Antimicrobial Stewardship- Focus on Clostridium difficile Infection
advertisement
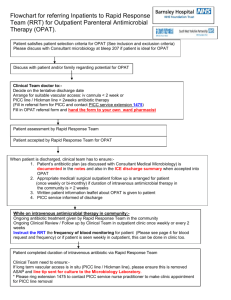
Transition from Hospital to Home Outpatient Parenteral Antimicrobial Therapy (OPAT) Karri A. Bauer, PharmD, BCPS Specialty Practice Pharmacist Infectious Diseases January 16, 2013 Objectives Understand combined benefits to provider and patient of outpatient parenteral antibiotic therapy (OPAT) List key components of a successful OPAT program Review OSUWMC data regarding transition of patients from hospital to home on OPAT Discuss the potential role of an infusion center at OSUWMC Background 1970s- Outpatient parenteral antimicrobial therapy introduced Minneapolis-Canada Community hospital reported successful treatment of > 150 patients with invasive infections 1998- 250,000 people treated, generates $2 billion in revenue Growth rate > 10% annually Emphasis on cost containment Availability of antibiotics administered once or twice daily Advances in vascular access Increased acceptance Increased availability of structured services Background • • • • • Facilitate early discharge Avoid hospital readmission Provide safe, effective, and cost-effective therapy Improve hospital throughput Improve patient satisfaction • Numerous studies have confirmed the safety with appropriate antimicrobial selection and monitoring Key Components Medical director/advisor Defined roles Physician, nurse, pharmacist, and patient Standards Physician, nurse, and pharmacist Accreditation or certification (JCAHO) Experience Policies Reporting of laboratory results Willingness to share local quality assurance and outcomes Willingness to share charge/cost information Key Elements ID Specialist ID Pharmacist Primary care Patient Case manager Nurse Delivery of OPAT Infusion centers Visiting nurse Self or caretaker Long term care facility Selection of Outpatient Antimicrobials Dosage schedules Long-term toxicity Drug stability Drug half-life Patient population Anticipated duration of therapy Patient tolerance Low incidence of side effects Cost effectiveness Home IV Antimicrobial Infusion Therapy 205 patients discharged from a VA Outpatient IV infusion team July 2000-December 2003 230 courses of IV antimicrobials Most patients ≥ 60 years of age DM, CAD, PVD IV therapy team verified that patients could perform infusion at home and provided instructions Osteoarticular (52%), bacteremia (14%), and skin and soft tissue infections (13%) Mostly PICCs Cox Am, Malani PN, Wiseman SW, Kauffman, CA. Home intravenous antimicrobial infusion therapy: a viable option in older adults. J Am Geriatr Soc 2007; 55:645-650. Home IV Antimicrobial Infusion Therapy Vancomycin (46%) and cefazolin, ceftriaxone, and ertapenem used for other infections Nephrotoxicity observed in 10 courses (4.3%) PICC complications common Failures: 9 cases (8%) in patients ≥ 60 years of age and 7 (6%) of patients < 60 years of age Overall, 70 (65%) courses in patients ≥ 60 years of age and 89 (72%) courses in patients < 60 years of age resulted in stable or improved infections Cox Am, Malani PN, Wiseman SW, Kauffman, CA. Home intravenous antimicrobial infusion therapy: a viable option in older adults. J Am Geriatr Soc 2007; 55:645-650. OPAT Outcomes Registry • Provided information regarding treated infections, pathogens, and antibiotics • Allowed sites to compare programs and experience • 24 contributing US sites- >8000 patients, >11000 courses • Osteomyelitis • Vancomycin • Most patients (93%) did not have repeat cultures • • • • 266 patients analyzed 3 experienced therapy failure 4 showed no change Overall adjusted failure rate of 2.5% Tice A. The use of outpatient parenteral antimicrobial therapy in the management of osteomyelitis: data from the Outpatient Parenteral Antimicrobial Therapy Outcomes Registries. Chemotherapy 2001;47(Suppl 1): 5-16. Economics of OPAT IV antibiotic treatment is ~$1000-2500,compared with $200-300 for OPAT/day Benefits Ability to return to work Reduction in cost of nosocomial infections ~5% of hospitalized patients develop an infection during hospitalization Estimate total cumulative cost of >$2 billion annually Outpatient care may reduce expenses, morbidity, and mortality Antimicrobial Stewardship at Transition of Care • Retrospective study 2/14/10-5/14/10 • Cleveland Clinic CoPAT Registry • Structured data entry form (CoPAT form) • No patient can leave the hospital on OPAT without CoPAT filled out • Electronic form requesting ID consultation • CoPAT request • CoPAT approved in 72% and avoided in 28% • 17% oral antibiotics; 11% no antibiotics • No significant differences in ED visits or readmissions when comparing CoPAT avoided vs CoPAT approved Shrestha NK, Bhaskaran A, Scalera NM, et al. Antimicrobial stewardship at transition of care from hospital to community. Infect Control Hosp Epidemiol 2012; 33:401-404. Impact of a Multidisciplinary Team Review of Potential OPAT • • • • • • 2000- Multidisciplinary OPAT team Independent from ASP Review antibiotic care plans at hospital discharge ID physicians, ID pharmacists, and case managers Receive therapy at a variety of non-acute care settings Interventions provided and documented • • • • Patient safety Regimen simplification Clinical efficacy Decreased healthcare expenditures Heintz BH, Halilovic J, Christensen CL. Impact of a multidisciplinary team review of potential outpatient parenteral antimicrobial therapy prior to discharge at an academic medical center. Ann Pharmacother 2011; 45:1329-1337. Impact of a Multidisciplinary Team Review of Potential OPAT • Analysis of impact of OPAT between 7/1/09-6/30/10 • 613 bed academic tertiary care hospital • Electronic form requesting ID consultation • Safety, efficacy, and complexity • Economic benefits (total number of hospital days avoided) Heintz BH, Halilovic J, Christensen CL. Impact of a multidisciplinary team review of potential outpatient parenteral antimicrobial therapy prior to discharge at an academic medical center. Ann Pharmacother 2011; 45:1329-1337. Impact of a Multidisciplinary Team Review of OPAT • Interventions • Regimen safety- 56.1% • Simplification- 40.6% • Efficacy- 28.6% • OPAT was avoided in 13.2% referrals Heintz BH, Halilovic J, Christensen CL. Impact of a multidisciplinary team review of potential outpatient parenteral antimicrobial therapy prior to discharge at an academic medical center. Ann Pharmacother 2011; 45:1329-1337. Impact of a Multidisciplinary Team Review of Potential OPAT Heintz BH, Halilovic J, Christensen CL. Impact of a multidisciplinary team review of potential outpatient parenteral antimicrobial therapy prior to discharge at an academic medical center. Ann Pharmacother 2011; 45:1329-1337. Impact of a Multidisciplinary Team Review of OPAT Heintz BH, Halilovic J, Christensen CL. Impact of a multidisciplinary team review of potential outpatient parenteral antimicrobial therapy prior to discharge at an academic medical center. Ann Pharmacother 2011; 45:1329-1337. Impact of a Multidisciplinary Team Review of OPAT • Discharge delays avoided • 6.2% referrals, resulting in total of 228 days (mean 6.5 days) and $366,000 in hospital bed cost savings • CVC placement prevented in 48 referrals, represents an additional $58,080 in cost savings • $424,080 of direct inpatient care-related costs was avoided over 1-year study period • Mean 27 minutes of ID pharmacist time was required Heintz BH, Halilovic J, Christensen CL. Impact of a multidisciplinary team review of potential outpatient parenteral antimicrobial therapy prior to discharge at an academic medical center. Ann Pharmacother 2011; 45:1329-1337. Transition from Hospital to Home Outpatient Parenteral Antimicrobial Therapy (OPAT) Karri Bauer, PharmD, BCPS Jessica Johnston, MSPH Debbie Goff, PharmD, FCCP OSUWMC and University Optioncare Background • Audit in 2009 completed by Jen Severing, PharmD, BCPS • Evaluate home regimens of nafcillin and piperacillin • Patients discharged with incorrect or ambiguous orders • 30% of nafcillin orders; 24% of piperacillin orders • 26% readmitted for suspected or confirmed ongoing infection 63 70 60 Incorrect/Ambiguous 50 Total 40 30 19 20 17 4 10 0 Nafcillin Piperacillin Background • At OSUWMC, approximately 200 patients per year are discharged to University Optioncare on OPAT • Currently, not every patient discharged on OPAT is seen by an ID physician or ID pharmacist • Collaboration between ID specialists at OSUWMC and pharmacists at University Optioncare provides an unique opportunity to study outcomes • Relationship provides a method for prompt identification of patient care issues and improved access to communication Methods • All patients who received inpatient antimicrobial therapy and were discharged on OPAT (ertapenem +/- additional antibiotic) through University Optioncare between 1/1/1112/31/11 • Patients < 18 or > 89 years of age, prisoners, and pregnant females were excluded • Data obtained from the electronic medical record and University Optioncare database • IRB approved for all patients discharged on OPAT through University Optioncare Results n=100 Age 48 (39-60) Male 53 Service* --UH hospitalist --Colorectal surgery --Gen surgery --Inpatient ID --Urology 9 5 5 5 5 Comorbidities --Diabetes --Chronic renal disease --Malignancy --Chronic respiratory disease --Immunosuppression --Liver disease 18 15 16 15 10 3 *Top 5 services presented Data presented as % unless otherwise stated Results n=100 Infectious diagnosis* --Osteomyelitis --Intra-abdominal --UTI/pyelonephritis --Pneumonia --Bacteremia 21 21 12 7 6 IV access --PICC --Groshong 99 1 ID follow-up upon discharge 60 Combination therapy 31 Median antibiotic duration, days *Top 5 diagnoses presented Data presented as % unless otherwise stated 21 (14-42) Results Organism % Polymicrobial 33 Culture negative 26 MRSA* 6 MSSA 5 Gram negatives** 52 Antimicrobial Agent# % Ertapenem 100 Vancomycin 15 Daptomycin 11 Penicillins 2 Fluoroquinolones 1 *1 patient had MRSA identified as the only organism **8 patients had E coli; 6 patients had ESBL E coli; 6 patients had K pneumoniae #30 patients received combination therapy Results Outcome n=100 Line-related complication 0 Antibiotic-related complication --Intolerance* --Compatibility --Allergy 2 0 0 Change in antibiotic therapy 4 Post discharge antibiotic additions 12 Transition to oral therapy --Osteomyelitis 9 5 Clinical cure 80 Infection-related readmission** 19 *1 patient elevated liver enzymes; 1 patient elevated vancomycin level **Median time to readmission was 50 days (11-133) Data presented as % unless otherwise stated Results • 20 patients did not achieve a clinical cure • 19 patients had an infection-related readmission Infectious Diagnosis n=20 Intraabdominal 6 (20) Osteomyelitis 4 (20) UTI/pyelonephritis 3 (15) Soft tissue 3 (15) Pneumonia 2 (10) Bacteremia 1 (5) LVAD 1 (5) Organism n=20 Gram negative 14 (70) Culture negative 5 (25) Polymicrobial 5 (25) MRSA 3 (15) Results • 20 patients could have potentially received oral antibiotics • 17 patients- no ID consult • 3 patients- ID consult • 3 patients could have potentially received ceftriaxone instead of ertapenem • 3 patients- no ID consult Conclusions • Currently, there is a great emphasis on methods to improve hospital throughput and patient satisfaction while minimizing health care-associated costs • Administration of IV antimicrobials on an outpatient basis has been shown to be safe, efficacious, practical and cost-effective • Future direction of the study is to complete review of all patients discharged on OPAT through University Optioncare and economic analysis • OPAT presents a future direction for OSUWMC and “Create the Future Now” Transition from Hospital to Home Outpatient Parenteral Antimicrobial Therapy (OPAT) Karri A. Bauer, PharmD, BCPS Specialty Practice Pharmacist Infectious Diseases January 16, 2013