Supplementary Appendix This appendix has been provided by the
advertisement

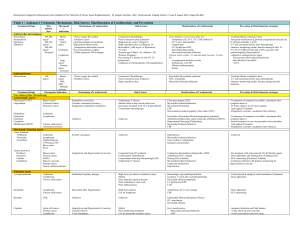
Supplementary Appendix This appendix has been provided by the authors to give readers additional information about their work. Population Study and Protocol Study population Patients who present with chest pain or ischemic equivalents (arm pain, neck pain, jaw pain, shortness of breath, nausea, epigastric pain, etc) within 6 hours of the most recent symptom onset that caused the patient to go to the Emergency Department in whom there is reasonable suspicion for the diagnosis of ACS will be included. Inclusion Criteria coronary syndromes (e.g. chest discomfort/pain, squeezing/fullness in the chest, pain radiating to left or both arms, jaw pain, pain in the back/neck/stomach, shortness of breath, cold sweat, nausea/vomiting, lightheadedness). partment within 6 hours of the onset of the most recent symptoms that prompted the subject to seek medical attention in the Emergency Department. -up. Exclusion criteria etc.) Predetermined Guidelines of the Endpoints Committee “Gold Standard” Diagnosis Once the 30 day follow up has been completed, each CRF will be reviewed by at least two board-certified cardiologists, who will each make a determination of the final diagnosis. All evaluations may be reviewed for consistency by a designated endpoints committee. The final clinical diagnosis will be based on predetermined guidelines. • ST Elevation Myocardial Infarction (STEMI) • Non-ST Elevation Myocardial Infarction (NSTEMI) • Unstable angina • Cardiac but no ACS (e.g. Heart failure, Hypertensive crisis, Takotsubo, Myocarditis, Pericarditis, Arrhythmia, Sepsis) • Non-cardiac chest pain • Unclassified cause of chest pain (no AMI, but UA cannot be ruled out) The cardiac troponin (cTn) results to be used for the Gold Standard Diagnosis evaluation will be provided by the CHOPIN Core Laboratory. These results will be obtained from the plasma that is used in the study for all of the study biomarkers. In patients with incomplete blood draws and therefore e.g. a missing 6 hour draw, the local troponin values are to be used for the assessment. Definitions AMI will be defined as recommended in current guidelines (Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation 2007;116:2634-53.). In brief, AMI will be diagnosed when there was evidence of myocardial necrosis in a clinical setting consistent with myocardial ischemia. Necrosis will be diagnosed by a rising and/or falling pattern of the cTn with at least one value above the 99th percentile with an imprecision of less than 10% (Apple FS, Jesse RL, Newby LK, Wu AH, Christenson RH. National Academy of Clinical Biochemistry and IFCC Committee for Standardization of Markers of Cardiac Damage Laboratory Medicine Practice Guidelines: Analytical issues for biochemical markers of acute coronary syndromes. Circulation 2007;115:e352-5., Apple FS, Wu AH, Jaffe AS. European Society of Cardiology and American College of Cardiology guidelines for redefinition of myocardial infarction: how to use existing assays clinically and for clinical trials. Am Heart J 2002;144:981-6). Clinical Classification of different types of myocardial infarction Type 1 Spontaneous myocardial infarction related to ischemia due to a primary coronary event such as plaque erosion and/or rupture, fissuring, or dissection. Type 2 Myocardial infarction secondary to ischemia due to either increased oxygen demand or decreased supply, e.g. coronary artery spasm, coronary embolism, anemia, arrhythmias, hypertension, or hypotension. ST-elevation MI will be defined as a new ST-elevation at the J point in two continuous leads with the cut-off points: ≥ 0.2 mV in men or ≥ 0.15mV in women in leads V2-V3 and/or ≥ 0.1 mV in other leads. Non ST-elevation MI will be defined as the rise and fall of biomarkers in the setting of ischemia. The ECG may include ST-depression and T wave changes, but does not include STelevation. To define a significant change in cTn values between blood draws for the Core Lab troponin assay to be used for the Gold Standard Diagnosis, the Core Lab will validate the package insert claims and will supply the cardiologists with the slope and instructions on how to interpret the results. Unstable angina will be diagnosed in patients with non-diagnostic troponin levels and typical angina at rest, a deterioration of a previously stable angina, in cases of positive cardiac exercise testing or cardiac catheterization with coronary arteries found to have a stenosis of 70% or greater, and in ambiguous cases in which follow-up information reveals AMI or a sudden unexpected cardiac death within 30 days. Further predefined diagnostic categories include cardiac but not coronary symptoms (e.g. perimyocarditis, tachyarrhythmias), non-cardiac symptoms, and symptoms of unclassified origin. If AMI is excluded in the ED, but no sufficient further diagnostic procedures are performed for conclusive diagnosis, symptoms will be classified as to be of unclassified origin. Role of the Cardiologists Final Assessment of the Patient The two cardiologists from each site will have access to all the information in the case report forms and the medical record. The cardiologists will each perform the case evaluation independently of each other and will be blinded to the other’s evaluation, and the biomarker results being assessed in this trial (BRAHMS biomarkers copeptin, MR-proADM, MR-proANP, CT-proET-1, and procalcitonin). Since their determinations will be the basis for the “Gold Standard” of diagnosis, they will have access to any additional information that becomes available after the patient’s visit to the emergency department. The two cardiologists will make their independent assessments and record this on the “Gold Standard” Diagnosis form. On any cases that the cardiologists disagree, (the “Gold Standard” Diagnosis forms must be in complete agreement for both primary and secondary diagnoses) they will review together, and will attempt to reach a consensus. They may refer back to the medical record and all other additional data available for the case. There must be complete agreement on these items before the data will be coded. If agreement cannot be reached, the case will be adjudicated by the Endpoints committee. Definition of myocardial infarction Criteria for acute myocardial infarction The term myocardial infarction should be used when there is evidence of myocardial necrosis in a clinical setting consistent with myocardial ischemia. Under these conditions any one of the following criteria meets the diagnosis for myocardial infarction: • Detection of rise and/or fall of cardiac biomarkers (preferably troponin) with at least one value above the 99th percentile of the upper reference limit (URL) together with evidence of myocardial ischemia with at least one of the following: • Symptoms of ischemia; • ECG changes indicative of new ischemia [new ST-T changes or new left bundle branch block (LBBB)]; • Development of pathological Q waves in the ECG; • Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality. • Sudden, unexpected cardiac death, involving cardiac arrest, often with symptoms suggestive of myocardial ischemia, and accompanied by presumably new ST elevation, or new LBBB, and/or evidence of fresh thrombus by coronary angiography and/or at autopsy, but death occurring before blood samples could be obtained, or at a time before the appearance of cardiac biomarkers in the blood. • Pathological findings of an acute myocardial infarction. Criteria for prior myocardial infarction Any one of the following criteria meets the diagnosis for prior myocardial infarction: • Development of new pathological Q waves with or without symptoms. • Imaging evidence of a region of loss of viable myocardium that is thinned and fails to contract, in the absence of a non-ischemic cause. • Pathological findings of a healed or healing myocardial infarction. Data analysis Diagnosis: • Improvement in ROC AUC by the addition of copeptin to troponin • Illustration of clinical utility: ROC plots for combined model, ROC for non-diagnostic troponin patients only. • Addition of copeptin to physician assessment of AMI probability • Subgroups analysis for troponin-negative cases and ECG non-diagnostic cases • CART analysis to determine the relative contribution of the markers to diagnostic accuracy Prognosis: • Cox regression model for continuous biomarkers, without and with adjustment for covariates (relevant covariates selected by univariate tests) • Illustration of clinical utility: Kaplan-Meier plots • Time-dependent ROC plots (at 30, 90 and 180 days follow up) Secondary Endpoints/Hypotheses 1. Copeptin improves early diagnostic performance for AMI when used in combination with troponin for the initial blood draw in patients presenting to the emergency department with symptoms consistent with acute coronary syndromes with symptom onset of less than or equal three hours. 2. On the initial blood draw, copeptin is useful in the diagnosis of AMI for patients with nondiagnostic troponin values. Non-diagnostic troponin values are defined as all values below the 99th percentile. 3. In patients presenting to the emergency department with chest pain or ischemic equivalents with symptom onset of less than or equal three hours with non-diagnostic troponin values on the first draw, copeptin values will be predictive of a subsequent positive troponin in AMI patients. 4. Copeptin, Mid Region pro Adrenomedullin (MR-proADM), Mid Region pro Atrial Natriuretic Peptide (MR-proANP), C-Terminal pro Endothelin-1 (CT-proET-1), and procalcitonin are prognostically significant for death, AMI, and revascularization. 5. For patients presenting with symptoms consistent with acute coronary syndromes, the risk of major adverse cardiac events (MACE) is greater among patients in the 4th quartile of MRproADM concentrations than among patients with MR-proADM values in the 1st quartile. 6. Copeptin adds to physician assessment by VAS for AMI diagnosis in the first two hours following presentation to the emergency department. 7. In patients with a non-diagnostic ECG and non-diagnostic troponin, a copeptin level >14 pmol/l on the initial blood draw distinguishes between patients with an AMI and patients with unstable angina or other diagnoses. Non-diagnostic ECG is defined as an ECG with no new significant ST-elevation (ST-elevation at the J-point in two contiguous leads with the cut-off points: ≥0.2 mV in men or ≥ 0.15 mV in women in leads V2-V3 and/or ≥ 0.1 mV in other leads), with no new horizontal or down-sloping ST depression ≥ 0.05 mV in two contiguous leads, and/or with no T inversion ≥ 0.1 mV in two contiguous leads with prominent R-wave or R/S ratio >1. 8. In suspected ACS patients with a non-diagnostic ECG and a non-diagnostic troponin concentration on the initial blood draw, a copeptin level < 14 pmol/l (on the initial blood) can be used to exclude non-ST-segment elevation myocardial infarction (NSTEMI).