SS_BRS Research Forum_May 15 - University of Hertfordshire
advertisement

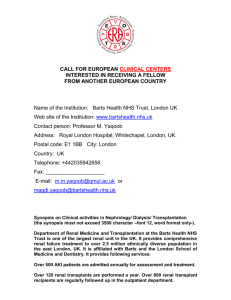
Developing depression screening tools to meet the linguistic needs of patients with ESRD from South Asian backgrounds Sharma S1, Mooney R1, Davenport A2, Day C3, Duncan N4, Warwick G5, Yaqoob M6, Bhui K7, Randhawa G8,, Wellsted D1, Da Silva-Gane M9, Farrington, K9 1 Centre for Lifespan and Chronic Illness Research, University of Hertfordshire, 2Renal Unit Royal Free Hampstead NHS Foundation Trust, 3Renal Unit Birmingham Queen Elizabeth NHS Foundation Trust, 4 Renal and Transplant Centre Hammersmith Imperial College NHS Trust, 5University Hospitals of Leicester NHS Trust, 6Centre of Translational Medicine and Therapeutics, William Harvey Research Institute, Barts and the London, Queen Mary University of London, 7Wolfson Institute of Preventive Medicine, Barts and The London School of Medicine and Dentistry, 8Institute for Health Research, University of Bedfordshire, 9 Renal Unit Lister Hospital, Stevenage NHS Trust Research funded by the British Renal Society and British Kidney Patients Association (2013); NIHR RfPB (2014-2016) Depression is common experience on dialysis. It is estimated that at any one time, up to 30 per cent of patients experience clinically significant symptomatology. Self-report screening questionnaires, usually based on established western diagnostic criteria, aid the classification of patient symptoms as mild, moderate or severe and so facilitate access to support. The majority of scales have been developed for use with white English speaking groups and assume that the experience of depression is universal. Cultural beliefs, however, are known to impact conceptualisations and so expression of distress. Given that a significant proportion of renal service users are from South Asian backgrounds- with origins in India, Pakistan and Bangladesh- and that language barriers are frequent, it is difficult to explore low mood and support needs in this group. We discuss the early stages of a research programme aimed at specifying suitable depression screening practices for patients with limited English language skills, recognising that national guidelines on the identification of distress in ethnic minorities are also lacking. Whilst there are numerous frameworks designed to aid the adaptation of Patient Reported Outcomes Measures, we provide an overview of the challenges associated with such an undertaking and with a focus on: attributes of translators, the usefulness of back translation, and patient preferences for methods of scale completion given varying levels of literacy. Emerging issues are of relevance in the broader context of renal where challenges exist related to the inclusion of diverse groups in health research.