Acetylsalicylic Acid Toxicity
advertisement

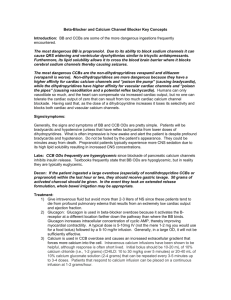
Chapter 147 – Aspirin and Non-steroidal Agents Aspirin Pharmacokinetics Absorption: ASA is rapidly absorbed from the GI tract b/c ASA is in its unionized form in the acidic stomach. Peak serum levels occur at 2 – 4 hrs. Levels may continue to rise for > 12 hrs in large ingestions b/c ASA forms concretions which ↓ dissociation. Distribution: In therapeutic doses, largely protein-bound (overwhelmed with acute OD and chronic toxicity). Low Vd. Metabolism/Elimination: o Small amt is hepatically conjugated with glycine & glucoronic acid o Most is eliminated unchanged in the urine o At therapeutic levels, elimination follows 1st order kinetics, but in overdose elimination is zero order b/c of enzyme saturation Drug is metabolized at a constant rate, regardless of concentration Drug is metabolized at a fixed % per unit time, thus quantity of drug metabolized is concentration dependant Pathophysiology Salicylic acid dissociates at normal pH to salicylic acid (salicylic acid ↔ H+ + salicylate) Therefore ↓ pH → ↑ [salicylic acid]. In its non-ionized form, salicylic acid readily crosses the blood-brain barrier. This means that acidosis promotes entry of salicylates into the CSF, and therefore as respiratory acidosis develops, salicylate toxicity worsens, often with a paradoxical ↓ in serum levels. Chronic Ingestion This occurs more commonly older people due to a number of physiologic changes that promote decreased clearance of ASA and higher levels of unbound ASA. Decreased hepatic blood flow hepatic conjugation Decreased renal function elimination Chronic exposure to ASA leads to albumin binding levels of free (active) drug which cause toxicity with relatively low serum levels. Effects of ASA Respiratory: ASA acts on the central respiratory centres to ↑ the respiratory drive, producing a respiratory alkalosis Prolonged high serum concentrations of ASA eventually depress the respiratory centre, leading to respiratory acidosis Non-cardiogenic pulmonary edema can occur with ASA overdose. Risk factors are: o In adults: age > 30 yrs, smoker, chronic toxicity, neurologic symptoms, ASA > 3 mmol/L o In kids: high serum levels, low PCO2, ↓ serum K+ Metabolic: Mobilization of glycogen stores → hyperglycemia initially. This followed by hypoglycaemia d/t inhibition of gluconeogenesis Uncoupling of oxidative phosphorylation → ↑ anaerobic metabolism with lactic acidosis and ↑ levels of Kreb’s cycle intermediates (pyruvate, ketoacids, organic acids). This process also → heat production Hypokalemia: Occurs through multiple mechanisms o Intracellular shift d/t respiratory alkalosis o Exchange of H+ with K+ in the kidneys as the kidneys excrete HCO3- as compensation for the respiratory alkalosis o Vomiting d/t stimulation of medullary chemoreceptor trigger zone → K+ losses Neurologic: Cerebral edema Tinnitus Diagnosis Any pt with an acute ingestion > 150 mg/kg or symptoms of toxicity and a history of chronic use should be assessed in the Ed. Levels: Serum ASA levels should be obtained 6+ hrs after ingestion. A 2nd level should be obtained 2 hrs after the 1st to ensure that the serum level is not still climbing. Toxic levels: o Acute toxicity: > 3 mmol/L o Chronic toxicity: levels are difficult to interpret Acid-base status Electrolytes & renal function (especially potassium Treatment ABCs: Airway mgmt – avoid intubation if possible… may lead to worsening of metabolic acidosis. If intubation necessary, give Na HCO3- boluses first and ventilator rate post-intubation matches preintubation rate ensure adequate CO2 clearance Decontamination: MDAC is recommended d/t the formation of concretions Supportive Care: Most pts are hypovolemic and almost all require K+ replacement Elimination: Urine alkalization o Increase urinary pH that ASA will be in its ionized form in the urine and thus will not be reabsorbed o Need to correct hypokalemia first or you will not be able to alkalize the urine d/t exchange of H+ with K+ in the tubule o Start with 1-2 mEq/kg IV then infusion at 2x’s maintenance o Add 3 amps NaHCO3 + 40 mEq KCl to 1L D5W to create an isotonic solution o Goals: urine pH 7.5 – 9 & serum pH 7.45 – 7.55 o Follow ASA levels q1-2 hr until consistent ↓ is seen Indications for dialysis Hemoperfusion + hemodialysis preferred for pts with significant toxicity for maximal clearance. Hemoperfusion achieves more effective clearance, but hemodialysis permits modification of electrolytes. In most centres, only hemodialysis is used. Level > 3 mmol/L + end-organ symptoms: o CNS toxicity o Pulmonary edema o Coagulopathy Absolute levels: o Acute toxicity: 7 mmol/L o Chronic toxicity: 4 mmol/L Clinical deterioration despite adequate supportive care Unable to alkalinize urine b/c pt cannot tolerate fluid load (CHF, renal failure) Renal failure Dialysis duration: The necessary length of the run is not well defined. Recommendations are typically 3.5 – 4 hrs with blood pump speeds of 250 – 350 cc/hr. Repeat levels are required after dialysis to ensure adequate clearance. Non-Steroidal Agents Pharmacokinetics Absorption: Rapidly absorbed from the GI tract with peak levels < 2 hrs after ingestion, except sustained release preparations. Weak acid, so unionized in stomach → passage into gastric mucosal cells. Distribution: Highly protein bound with low Vd Metabolism/Elimination: o Primarily hepatic metabolism o < 10% excreted unchanged in urine Classes Salicylate Pyrazolones – phenylbutazone Anthranilic acids (fenamates) – mefanamic acid Acetic Acids (end in ac) – diclofenac, ketorolac Proprionic acids (end in profen) – ibuprofen, ketoprofen, naproxen Oxicam – peroxicam COX-2 Inhibitors (end in ib) – celecoxib, rofecoxib Mechanism of Action Inhibition of cyclooxygengase → ↓ prostaglandin production. COX-1 is responsible for the production of physiologic prostaglandins (hemostasis, GI protection, renal function). COX-2 is an inducible enzyme with ↑ activity in the setting of inflammation. Therapeutic Adverse Effects GI Nausea, vomiting, AP, gastritis, PUD, bleeding Bleeding is d/t direct mucosal irritation + inhibition of cytoprotective prostaglandin production GU ↓ prostaglandins → vasoconstriction with ↓ renal blood flow. This results in ↓ GFR and retention of Na+, K+ and H2O NSAIDs are also a major cause of AIN (immune-mediated) Immun Anaphylactoid reaction (25% of pts with asthma + nasal polyps) Heme ↓ plt aggregation Neuro Confusion, delirium, HA Tinnitus or hearing loss Visual disturbances Aseptic meningitis MSK Fasciulations Metab Anion gap metabolic acidosis CVS Mild hypotension Toxic Ingestions In general, NSAIDs are safe, and cause minimal symptoms even with lg overdoses. The exceptions are: Pyrazolones: Early GI symptoms followed by acid-base & electrolyte disturbances, pulmonary edema, seizures and ↓ LOC, hypotension, cardiopulmonary arrest. MDAC and gastric lavage recommended, as there is no specific antidote Fenamates: Muscle twitching and seizures + GI symptoms Renal failure occurs rarely with significant overdoses in the setting of hypotension. Assessment All pts who have ingested pyrazolones or fenamate should be assessed. For other NSAIDs, doses < 100 mg/kg do not require medical assessment. Pts who have ingested 100 – 300 mg/kg and have symptoms or have ingested > 300 mg/kg (approximately 5x’s the daily dose) should be assessed. Management Decontamination: gastric lavage and MDAC should be considered in pts with pyrazolone or fenamate ingestion. Consider AC for pts with other NSAID ingestions. Supportive Care: Treat hypotension aggressively to avoid renal impairment Enhanced Elimination: No role for HD or HP. Disposition Discharge if asymptomatic x 4 hrs (8 hrs if pyazolone or fenamate)