OPAT standard operational policy
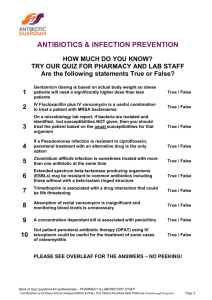
advertisement

Outpatient Parenteral Antibiotic Therapy (OPAT) Service Operational Procedure Author(s) – Job titles Rashida Goswami (OPAT/Vascular Access Nurse Victoria Longstaff (Infection Control Nurse Consultant ) Version 1 Version Date September 2014 Implementation/approval Date DRAFT Review Date Reviewing Committee Policy Reference Number Version Control Version Number Date Author (Job Title) 1 16/09/2014 OPAT/Vascular Access Nurse 1 Reason Ratification required? New service Yes 1 ScopeThe standard Operation Procedure applies to all healthcare professionals involved in direct or indirect care of patients requiring delivery of Outpatient Parenteral Antibiotic Therapy 2 Objectives of the OPAT service: To facilitate the discharge of a selected group of patients by providing an OPAT service. To provide specialist advice in the care of the OPAT patient. Audit the activities of the OPAT service. Champion the OPAT service both within the hospital and community. 3 Principles of the OPAT Service at HUH: OPAT team at Homerton University Hospital includes Clinical Nurse Specialist, Consultant Microbiologists/ID, and Antimicrobial Pharmacists. Microbiology/ID SpR available for clinical advice/support as required and Infection Control Nurses to assist in service cover. It has been agreed by the OPAT team; The referral for OPAT will be made by the patient’s clinical team using the appropriate referral form (Appendix 1) and contacting the team to discuss the case; the team may already be aware of the patient through multidisciplinary team Microbiology/Infectious diseases meetings (MDT). The OPAT team may have already placed a vascular access device, (VAD) at the request of the clinical team. Clinical responsibility will remain with the clinical team; a consent document (Appendix 2) to this effect will be signed by the clinical team and the patient prior to discharging the patient. This document outlines the responsibilities of the clinical team and patient. This document sits with the OPAT patient held notes (Appendix 3). The patient held notes stays with the patient for the duration of therapy and are then is filed in the patients main medical records Before discharge all OPAT patients will have been discussed at the weekly MDT meetings (virtual ward round). At other times to facilitate early discharge the OPAT nurse will consult with either the ID/Microbiology consultant to discuss appropriateness of antimicrobial regimes. The discharge pathway is outlined in Appendix 4; this is meant as a guide only and any part of the pathway can occur at varying times depending on the 2 individual patients and their needs. All patients follow this pathway irrespective of clinical condition, including those patients accepted from outpatient clinics and A&E areas. Exclusion/inclusion criteria, o This service is for adult patients, o All patients will be assessed individually by the OPAT nurse regarding the appropriateness of OPAT using OPAT Suitability Assessment Form Appendix 5 o Appropriate antimicrobial therapy that can be delivered in the outpatient/community setting safely. 4 Roles and Responsibilities – Patient’s Designated Team Clinical responsibility will remain with the consultant discharging the patient from hospital. Team must complete OPAT referral form available on trust intranet site. A full suitability assessment will be carried out by the OPAT CNS. Consultant Microbiologist will review the patient once accepted by the OPAT CNS. The Team responsible for the patient care must prescribe intravenous antibiotics on TTA’s for the duration until patient is reviewed by the Consultant Microbiologist in outpatient clinic. The OPAT nurse will co-coordinate further supplies. The responsible team for patient must complete and sign consent form. The OPAT medication administration chart must be completed for all patients before discharge. All patients must have a minimum of one dose of their OPAT medications in hospital before their discharge. OPAT consultant There will be a designated Micro/ID consultant responsible for the OPAT service at all times. The OPAT consultant will initially review patient as an inpatient and devise patient management plan prior to discharge. Outpatient clinic review for weekly OPAT management plan including response to treatment and monitoring for potential adverse effects. Request and review any investigations e.g. bloods tests including therapeutic drug monitoring. Communicate with the referring consultant/GP and other MDT members as required Lead MDT virtual ward weekly 3 OPAT Nurse The role of the OPAT nurse includes the following: Assess patient and carer suitability. Patient and carer education and support. Coordinate with ward pharmacist regarding discharge planning and ongoing outpatient supplies of IV antimicrobials. Co-ordinate OPAT clinic review. Co-ordinate monitoring of response to OPAT and any drug toxicity. PICC line insertion after appropriate training. Administer intravenous antibiotics to patients using the hospital attendance model. Community nurses Intravenous antibiotics may only be administered by registered nurses with the necessary knowledge and skills in preparing and administering intravenous antibiotics and evidence that they are confident and competent to carry out this practice. Nurses involved in any aspect of administration of intravenous antibiotics have a responsibility to acquire and maintain the necessary knowledge and clinical skills. It is the responsibility of nurse to administer prescribed intravenous antibiotics as per trust policy. Assess patients’ home environments for suitability for OPAT and contact OPAT team if any concerns Antimicrobial Pharmacist: Hospital Antimicrobial Pharmacist can be contact for advice. On discharge hospital pharmacy will provide patients with prescribed intravenous antibiotics, diluents and flushes till their first follow up appointment with Microbiology Consultant at outpatient clinic. Hospital Antimicrobial Pharmacist will periodically review all reconstitution and administration instructions listed on the OPAT drug chart. Any changes will be communicated to all relevant parties. Pharmacy will coordinate further supplies with OPAT nurse and consultant microbiologist. 6 Antimicrobial Therapy: The decision regarding outpatient parenteral antimicrobial therapy is a joint decision made by the clinical team after advice is sought from Consultant Microbiologist/ID Consultant. Apart from sensitivities of the bacteria the following criteria are taken into consideration when deciding therapy. Once daily antimicrobial therapy is the first choice 4 BD antimicrobial therapy is chosen if the clinical condition of the patient enables BD therapy or if this is the drug of choice and this can be facilitated in the community or the Medical Day Unit. (NB not all community teams can facilitate BD regimes and this is considered a limiting factor in some situations). Intermittent infusions longer than 30 minutes or antibiotics that require frequent monitoring cannot be facilitated in the community and would require daily outpatient appointments by the patient. (Drugs in this category include gentamicin and amikacin ) Length of treatment is agreed by clinical team in discussion with the OPAT team. Conversion to oral therapy if appropriate will occur at the end of IV therapy and this is managed by the OPAT CNS in consultation with the clinical team and Microbiologist attached to the referring clinical team. District Nurse administration in the patients home is the preferred method of administration, other options include daily visits to the MDU where the VAN/OPAT CNS would administer the antimicrobials All patients will receive the first doses of antimicrobial therapy in hospital. The hospital will supply all antibiotic, diluents and flushes for the duration of the therapy. In some certain situations the OPAT team may be asked to supply other consumables for patients by community teams. This is funded by the OPAT service as are all consumables required for self-administration. Drugs primarily used in OPAT are: Ceftriaxone, Teicoplanin & Ertapenem. Other drugs used include Amikacin, Gentamicin, Ceftazadime, Meropenem, and Daptomycin. 6 Referrals: Referrals to the service are completed using the OPAT referral form available on the Intranet and emailed to opatandvascularaccess@homerton.nhs.uk . See Appendix 1 for referral process and referral form Clinical conditions that will be considered for the service include: Osteomyelitis Cellulitis Soft tissue/wound infections Joint Infections Endocarditis Any other conditions that require long-term antibiotics will be considered after review. 5 Those patients who live in the Hackney CCG will have the option of home administration by District Nurses or attending the MDU daily. Patients living outside Hackney CCG will be arranged on a case-by-case basis. All patients will be reviewed on a weekly basis by the OPAT Specialist nurse and/or consultant, which includes a full review including blood tests. Transport can be arranged but we would prefer them to make their own way to hospital. Before they can be considered for the service they must be: 1. Fully assessed medically which needs to include relevant swabs/blood cultures for microbiology. 2. Requiring once daily IV Antibiotic regime e.g. ceftriaxone (a bd regime may be considered on a case by case basis) 3. Clinical responsibility remains with the relevant team who will be contacted for follow-up. Conversion to oral therapy if appropriate will occur at the end of IV therapy and this is managed by the OPAT CNS in consultation with the clinical team and Microbiologist 4. IV Antibiotics need to be written as a TTA. Drugs will be stored in the MDU and those to be administered by the District nurses will be supplied directly to the patient on discharge and at each outpatient clinic appointment. IVDU – patients with a history can be accepted onto the service after an individual history is taken and it is agreed by the OPAT team, this is on a case-by case basis. They will be managed with either a daily cannula injection; once again this is on a case by case basis after discussion with the OPAT team. OPAT service will: 1. For patient requiring administration of intravenous antibiotics at home OPAT CNS will liaise with District Nursing Team to arrange for the administration of prescribed antibiotics and fax/email DN referral form and confirm fax has been received. 2. Patients attending hospital for intravenous antibiotic administration will be seen by the OPAT CNS or ICT nurse covering OPAT CNS on the Medical Day Unit. 3. Monitor clinical condition and recommend any antibiotic changes. 4. Refer back to the relevant clinical team for any necessary follow-up. 5. Provide patients with supply of intravenous antibiotics. Patients who require longer than a 6-day course of treatment will be considered for a midline or PICC line; otherwise they will be managed with peripheral cannulae. 6 Referrals can be made by completing the referral form and emailing it to the opatandvascularaccess@homerton.nhs.uk 7 Discharge process and Information: Once a patient is accepted on to the OPAT service and method of administration has been decided the following information sent to the district/community Nurse team. Referral to District Nurses Vascular access device information, including tip position if relevant. Contact numbers including out of hours number. Copy of discharge summary. At least one week’s supply of the drug, diluents and flushes are given to the patient on discharge from HUH with instructions for storage in the home. At weekly review the patient is supplied with further supplies. For patients on OPAT, the OPAT team will request their medical notes from medical records and an entry made detailing that the patient is currently part of the OPAT program. Separate OPAT patient held records will be held by patient. The GP will be sent a copy of the discharge summary regarding their patient informing them of the treatment plan for their patient. If appropriate other letters will be sent by OPAT team throughout the course of therapy if the need arises. At other times it may be necessary to write to consultants of OPAT patients informing or significant changes to treatment as decided due to clinical or environmental need, (e.g. drug reactions, non-compliance), this is copied to GP and /or District Nurse team as appropriate. 8 Vascular Access: The patient will have an appropriate VAD inserted to facilitate OPAT. This decision is made by the CNS in discussion with the patient. Devices that are used are: Peripheral cannula, (primarily for daily OPAT patients requiring short courses of treatment). If the patient is being discharged into the community with a peripheral cannula it is important to check with the relevant community/DN team that they will accept a patient with a peripheral cannula and if so there is a clear pathway for re-insertion should this be required out of hours. Midline cannula: 1. Leaderflex midline, which can stay insitu for 4 weeks, this has a much smaller gauge catheter and is more suitable for short courses of treatment. 7 PICC - suitable for all drug administration. The tip of this line sits in the lower third SVC. (Available in both single and double lumens) Skin tunnelled catheter e.g. Hickman line– suitable for all drug administration and should be considered when a PICC is unable to be inserted. All documentation will be kept within the patients records. 9 Review: All OPAT patients will be reviewed according to clinical need, (minimum of once weekly) by the CNS and/or ID/microbiology consultant, whom will care for the vascular access device, take blood test as determined by the clinical condition of the patient and follow-up the results, informing the clinical team/OPAT team as required. Any other requirements of the patient, e.g. transport, assistance with dressings, further investigations will be done at the discretion of the CNS, liaising with clinical teams as required. For patients on OPAT, the OPAT team will request their medical notes from medical records and an entry made detailing that the patient is currently part of the OPAT program. Separate “Patient held” OPAT records will be held by patient. 10 Discharge: On completion of therapy the patient will be discharged back to the relevant clinical team and/or the GP for follow-up. The timing of this is determined by the patients’ clinical condition and any on-going treatment plan. SOP Review – Mandatory: This policy will be reviewed in 3 years’ time. (Normal review period for a policy is 3 years) Earlier review may be required in response to exceptional circumstances, organizational change or relevant changes in legislation or guidance. 11 12 Monitoring/Audit – In order to examine the quality OPAT service programme, an annual service review report will be produced at the end of every financial year which will include: Clinical outcome measures Patient’s length of stay/ bed days saved Programme outcomes Bacterial outcomes Antibiotic outcomes Adverse events to antibiotic 8 Access device infection Referring team Medical conditions referred Annual activity report: An annual serviced review report will contain activity. Service delivery: The weekly OPAT Clinics will be held in the Out-Patients Department where the CNS and consultant Microbiology/ID will review patients currently receiving treatment. Weekend administration for patients attending MDU will either be done in Medical Day Unit (by community nurses) or in the patient’s own home. Senior Nurse to check capacity before deciding patient can be seen at Medical Day Unit over weekends. 13 OPAT Business Continuity Plan The Trust OPAT team is a small team of staff with specialist knowledge within the field of outpatient parenteral therapy patient management. The team comprises of: Lead OPAT Consultant Microbiologist/Infectious Diseases Consultant Antibiotic pharmacist (Advisory Role) OPAT Nurse , 1 WTE Band 2 infection control team administrator. 0.2 WTE The OPAT Business Continuity Plan would be required if there were severe reduced staff levels and/or long term reduced levels of staff within the OPAT Team or as part of the Trust Business Continuity. The team’s leave is planned to ensure that there is always clinical staff available at an appropriate level. In the absence of Lead OPAT microbiology consultant one of the other 2 consultants will cover the service. In the absence of OPAT CNS there will be limited service for patients wishing to attend Medical Day Unit. Patients will be informed of this when offered the option for intravenous administration at MDU. In the absence of OPAT Nurse Patient will be referred to the community nurses for home IV antibiotic therapy. Infection Prevention and Control Nurse will cover the weekly OPAT clinic in the absence of OPAT Nurse To provide safe and quality care to patients on OPAT register while CNS is away there will be case by case review of patients 2 weeks prior to OPAT CNS’s planned annual leave 9 No new referrals will be assessed/accepted to the service. Normal OPAT service will resume on OPAT CNS‘s return from annul leave. The BCP would need to be considered if the Lead OPAT consultant and OPAT CNS were not available for a prolonged period of time (over 3 weeks). It would also need to be considered if there were to be reduced levels of staffing within ICT for prolonged periods of time, for example if there was no consultant support available due to long term sickness or leave or if one or two of the band 7 infection control nurses were on unplanned prolonged leave. For the purpose of considering this BCP unplanned prolonged periods of leave should include leave of over 4 weeks depending on number of staff involved. Management Action Team members will regularly cover each other’s leave and therefore any specific procedures relating to mandatory requirements will be known to another team member. The impact of any changes in service provision would need to be discussed with the Chief Nurse and the Chief Executive made aware if there are possible risks relating to compliance with statutory requirements (e.g. Health and Social Care Act 2009). The ability to continue to provide service to new OPAT patients requiring assessment would need to be considered and contingency plans put in place. Therefore full service provided by OPAT Team would need to be covered by other means (e.g. locum cover for Consultant/CNS). 10 Appendix 1 OPAT Referral Form Patient name Date of birth Hospital number NHS Number Ward Consultant Date of admission Past medical history Current condition requiring OPAT Planned duration of antibiotic treatment Microbiology team aware of the patient Current IV access Has OPAT been discussed with the patient and they agree to the referral? Please email the referral to opatandvascularaccess@homerton.nhs.uk 11 Appendix 2 Consent for patient to be an OPAT Service patient: Name of Patient Referring Consultant Permission is given by the referring clinical team, after discussion with OPAT team that the clinical responsibility for the patient remains with referring team. Yes No Signature Designation Bleep Date Accepted on to OPAT programme OPAT Clinical Nurse Specialist Date I understand this programme is to facilitate my early discharge from hospital and I agree to return to hospital for my prescribed course of treatment and will contact the service if any problems occur during the course of treatment we have prescribed for you. Patients Signature Date 12 Appendix 3 Patient Held record Patient Name DOB Antimicrobials: From To DRUG Dose/Route/Freq Other medication OPAT start date: Progress & Management Plan: Date/Time Notes 13 14 Appendix 4 15 Appendix 5 OPAT Suitability Assessment Checklist Yes Checklist for patient Informed consent obtained Fully alert and oriented (History of dementia or mental health issues e.g. self-harm) Have access to telephone at home to be able to access help in an emergency Has adequate venous access: IVDU patients are not generally suitable for OPAT service NOK informed Is medically stable and ready for discharge Willing and able to attend hospital for follow ups/ Hospital Transport required? Understand their condition and are able to care for vascular access line (what to do if line comes out and know what to do in an emergency). Checklist for home setting No problems with the home environment: suitable for DN to administer IV antibiotics at home e.g. lighting, cleanliness , water and electricity supply Are there any other know problems with home environment? Is patient on anticoagulation or bedbound Checklist regarding OPAT service Patient supplied with contact details for OPAT & DN (if needed) Patient provided with drug information All supplies and consumables are given to patient if IV antibiotics administered by DN Team at home Patient provided with patient held records including OPAT drug chart Other relevant discharge plans Patients requiring wound management must be referred to district nurses by completing DN referral form Yes/No Print Name: Date: Signature: 16 No