OPAT - Massachusetts General Hospital
advertisement

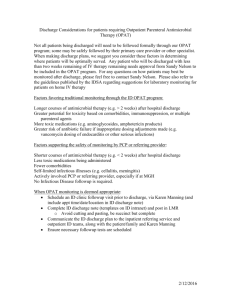
Hospital Discharge and Outpatient Parenteral Antimicrobial Therapy (OPAT) Sandy Nelson, M.D. What is OPAT? • Hospital stays have become shorter, and patients often do not complete their antibiotic courses as inpatients. • Some patients will continue on IV antibiotic therapy after hospital discharge – OPAT = Outpatient Parenteral Antimicrobial Therapy • Yet the antimicrobial treatment still carries risks – – – – Drug related adverse effects Superinfections (e.g. C difficile) PICC line complications (thrombosis, infection, occlusion) Antibiotic intolerances are common • Points of transition are error-prone – Electronic and personal communications minimize errors What is OPAT? • At MGH, OPAT is a system that assists ID physicians in caring for their outpatients on IV antibiotic therapy – OPAT does not replace the care of ID and other physicians, but facilitates it • Active lab tracking and communication of abnormal results • Communication with home infusion services and VNAs • Prompt access to care for problems (NP) • Proactive followup coordination • OPAT cares for approximately 700 patients yearly Preparing for ID signoff • Decide on antimicrobial plan • Determine what care providers will be supervising antimicrobials after hospital discharge: ID (with OPAT) or other • Considerations (see suggestions in handout and online): – duration of therapy, toxicity of antibiotic regimen, risk of antimicrobial failure, comorbidities, involvement of primary or specialist team • Followup in ID is required if OPAT system involved Preparing for ID signoff • First, ask Karen Manning to schedule the followup ID appointment (kmanning3@partners.org) – Appointment will be scheduled preferentially with MGH fellow or any provider who can provide inpatient-tooutpatient continuity – In your appointment request, please also include the desired time frame for the appointment and the anticipated “antibiotic stop date” – Please note the ideal followup appointment is usually 1-2 weeks after hospital discharge (not at the end of a six week course) – Some patients may be scheduled to be seen by one of our clinic NPs ID Discharge Form • Any patient being discharged on IV antibiotic therapy needs an ID discharge note in the chart and in the electronic record • Templates under “Fellow Resources” on ID Intranet – Two forms, depending on whether ID/OPAT will be following the patient after discharge – Be succinct but relay information relevant for decision making, particularly if you will not be following the patient after discharge – Include laboratory monitoring (and goal drug levels if relevant). Suggestions for laboratory monitoring are included in your orientation handouts and online. Be succinct – avoid requesting a BMP if all you want is a BUN and creatinine – Include studies that are still pending and need followup – Avoid cutting/pasting Infectious Diseases Discharge Plan and Sign Off Note Name: MRN: Referring Service/Physician: Malcolm Smith, Orthopedics ID Physician: Sandra Nelson, MD Discharge date/to: 5/12 anticipated to home Primary ID Diagnosis/Diagnoses Osteosynthesis infection – left clavicle Relevant history, hospital course, ID medical decision making, and future considerations: Mr. X is a healthy 52 year old male who sustained a displaced left clavicular fracture last month while skiing, and on 4/22 underwent ORIF with a distal hook plate. He had uneventful postoperative course and was doing well until early May when he noted swelling and some drainage at the surgical site followed by flu-like symptoms. He presented to the ED where he was administered a dose of cefazolin; antibiotics were otherwise held until he went to the OR on 5/8 for debridement. There was purulence within the soft tissues and some fat necrosis which was debrided, the purulence did extend down to the hook plate. Cultures from wound drainage grew CoNS; operative cultures are growing pleomorphic gram positive rods in thio broth I suspect this will be propionibacterium. Current plans call for a six week course of IV antibiotics. He will be discharged on cefazolin, though I may revise this in the outpatient setting depending on final culture results. He does have a history of DVT/PE and is on warfarin for Factor V Leiden heterozygosity. We reviewed with the hematology service that PICC placement would be fine as long as his INR is maintained between 2-3. His INR will need to be closely followed while on antibiotic therapy. Microbiology: 3/6: Wound drainage: CoNS (meth-susceptible) 3/8 OR cultures: pleomorphic gram positive rods Antibiotics and Dose: Cefazolin 2 grams IV q8 Antibiotic Start Date: 5/7/13 Anticipated Antibiotic Stop Date: 6/19/13 contingent upon clinical improvement Allergies: NKDA IV access and date inserted: RUE PICC 5/11/13 Labs and frequency: CBC with differential, LFTs, BUN, Creatinine weekly on Monday or Tuesday Studies related to ID consultation still pending: final operative cultures Fax labs to attention of: Sandra Nelson, MD and Karen Manning at 617-643-2903 Follow-up ID Appointment: 5/23 at 10 a.m. Outpatient Precautions needed: no Communicating the Plan • Post the note electronically in LMR/CAS • Print the note and put into the hospital chart • Communicate the plan verbally and electronically to the primary inpatient team and case manager • Discuss the plan with the patient. If possible provide the patient with your “team card” including the appointment information • Email the note to the outpatient team (ID fellow and outpatient attending, and kmanning3@partners.org) Special Considerations • OPAT does not take over antimicrobial supervision until after hospital discharge – If there are important pending results or monitoring after ID signoff but before hospital discharge, please ensure primary team is aware to follow, alternatively keep a “less active” list to check on periodically • Patients going to SNF or rehab – OPAT will help with the care of these patients if otherwise appropriate for OPAT care • Patients going home on oral antibiotics – With rare exceptions (e.g. high risk patients on linezolid) OPAT will not monitor patients going home on only oral meds Special Considerations • Patients who do not otherwise need ID followup – OPAT will only monitor patients who will be seen in ID followup • Fellow does not have clinic availability in the time frame in which the patient needs to be seen – Discuss with your preceptor, move other patients, utilize NPs at a time you are in clinic • Avoid conflicts over who will supervise antimicrobials – Involve your attending if you sense any issues • Please page or email me with any questions (sbnelson@partners.org)