direct pressure while you complete the bleeding sweep. Once the initial bleeding sweep is completed (legs, neck, and arms) you go back and treat life threatening bleeds in order of severity. Following treatment of life threatening bleeds the trunk is assessed and occlusive dressing are applied to penetrating trunk (chest, back, abdomen) injuries. 6. Assess quality of breathing by looking at patient for signs of distress, chest rise, listening for abnormal breathing sounds, if patient is unconscious feel for air movement. Perform head tilt chin lift if any abnormalities are noted. Look in patient’s mouth for obvious obstructions and remove if able to grasp without fear of pushing object further down airway. NOTE: wound packing will be delayed until this point in the assessment if you have additional help who can maintain direct pressure until the “B” and “A” have been accomplished. 7. Roll unconscious patients into the recovery position. Allow conscious patients to assume position most comfortable to them. 8. Tension Pneumothorax is assumed in any patient with chest trauma, penetrating or blunt, monitor for signs of breathing difficulty. Assume any patient with a chest seal applied will develop a tension pneumothorax. Field treatment involves “burping” or pealing back the chest seal in an attempt to allow the tension build-up to vent through the open hole. Burp the chest seal and then immediately re-apply. 9. Hypothermia is a major concern for patients with suspected internal bleeding or patients with significant blood loss. Patients in shock are no longer able to maintain their normal body temperature (98.6). As their core temperature approaches 91 degrees their ability to clot is severely degraded and any internal (non-compressible) injuries will continue to bleed. Protect these patients from any further heat loss if at all possible. Consider wrapping in blankets and insulating them from surfaces that increase heat loss such as concrete. These patients need to be actively warmed if at all possible (blankets are designed to hold in body heat, these patients aren’t producing body heat). This can be accomplished by using the Hypothermia Prevention and Management Kit (HPMK) or placing the patient in a heated environment such a vehicle with the heater running. This is a year round concern, not just a winter concern.