Review of the Implementation of Care Plus
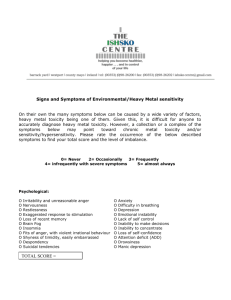
advertisement

Review of the Implementation of Care Plus 22 August 2006 Published in December 2006 by the Ministry of Health PO Box 5013, Wellington, New Zealand ISBN 978-0-478-30714-6 (Internet) HP This document is available on the Ministry of Health’s website: http://www.moh.govt.nz CONTENTS ABBREVIATIONS ........................................................................................................................ IV EXECUTIVE SUMMARY .............................................................................................................. 1 BACKGROUND ............................................................................................................................. 1 IMPLEMENTATION ........................................................................................................................ 1 W HO IS GETTING CARE PLUS? ..................................................................................................... 2 IMPACT ....................................................................................................................................... 2 DISCUSSION ................................................................................................................................ 3 1 BACKGROUND ......................................................................................................................... 6 2 DESIGN OF THE CARE PLUS IMPLEMENTATION REVIEW ................................................. 8 3 IMPLEMENTING CARE PLUS ................................................................................................ 11 PROVIDER PERSPECTIVES .......................................................................................................... 13 Attitudes to Care Plus .................................................................................................. 14 Uptake of Care Plus .................................................................................................... 15 Identifying potential Care Plus patients ....................................................................... 15 DHB PERSPECTIVES .................................................................................................................. 16 DESCRIPTION OF SERVICE DELIVERY MODELS ............................................................................. 17 Payment structures and service models ..................................................................... 17 Impact of funding changes .......................................................................................... 20 Teamwork .................................................................................................................... 21 PROVIDER SURVEY .................................................................................................................... 22 4: WHO IS GETTING CARE PLUS NOW? ................................................................................ 27 PRACTITIONERS’ VIEWS ............................................................................................................. 27 DHB PERSPECTIVE.................................................................................................................... 28 NATIONAL DATA ......................................................................................................................... 29 PRACTICE DATA ......................................................................................................................... 30 Hospital discharges profile .......................................................................................... 34 HUHC patients to Care Plus........................................................................................ 35 ESTIMATING THE POTENTIAL CARE PLUS POPULATION ................................................................. 36 IS THE CURRENT CARE PLUS FORMULA FAIR? ............................................................................. 39 Comparative characteristics of Care Plus patients ..................................................... 39 5 IMPACT OF CARE PLUS ........................................................................................................ 41 PATIENTS’ PERCEPTIONS OF CARE PLUS: IN-DEPTH SURVEY ........................................................ 41 PATIENTS’ PERCEPTIONS OF CARE PLUS: BRIEF TELEPHONE SURVEY ........................................... 42 PROVIDER PERSPECTIVES .......................................................................................................... 45 PRACTICE DATA ......................................................................................................................... 45 Consultation rates ....................................................................................................... 45 Quality of primary health care ..................................................................................... 46 OUTPATIENTS AND EMERGENCY DEPARTMENTS (EDS) ................................................................ 47 HOSPITAL DISCHARGES.............................................................................................................. 48 6 CONCLUSIONS AND IMPLICATIONS ................................................................................... 49 THE ROLE OF THE MINISTRY OF HEALTH AND DHBS .................................................................... 50 THE ROLE OF PHOS AND PRACTICES .......................................................................................... 51 NATIONAL FUNDING ................................................................................................................... 52 DELIVERING CARE PLUS IN THE PRACTICE .................................................................................. 53 W HO GETS CARE PLUS?............................................................................................................ 56 THE KEY ROLE OF NURSES ......................................................................................................... 57 APPENDICES ............................................................................................................................. 60 APPENDIX 1: SUMMARY OF FINDINGS FROM PILOT EVALUATION. ................................................... 60 APPENDIX 2: REVIEW METHODS ................................................................................................. 63 APPENDIX 3: CARE PLUS CONDITIONS ........................................................................................ 69 APPENDIX 5: QUALITATIVE RESEARCH REPORT ........................................................................... 73 APPENDIX 6: PATIENT SURVEY: SUMMARY OF RESPONSES ........................................................... 74 Tables Table 1: Care Plus enrolments at April 2006 ...................................................................... 13 Table 2: Payment structures ................................................................................................. 18 Table 3: Features of payment structures ............................................................................. 19 Table 4: Provider survey response rate ............................................................................... 22 Table 5: Ca r e Plu s p at ien ts, b y ag e and ethn ici ty ............................................................ 29 Table 6: Access and Interim Care Plus rates, by ethnicity ................................................ 30 Table 7: P ra cti ce sam p l e Ca r e Plu s rat es, by ethn icity ................................................... 31 Table 8: P ra cti ce sam p l e Ca r e Plu s ag e by ethn ici ty b rea kdow n ................................... 31 Table 9: Ca r e Plu s c ri te ri a ................................................................................................... 32 Table 10: C a re Pl u s co n d itio n s ............................................................................................ 33 Table 11: C a re Pl u s co n d itio n s ............................................................................................ 34 Table 12: Ho sp it al d isch arg e p ro f ile .................................................................................. 35 Table 13: Estim ated se ve n m o st co m m on ch roni c conditio ns ........................................ 37 Table 14: Nu m b e r o f ch r o n ic co n d it ions ............................................................................ 37 Table 15: Po ten t ial C ar e Plu s p o p u lati on – rev ise d est im ate s ....................................... 38 Table 16: C a re Pl u s p atie n t ‘c lin i cal need ’ su rro ga tes .................................................... 39 Table 17: PM S - b a sed Ca r e Plu s al loca tion t abl e .............................................................. 40 Table 23: C a re Pl u s im p a ct o n co n su ltatio n rat es ............................................................ 46 Table 24: Sam p l e p re sc ri b in g d at a fo r pati ents wi th diab etes ....................................... 46 Table 25: Pr esc r ib in g q u ality - o f - ca r e in dic ato rs .............................................................. 47 Table 27: C a re Pl u s im p a ct o n h o spit al adm is sion r ates ................................................ 48 Table 28: Su m m a ry o f p r actit io n e rs ’ sug gest ions for im p rov ing Ca re Plus ................. 55 Figures Figure 1: Care Plus recruitment, number of patients ......................................................... 13 Figure 2: Expected Care Plus and HUHC shifts .................................................................. 24 Abbreviations CCM chronic care management DHB District Health Board ED emergency department GP general practitioner HUHC High User Health Card OP outpatients PHO primary health organisation PMS patient management system Executive Summary Background Care Plus was rolled out nationally on 1 July 2004 as a new primary health care initiative targeting people with high health needs due to chronic conditions, acute medical or mental health needs, or terminal illness. The programme aims to improve chronic care management, reduce inequalities, improve primary health care teamwork and reduce the cost of services for high-need primary health users. To be eligible for Care Plus funding a patient has to meet specified criteria. Funding is provided to primary health organisations (PHOs) based on a capitation formula and distributed by PHOs to practices in a variety of arrangements. Implementation The concept of Care Plus is supported by most practices (general practitioners and nurses), by PHOs and by District Health Boards (DHBs). Eighty percent of PHOs were delivering Care Plus in some or all of their practices by April 2006. Significant resources are needed for setting up Care Plus, to identify patients that may be eligible for the service and to establish clinical and business processes for delivering Care Plus, both within a practice and at the PHO level. Even in practices that have been delivering Care Plus for some time, enrolment growth has been much slower than expected. By April 2006 only 39 percent (range 3 to 122 percent) of predicted eligible1 patients were enrolled in PHOs that had started Care Plus. Funding models employed by PHOs varied widely. All PHOs received funding according to the national agreement, but varied in the extent of the initial practice payment and how the per visit reimbursement was distributed to the member practices. Although PHOs receive 50 percent up-front funding, ongoing PHO income is dependent on adequate enrolments and HealthPac accepting practice claims. Patient co-payments cited by the practices surveyed ranged from 0 to $42 (242 randomly selected practices). The mean was $6.61, and the median was zero. Eight percent of practices charged more than $30 for a Care Plus visit. Patient co-payments ranged from 0 to $20 in the patient survey (300 patients from 30 practices). Care Plus is equally likely to be delivered by doctors and nurses, either solely or in combination. Eighty-seven percent of practices give patients a Care Plan. Two-thirds of practices surveyed run Care Plus in conjunction with a chronic care management (CCM) programme. 1 ‘Eligible patients’ means the estimated maximum number of potential Care Plus patients for which a PHO received Care Plus funding according to the Care Plus funding formula. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p1 Although there was support for the concept of Care Plus, many practices felt that it is administratively complex, not flexible enough and under-funded (surveyed practices felt a payment of $290 to the practice would meet most concerns about funding). Who is getting Care Plus? Practitioners reported that Care Plus is being targeted at patients with chronic high need. According to DHB and PHO interviewees, easy-to-contact patients are probably enrolled first, so there may be some bias towards patients who already have reasonable access to care within this group. Care Plus may not be well suited to patients who need intense interventions (more than four per year). Māori and Pacific patients appear more frequently than their population rates in Care Plus enrolments, as would be expected from known greater need. Care Plus is generally not being used as a replacement for the High User Health Card (HUHC), although this was an early Ministry of Health expectation. The commonest Care Plus entry criterion is two-plus chronic conditions. Diabetes and ischaemic heart disease are the commonest chronic conditions. Some commonly recorded Care Plus chronic conditions may not have been originally anticipated (eg, hypertension, elevated lipids). A previous estimate2 of approximately 8 percent of the population being eligible for Care Plus was confirmed. The age, gender and quintile distributions of the current Care Plus funding formula were broadly confirmed in an analysis of patient management system (PMS) data from 30 sample practices. Impact Patients felt their care had improved, and in particular that it was more structured. Most patients appreciated having dedicated time specifically to talk about their condition, rather than having discussion about the condition as part of a wider general consultation. Eighty percent of patients received a written Care Plan. Once enrolled in Care Plus, consultation rates increased by an average of four visits per annum compared with the previous year. Based on an analysis of prescribing patterns for specific chronic conditions there is as yet no clear evidence of improvements in prescribing quality for Care Plus patients. Hospital admissions for those enrolled in Care Plus rose 40 percent in the following year. This may have been due to improved monitoring of conditions (and subsequent appropriate referral) and/or the natural history of certain chronic illnesses. 2 CBG Health Research, Care Plus Investigation: Estimating case loads, Prepared for Ministry of Health, 2003. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p2 Discussion The slow uptake of Care Plus, the relative complexity of care delivery with written Care Plans and changes in practice processes and the difficulties some PHOs have experienced managing cash flow mean that Care Plus has taken longer than expected to become incorporated into the day-to-day delivery of primary health care. Nevertheless, the programme is regarded positively by most PHOs, practices, practitioners and patients, and does fill a gap in the range of subsidised services that have been offered by primary health care. Although uptake has been slower than expected, the patients who are enrolled in Care Plus appear to be from the major intended recipient groups, especially those with chronic illness. However, Care Plus is probably not the best method of improving access for patients who need intensive interventions requiring multiple primary health care contacts over a short period of time. Limited funding per patient, and limited space, time and nursing staff, may be reducing the potential uptake and impact of Care Plus. Mechanisms for encouraging the use of pooled resources could be explored, such as providing incentives for PHOs to maintain a Care Plus workforce and operating via referrals or practice visiting. The average fee for a Care Plus visit charged by the sampled practices was $6.However, with some patient co-payments of up to $45, some patients on Care Plus may still be facing a significant financial access barrier. Many practices are embracing a more team-oriented approach to delivering chronic care, which has the potential to lead to improved outcomes, and continued funding through Care Plus will support this paradigm shift. In an environment where some patients without subsidies can be charged high fees (eg, $65) for a consultation, it is only to be expected that some practices will use Care Plus to subsidise a patient visit. In this case the income to the practice might stay the same – the only thing that has changed is the fee barrier faced by the patient. The extent to which improved quality of care is delivered depends on the balance between these competing uses for the funding: how much of the extra resource provided by Care Plus is used to reduce co-payments, increase profit or provide increased resources. Given that increased funding for primary health care is provided from other sources (e.g., extending increased subsidies to adults aged 4564 years), we would expect to see increased Evaluation of the roll out of Care Plus CBG Health Research August 2006 p3 opportunities for more fully implementing those aspects of Care Plus that relate to improved quality of clinical care. It has been noted throughout this review that Care Plus seems to work best, in terms of improved care, when linked to a CCM programme. It was suggested by DHB and PHO interviewees that this might be because of the increased structuring of care that formal CCM programmes require. If Care Plus were to continue it would be worth considering whether some specific elements should be required in order to qualify for funding. Enrolment in a CCM programme could be one requirement, or at least the construction of a detailed Care Plan, possibly with specified components. Although a structured CCM programme is useful for patients with specific conditions, it would also be important to have a generic template available for other Care Plus patients. There will always be high-needs patients (eg, mental health patients or those with disabilities) who do not fit into rigid templates, and such an approach would not be desirable for many conditions. In addition, some chronic conditions would be too rare to warrant a detailed template. However, even a generic template could provide a useful structure for CCM (e.g., for exploring access to social welfare benefits, screening for depression, medication review). Although many providers felt that the level of overall funding for Care Plus should be increased, this review has not found any strong evidence to suggest the Care Plus funding model itself should be significantly altered. Some providers reported difficulties managing cash flow, which might be helped by larger payments, but the general concept of up-front establishment payments was supported, and subsequent staged payments over the year seems sensible (and consistent with all other funding). Earlier estimates of Care Plus numbers have been confirmed, and the general structure of the Care Plus funding matrix has also been validated. It seems clear that Care Plus does not always overlap well with the perceived needs of HUHC patients. Many HUHC patients are regarded as requiring frequent monitoring or episodic care, even if they have a chronic condition. This suggests that it may be desirable to maintain a separate funding stream for these patients, although it may be possible to incorporate these patients into the general capitation funding calculation. In view of the significant concerns about administration overheads and other transaction costs, it may be more efficient to add Care Plus payments to capitation funding, and pay them at some proportion of the estimated total uptake, with regular review of the evidence for improved care from practice data sources, possibly monitored through an enhanced performance management framework. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p4 The philosophical thrust of Care Plus, as a mechanism for facilitating care planning and increasing primary health care teamwork, probably requires a broader range of sector interventions than the current Care Plus initiative. It is notable here that one of the recommendations from providers was that Care Plus visits be aligned with medication repeat visits. Unless a nurse is merely handing a standing order to a general practitioner (GP) to sign, this should be an opportunity to titrate medication3 while reviewing overall management, and this requires prescribing rights. Primary health care nurses need access to short, affordable training courses to allow them to deliver chronic care services most effectively including prescribing. For many patients with chronic conditions, physical access to services is difficult. This also suggests that the development of the nurse home visitor role to undertake chronic care management in the home, which is often the best place to undertake comprehensive needs assessments, could be valuable. A large proportion of chronic care management is concerned with developing strategies to live with a condition, and an assessment of the living situation including social supports, family dynamics and physical environment is often essential. 3 Titration involves adjusting the dose of the medication until the desired effect is achieved. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p5 1 Background Care Plus was rolled out nationally on 1 July 2004 as a new primary health care initiative targeting people with high health need due to chronic conditions, acute medical or mental health needs, or terminal illness. The programme aims to improve chronic care management, reduce inequalities, improve primary health care teamwork and reduce the cost of services for highneed primary health users. To be eligible for Care Plus a patient must be enrolled with a PHO and meet a number of criteria, as follows. The potential Care Plus patient is assessed by a doctor or nurse at their general practice as being able to benefit from ‘intensive clinical management in primary health care’ (at least two hours of care from one or more members of the primary health care team) over the following six months, and either: has two or more chronic health conditions, so long as each condition is one that: is a significant disability or has a significant burden of morbidity; and creates a significant cost to the health system; and has agreed and objective diagnostic criteria; and continuity of care and a primary health care team approach has an important role in management; or has a terminal illness (defined as someone who has advanced, progressive disease whose death is likely within 12 months); or has had two acute medical or mental health-related admissions in the past 12 months (excluding surgical admissions); or has had six first-level service or similar primary health care visits in the past six months (including emergency department visits); or is on active review for elective services. PHOs receive Care Plus funding as a separate funding stream. The amount a PHO receives is determined on the basis of estimated numbers of Care Plus patients, which is calculated from the size and demographic profile of a PHO’s register. Nationally, funding has been allocated to cover 5 percent of the population, but this varies at the PHO level from 3.2 to 9.5 percent. The exact form in which Care Plus is being delivered varies from PHO to PHO, and even from practice to practice within a PHO. In general, a Care Plus patient can expect to receive an extended initial appointment with a nurse or doctor, in which their health needs are explored in more depth than is possible in a normal consultation. One of the features of this consultation will Evaluation of the roll out of Care Plus CBG Health Research August 2006 p6 be the development of a Care Plan. After this initial consultation, it is expected that a patient will be seen on at least a further three occasions over the next year, usually to monitor their ongoing care. Care Plus was developed as a result of a proposal from the Independent Practice Association Council (IPAC) in 2002 to improve access to services for people with high health care needs who might be relatively disadvantaged by the newly established Access and Interim PHO funding formulas. The scheme was originally conceived as a method of delivering targeted funding at ‘priority patients’. The Ministry of Health worked closely with provider groups, and IPAC in particular, to develop the Care Plus proposal into the form in which it was rolled out to PHOs. Key events in developing Care Plus were4: the development, in consultation with IPAC, of preliminary proposals for service delivery and funding based on the distribution of high-needs patients, derived by examining general practice records in three PHOs during 2003/04 external evaluation of the pilots’ three reports: September 2003, December 2003 and March 2004 (see Appendix 1) setting up the Care Plus reference group in October 2003, with membership from PHOs (both Interim and Access), District Health Boards New Zealand, Royal New Zealand College of General Practitioners, Independent Practice Associations, First Health, Net Care and Health Care Aotearoa to advise on service specifications, a funding formula and a process for national roll-out running six Ministry-led regional workshops to help prepare PHOs and DHBs for Care Plus in South Auckland, West Auckland, Rotorua, Wellington, Christchurch and Dunedin during March 2004 using feedback from individual pilots, workshops and evaluations to fine-tune the Care Plus funding formula and services specifications a joint PHO, DHB and Ministry of Health agreement to changes to contracts for Care Plus (April and July 2004) 25 PHOs entered the three-month preparatory phase for Care Plus on 1 April 2004. By 1 July 2004, 43 out of 73 PHOs were being funded at some stage of Care Plus development. At that stage the Ministry commissioned a review of the national implementation of Care Plus, which was carried out by CBG Health Research, after some delays due to the slow roll-out of Care Plus, between November 2004 and May 2006. 4 See: http://www.moh.govt.nz/primaryhealthcare Evaluation of the roll out of Care Plus CBG Health Research August 2006 p7 2 Design of the Care Plus Implementation Review This review of the implementation of Care Plus was commissioned by the Ministry to get answers to three broad questions: Is Care Plus reaching those individuals with high primary health care need? What are the effects of the Care Plus programme? What are the best ways of organising and delivering Care Plus services? Prior to undertaking this review of the national implementation of Care Plus, CBG completed a review of the 2003/2004 Care Plus pilots. A summary of the findings is provided in Appendix 1. The key issues for the roll-out, as perceived by practitioners then, were: the payment for the time required to deliver Care Plus as intended, including Care Plans and in-depth reviews of conditions, was not sufficient. for some practices there was no financial incentive to change HUHC patients to Care Plus delivery of Care Plus required significant training of nursing staff in some practices there was resistance to allowing nurses to practise autonomously the transfer of HUHC patients to Care Plus meant loss of prescription subsidies. The level of patient involvement in Care Plus expected by practitioners varied from practice to practice. The main barriers to implementation experienced in the pilots were described as the large time commitment required for both patients and practitioners, patient lack of interest in intensive monitoring, and the lack of staff to deliver Care Plus services. Two patient groups were identified as less likely to engage with Care Plus: older males and the very elderly. Most practices thought there should be a Care Plus nurse co-ordinator at the PHO and/or national level. The majority of pilot practices thought that Care Plus was not an easy scheme to run in the busy and time-restricted environment of general practice. Getting the right staff involved in the Care Plus programme at a practice level was the strongest determinant for successful implementation. Nurses appeared to take a lead in care planning in most practices, but the input of GPs and nurses in Care Plus visits, particularly reviews, was varied and constrained by funding, time, and the extent to which practices supported autonomous nursing practice. Establishing the number of nursing and GP hours required in relation to patient numbers and implementing a plan to stagger the introduction of the programme were also seen as factors contributing to success. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p8 During the pilots, some practices experienced problems with patient drop out, sometimes as high as 50 percent at the follow-up review stage. The reasons for this included lack of active recall for review appointments, negative perceptions of nursing consultations, and Care Plus being offered at limited times because of the need for extra nursing cover. While these findings contributed to the design of the current project, this national implementation review is focused on how well Care Plus is reaching those individuals with high primary health care needs, and on understanding the overall impact of the programme. Data were collected from: patient focus groups PHO case studies DHB interviews Ministry of Health interviews key informant interviews with practices in participating PHOs PMS and clinical management analyses PMS data extract correlation with hospital discharge data in the National Minimum Dataset secondary care utilisation review from hospital records (emergency departments and outpatients) a computer-assisted telephone survey (CATI) of 300 patients a survey of 250 providers. More details on the methods employed are provided in Appendix 2. The selection of the PHO and practice participants for the focus groups and interviews was undertaken in consultation with the Ministry, in order to get a representative sample of providers covering small and large PHOs, Access and Interim, and urban and rural. Twelve PHOs were chosen, and within each PHO a practice was invited to take part in the focus groups to explore how Care Plus was implemented on the ground. Practices invited 24 Care Plus patients to take part in four patient focus groups to describe their experience of Care Plus. Representatives of the seven DHBs that contracted with each PHO were also interviewed. All qualitative research was conducted by an experienced researcher who was familiar with the development of Care Plus. The findings of interviews were supplied to participants for validation. From each PHO two to three practices were chosen to build a sample of 30 practices for further research. Each of these practices invited the next 10 Care Plus patients they saw, after a nominated start date, to take part in a phone interview with a researcher, for which they received a small koha. These same practices provided downloads of data from their PMS, which could be used to assess the impact of Care Plus and how well it was achieving its original Evaluation of the roll out of Care Plus CBG Health Research August 2006 p9 goals in terms of targeted assistance. National Health Index numbers were forwarded to the New Zealand Health Information Service to extract hospital discharge dates and codes for registered patients of these practices from the National Minimum Dataset. This data was used to assess the impact of Care Plus on secondary care utilisation, and specifically on ambulatorysensitive hospitalisations. These same National Health Index numbers were supplied to the seven DHBs, and a record of outpatient (OP) and emergency department (ED) attendances was requested. The last piece of research was a survey of 250 randomly selected general practices, asking questions about the implementation of Care Plus in each practice. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 10 3 Implementing Care Plus Key points The concept of Care Plus is supported by most practices (GPs and nurses), PHOs and DHBs. Eighty percent of PHOs were delivering Care Plus in some or all of their practices by April 2006. Significant resources are needed for setting up Care Plus to identify patients who may be eligible for the service and to establish clinical and business processes for delivering Care Plus, both within a practice and at the PHO level. Even in practices that have been delivering Care Plus for some time, enrolment growth has been much slower than expected. By April 2006 only 39 percent (range 3122 percent) of predicted eligible5 patients were enrolled in PHOs that had started Care Plus. Funding models employed by PHOs vary widely. All PHOs receive funding according to the national agreement, but there are variations in the extent of the initial practice payment and how the per visit reimbursement is distributed to the member practices. Although PHOs receive 50 percent up-front funding, ongoing PHO income is dependent on adequate enrolments and HealthPac accepting practice claims. Patient co-payments cited by practices surveyed ranged from 0 to $42 (242 randomly selected practices). The mean was $6.61, and the median was zero. Eight percent of practices charged more than $30 for a Care Plus visit. Patient co-payments ranged from 0 to $20 in the patient survey (300 patients from 30 practices). Care Plus services are equally likely to be delivered by doctors and nurses, either solely or in combination. Eighty-seven percent of practices give patients a Care Plan. Two-thirds of practices surveyed run Care Plus in conjunction with a CCM programme. The Ministry devoted significant resources to helping DHBs and PHOs to implement Care Plus. As mentioned earlier, the concept itself was originally proposed by IPAC, and the details of the Care Plus programme were developed in close collaboration with the Care Plus reference group, representing a wide range of health sector stakeholders. The Ministry held a series of workshops around the country to assist DHBs and PHOs with their Care Plus planning. All publications, discussion documents and summaries of the workshop findings were available on the Ministry of Health website. 5 ‘Eligible patients’ means the estimated number of potential Care Plus patients for which a PHO received Care Plus funding according to the Care Plus funding formula. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 11 Before a PHO could receive Care Plus funding they were required to undertake a three-month preparatory period. PHOs received a small base allocation ($11,000) plus $1.14 per eligible PHO enrollee to assist them with the required tasks, which were to: set up PHO systems – including PHO-wide billing systems for claiming Care Plus payments, training PHO staff about Care Plus, (in some cases) developing Care Plan templates, and establishing teams to help practices deliver Care Plus set up practice systems – including systems for identifying patients, setting up Care Plus clinics, and establishing protocols for Care Plus reviews help identify Care Plus patients – constructing lists of possible Care Plus patients, either from practitioner memory of patients or from queries of PMS (this often involved merging various sources of information and was not necessarily an easy task) train practitioners – particularly when implementing CCM programmes, so that practitioners knew how to complete Care Plans, print them out and fill in templates complete business plans (for subsequent approval by the DHB) notify and consult on fees – to reach agreement between PHOs and practices on the schedule for payments (these were wide and varied) complete, and have approved by the DHB, a Care Plus plan. Twenty-five PHOs entered the three-month preparatory phase for Care Plus on 1 April 2004, and by 1 July 2004 43 out of the then 73 PHOs were being funded at some stage of Care Plus development. When a PHO commenced delivering the Care Plus programme they were paid 50 percent of the annual allocation according to the funding formula6 up-front, with payment of the remainder contingent on Care Plus enrolment rates. Growth in Care Plus enrolments has been steady, although slower than anticipated, as discussed later in this section. By April 2006 64 out of the then 81 PHOs had commenced the programme, and in those PHOs 39 percent of the estimated eligible patients had been enrolled in Care Plus. The following table shows the populations in these groups of PHOs. Seventy-nine percent of all registered patients in New Zealand were enrolled in a PHO that had started Care Plus; nationally 32 percent of the estimated number of Care Plus patients were enrolled. The ‘residual’ column is calculated as the number of estimated Care Plus patients, less the number of HUHC patients. 6 See Appendix 4 for details of the Care Plus funding formula. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 12 Table 1: Care Plus enrolments at April 2006 N 81 Population 3,909,791 Eligible1 CP 212,178 HUHC 63,447 Residual Care Plus not HUHC 148,731 Enrolled Care Plus2 46,959 % eligible enrolled 32 All PHOs Care Plus 64 3,128,001 166,865 45,890 120,975 46,959 PHOs Care Plus PHO data 79% 80% 79% 72% 81% (100%) as % of all 1 ‘Eligible’ means the Care Plus population a PHO is funded for under the current funding formula 39 N.a. (approximately 5.4 percent of the PHO population). 2 Care Plus patients are only from PHOs delivering Care Plus; the top line shows the uptake of Care Plus based on the nationally eligible population (ie, all PHOs). The pattern of enrolment is shown in Figure 1. Different numbers of PHOs contribute to each bar as more PHOs rolled out Care Plus (42 in January 2005, increasing to 64 in April 2006). Figure 1: Care Plus recruitment , number of patients , for PHOs implementing Care Plus Percent of target 50 40 30 20 10 0 Jan 05 Apr 05 Jul 05 Oct 05 Jan 06 Apr 06 The rate of uptake of Care Plus nationally reflects both the size of the PHOs that commenced Care Plus at various times and their rate of uptake. Provider perspectives Focus groups and interviews were held with the doctors and nurses providing Care Plus (see Appendix 2 for full details of the methods used). Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 13 Attitudes to Care Plus Overall, practices and PHOs were very supportive of the concept of Care Plus. It was viewed as a significant improvement in the delivery of primary health care, providing access to services it had not been previously possible to access, or financially viable for practices to provide. We can get them in more regularly, and ensure that they get the care and medications at the same time. However, participants differed in their views of the purpose of the programme. Some of the doctors and nurses interviewed regarded Care Plus as an important case management initiative that could enhance the patientpractice relationship and could become the basic model for delivering all chronic care. Others perceived that it was simply offering low-cost access to GP services for chronic care patients. In this instance, there appeared to be more interest in Care Plus as a funding stream as opposed to a system of care. Many participants perceived the programme as being a link between Access- and Interimfunded practices, which meant all practices could offer increased access for high-needs patients. We have been right behind it from the start. It’s a bridge between Access and Interim funded practices. Practices and PHOs varied greatly in their organisation and delivery of Care Plus. Most described a nurse/GP-focused model, with varying degrees of involvement of other professionals. Some explained that Care Plus is nurse driven, with GP input. Others described Care Plus as GP driven, with or without the help of nurses. At the practice level practitioners often planned Care Plus visits to coincide with patients’ medication requirements. PHOs varied in the priority they assigned to Care Plus as a replacement for HUHC. Some reported that it had not been a high priority relative to other initiatives, and that they had not actively encouraged the transfer of HUHC patients onto Care Plus. Others viewed Care Plus as a higher priority, and provided funding incentives to encourage practitioners to transfer HUHC patients. These were the organisations that strongly supported Care Plus as a new model for chronic care. At the time of provider interviews (late 2005), seven of the twelve selected PHOs were implementing Care Plus as part of an existing or new CCM programme. The programme was typically targeting people with diabetes, chronic obstructive pulmonary disease, cardiovascular disease, asthma and arthritis. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 14 Uptake of Care Plus PHOs reported wide variations in the proportions of practices delivering Care Plus (25 to 96 percent), and within practices there were even wider variations in practice enrolment figures (0 to 80 percent of estimated Care Plus patients). There is no doubt that overall the uptake of Care Plus has been slower than anticipated. Participants thought that practices with some spare capacity (ie, not extremely busy), good IT systems, experience with other chronic care programmes, and enthusiastic practice staff more readily embraced Care Plus. Practices with more limited resources, including IT and nursing staff, had been slower and required more support to start the programme. PHOs that had been involved in the Care Plus pilots have higher rates of enrolment and more developed Care Plus systems. All of these organisations had linked Care Plus to a CCM system. Some had previously failed to reach quarterly targets, but at the time of interview most expected to have enrolled their full quota within the next six months. Identifying potential Care Plus patients Most practices used their knowledge of their patients and information contained in the PMS to identify eligible patients. The selection of Care Plus patients is mainly left to the practitioners, who described some use of subjective criteria when choosing patients for Care Plus. Most explained that they would usually consider social status and patients’ own motivation to decide who would most benefit from reduced fees or the Care Plus approach. The doctors pick them up through their records when they come in. It’s also who can afford to come and who can’t. It’s targeting those people that can’t afford to come to the doctor. The majority of practitioners reported that they had opportunistically recruited Care Plus patients when they presented for routine visits or telephoned to obtain a prescription. They saw the advantage of this method being that it fits within current practice workloads. The key disadvantage was the extra time required to manage the introduction of the concept within the scheduled consultation period For us it’s been opportunistic but some have targeted and invited using the systems. Few PHOs and practices reported specifically inviting patients, by letter or phone call, to enrol in the programme. Of those that did send out invitations, most felt that few patients had responded immediately, but that they or the practitioner had instigated the enrolment at the next surgery visit. We did send out letters to the eligible patients as a first step. Then, they would come in to see the doctor and usually they would then be recruited. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 15 To date, organisations advised that the chronic care enrolment criteria (more specifically, the conditions diabetes, chronic obstructive pulmonary disease, cardiovascular disease, asthma and arthritis) are commonly used to enter patients into the programme. PHO managers also advised that practitioners have enrolled patients who have had hospital admissions and/or are awaiting elective surgery. However, there appears to be little or no active use of ED/hospital lists, as few organisations had received them from hospitals/DHBs. Participants said they preferred to select from PMS or practice knowledge of the patients. The chronic conditions has been by far the most popular criteria …a small number of elective services waiting criteria. This was a very natural use of quarterly visits, given that prescriptions for chronic illnesses are usually issued every three months. If Care Plus visits didn’t coincide with re-issuing prescriptions, the patient would need a further visit, or at least a phone contact, to have their medication renewed. In addition, the issuing of new prescriptions is the natural time to discuss medication dose titration or other alterations. DHB perspectives Representatives from the seven DHBs contracting with the 12 PHOs selected for closer study were interviewed. DHB representatives were also supportive of Care Plus as a concept. They generally regarded it as a fairly centrally driven initiative (ie, from the Ministry), with limited input from DHBs. The views of the DHB representatives mirrored the range of views from PHOs and practices: some viewed it as an important disease management approach, while others treated it simply as a mechanism to lower the cost of GP access. DHB representatives felt that the definition of Care Plus is critical. They reported that PHOs that had regarded Care Plus as a mechanism to lower access costs had not seriously focused on implementing teamwork and/or a patientcentred / care-planning approach. Most reported that within the DHBs, staff expected the programme would become increasingly important because of its association with chronic care. Four of the seven DHBs had approved Care Plus as part of their CCM programmes. These organisations expressed the most support for Care Plus. Representatives from regions where no such CCM/Care Plus alignments were apparent were not as supportive of the programme. These participants reported lower levels of PHO engagement and commonly felt Care Plus implementation had come on top of a range of other Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 16 services. This group conveyed that they left the PHOs to decide whether to be involved in Care Plus without attempting to persuade them in any way. Some participants reported that Care Plus had met with some cynicism because of IPAC’s involvement in its conception. These representatives felt that DHBs were not sufficiently included in the early discussions and subsequent negotiations with PHOs. They perceived that, following the non-performance of many PHOs, the Ministry had handed Care Plus problems over to regional bodies. DHB representatives were able to report on the progress of all PHOs in their regions. They all reported that PHOs in their areas were at different stages of organising and delivering Care Plus, and were doing so under various service models and with different levels of success. They explained that the majority had fallen below targets, with few exceeding them. Commonly, participants observed that many organisations who were implementing the philosophy of Care Plus as a system of care delivery were requiring more time to embed it into general practice. Description of service delivery models Payment structures and service models PHOs differed in the way they were administering Care Plus funds to practices. Patient copayments ranged from no charge to $20 per visit, and some practices charged less than the possible maximum fees agreed with PHOs. They pay $14. We are Interim funded, so that is really good. Not all practices and PHOs were willing to provide details of Care Plus co-payments and/or the precise amounts paid to practices with respect to the payment structure. Some PHOs simply stated that the fees were within the Ministry specifications and patient co-payments were not above $20 per visit. The two tables below outline the different payment models. Table 2 outlines the payment structures in order of complexity, along with the stated rationale for the system. Table 3 relates the models to the size of the PHO, alignment with any CCM system, degree of teamwork, and level of financial risk to the PHO. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 17 Table 2: Care Plus Payment structures Simple models Equal fee-forservice payments P Up-front loaded; two payments per annum E Up-front loaded; fee-for-service payments P Payment structure Practices are paid equal amounts for each visit. Payments made on a quarterly basis are based on one initial invoice detailing enrolment. Practices are paid a large initial payment ($150) to enrol patients and complete the first visit based on one initial invoice detailing enrolment. They then receive one further payment to cover follow-up visits. Practices are paid a large initial payment to enrol patients ($80) and complete the first visit. Smaller subsequent quarterly payments are paid on submission of invoices for each visit. More complex models One up-front Practices receive an up-front capitation capitation payment, based on payment for their allocated Care Plus quota practices’ Care and on signing a memorandum Plus quota ($30 of understanding to undertake per patient); the programme. Subsequently, four equal feepractices are paid equal for-service amounts for each visit on payments submission of invoices for each P visit. Mixed fee-forPractices receive a quarterly fee service and for Care Plus. The PHO also capitation provides them with a capitation model top-up to give HUHC capitation for all Care Plus patients. E Up-front loaded; Practices receive a large initial mixed fee-forpayment to enrol patients in service CCM CCM and/or Care Plus and and Care Plus complete the first visit and CCM payment templates. Smaller subsequent quarterly payments are paid on E and P receipt of an invoice. Up-front loaded; Practices are paid a larger initial uncapped fee– payment ($45) to enrol patients for-service and complete the first visit. model for Care Smaller subsequent quarterly Plus patients payments ($20) are paid on without other submission of invoices for each subsidies visit. Practices receive extra monies ($15) per visit for Care Flexible funding Plus patients without other for extra subsidies. At any stage in the services Care Plus process, practices can claim extra service Evaluation of the roll out of Care Plus CBG Health Research August 2006 Rationale for use The model was selected to reduce the amount of paperwork for practices and to simplify the administration from the PHO’s perspective. The model was used exclusively by very small PHOs to reduce the administration workload. Staff perceived that the larger first payment would encourage nursing input into the initial stages of Care Plus. Staff perceived that this model had encouraged nursing input into the initial stages of Care Plus. The model was perceived to be uncomplicated for the practices who forward a monthly invoice for Care Plus. The initial capitation payment was seen to cover a practice’s fixed overheads and encourage the employment of any extra staff. The alignment of this payment to a signed memorandum of understanding was advocated as a way to formally obtain a practice’s ‘buy in’ to complete the programme. This is a model used by larger organisations that have merged Care Plus and HUHC funds to give practices capitation payments. In this way, they ensure that practices can earn exactly the same amount for Care Plus as they would for HUHC. This model was selected to encourage practitioners to enrol CCM patients onto Care Plus (there is a higher payment for dual enrolment, as opposed to Care Plus only). Care Plus funding forms the basis of the CCM system funding. This model was used by larger organisations that have merged Care Plus and HUHC funds to give practices capitation payments. In this way, they ensure that practices can earn exactly the same amount for Care Plus as they would for HUHC. The model also ensures that all patient copayments are the same as those for Community Services Card holders. It also provides for the involvement of other professionals and services in Care Plus, through the flexible funding of extra services. p 18 E payments of $80 per patient to purchase extra services. Practices could elect to group the extra service payments for all Care Plus patients. Notes: E = electronic-based claiming system; P = paper-based claiming system. Table 3 shows that the more complex payment structures were devised by the larger PHOs, who have commonly aligned Care Plus with an existing or new CCM system. However, some smaller PHOs are involved in more complex payment structures because of Care Plus/CCM alignment, while some of the larger organisations have opted for simple payment structures with the aim of reducing the administration burden. Table 3: Features of payment structures Model PHO size* CCM system: yes/no Level of teamwork Equal fee-for-service payments Small and large No Low Up-front loaded, two payments per annum. Small No High Up-front loaded; fee-forservice payments Small and medium No Low but evidence of nurse involvement Low but evidence of nurse involvement Medium Yes High High Mixed fee-for-service and capitation model Large Yes High High Up-front loaded; mixed fee-for-service CCM and Care Plus Small, medium, and large Yes Low Medium More complex models One up-front capitation; equal fee-for-service payments Up-front loaded; uncapped Large Yes High fee-for-service model and flexible funding * Based on the number of practices: small: 12; medium: 219; large: 20 plus. Level of financial risk held by PHO High Medium High All the payment models contained some financial risks for the PHOs. Models at either end of the complexity spectrum appeared to carry the highest risk, for different reasons. The less complex models pay practices based on an invoice system, often in the absence of an effective means of tracking actual activity. If the practice does not complete the PMS records properly, HealthPac will not subsequently reimburse the PHO for those patients in the next quarter. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 19 It’s a funding nightmare. If they do not fill out the form correctly to HealthPac, we lose out. The practice has already been paid. Those at the other end of the spectrum, employing reasonably complex capitation/fee-forservice models, recognised that these funding schemes did not fit well with the Ministry payments. Representatives explained that managing cash flow has proved to be a real issue because of the popularity of the schemes for A37, 2564-year-old patients. Managers believed there were two drivers of the situation: (a) the payment schemes provide some financial benefits for this patient group; and (b) there is a perception among practitioners that Care Plus is a chance for early intervention for younger patients with chronic conditions. A3 patients, 2564-year-olds: there is a financial advantage to the patient, not the doctors, if you put them on Care Plus. PHOs that had given practices larger up-front or initial payments thought this had encouraged nursing input into Care Plus. However, payment of equal amounts for each visit was thought to have led to some GPs viewing Care Plus as a funding stream for reduced-cost routine GP consultations. The equal funding means funding for cheaper GP visits. Some won’t involve the nurses at all. There were some risks associated with up-front payments in that it takes a few Ministry payments before PHOs break even. Most had been able to cover deficits from the initial 50 percent up-front funding reserves. The Care Plus/CCM payment scheme was described as cumbersome because patients must be divided into those who are part of CCM and Care Plus, Care Plus only or CCM only. It’s been a nightmare. We get information from the DHB on those in CCM. We get invoices from the practices and now a copy of every enrolment which we enter into a spreadsheet. Impact of funding changes All but two of the PHOs reported they had had to reduce Care Plus funding for at least one calendar quarter. The majority reported they had been able to use the 50 percent up-front funding reserves to cover any cash flow deficits. However, all noted that those funds were depleting rapidly, and if targets were not attained subsequent financial penalties could threaten the viability of the programme. We are bordering on real financial risk now because we have tried to maintain the integrity and philosophy of it all. It’s a real risk for us now. 7 ‘A3’ is used to refer to an unsubsidised adult patient Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 20 Larger organisations that had employed capitation in their payment scheme reported that the funding changes had greatly affected them. There appeared to be three main causes of the difficulties. Firstly, they had designed the project roll-out to control cash flow, not to fit the national funding and/or meet the new targets. Secondly, the sheer scale of some projects meant a small change greatly affected numbers. Finally, such models have attracted a greater enrolment rate of A3 patients (those without access to other subsidies) than anticipated. When the funding changes happened, these PHOs were behind the required coverage and had funds withheld. Typically, PHOs restricted Care Plus enrolments to stem cash-flow problems resulting from project growth in the affected quarter. There has been an enormous uptake in this group [under-65 and over-25]. There are a lot of people who need help in that category. We are not happy about the restrictions, but they were necessary. Teamwork The level of teamwork happening around Care Plus service varied. The highest levels of teamwork (ie, where there was evidence of other allied professionals and services being involved in Care Plus) were associated with some form of funding incentive. These models had provided practices with some up-front funding and/or the flexibility to access extra service payments. Such payments had been used to secure extra practitioner time (nurse and GPs), as well as funding the involvement of pharmacists, dieticians, podiatrists, counsellors, optometrists, physiotherapists, specialists, social workers and dermatologists (although the practice survey showed that use of additional staff was rare). Podiatrists, exercise programmes, and a chunk have been used for more doctor or nurse visits. We have nurse and GP teams but we also involve a nutritionist for many of the patients. PHOs appear to have promoted the involvement of other service professionals in three ways. Firstly, this was done by encouraging Care Plus as a basis of care for other service initiatives such as disease-state management nursing, outreach programmes, exercise provision, prescribing review projects, and/ or the Get Checked programme. Secondly, they provided separate funds out of the Care Plus budget, which could be used to involve other services and/or professionals. Referrals to outreach, rehabilitation, exercise classes, and so on ... patients love that we all talk with the doctor, share information. Finally, obtaining some form of practice buy-in to the programme via agreements (verbal or written) and subsequent up-front payments appeared to be a good first step towards getting practices to take a team approach. Representatives of PHOs using models that had provided specific payments for practices to involve other services or professionals reported that this Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 21 proved popular with many practices who engaged a variety of other professionals. Those that had been able to involve pharmacists observed that this professional group, in particular, have a lot to contribute to Care Plus. Flexible funding is crucial. It has been an incentive for the GPs to take part and involve others. It’s front-end loaded [and] that matches the service model. Others reported little or no involvement of external services and/or other professionals. Typically, they explained that the patients could not afford to access other services, and Care Plus monies were not sufficient to cover the cost. Some representatives advised that there was limited access to many services in certain areas. All participants noted that Care Plus’s demands on professional time (particularly nurses) and the cost of accessing external professionals are barriers to the ideal of teamwork in Care Plus. It’s nursing time really, that’s the key thing – sometimes we just don’t have sufficient nurses to be able to do it. Provider survey A survey of 300 randomly selected practices was planned as part of the review. Only practices in PHOs that had started Care Plus were surveyed. The survey asked questions about patient charges and a number of business processes, and there was some wariness about responding. The survey was conducted at the same time as GP groups were in discussion with DHBs about levels of co-payments for general medical services. The following table describes the response rate. Table 4: Provider survey response rate Group N Percent Contacted 366 Declined 49 14 Still considering participation 74 20 Replies received 243 66 Thirty-three percent of respondents were Access funded. The provider survey showed that, on average, a practice received $185 per annum for each Care Plus enrolment. Some practices (five) received a bulk grant based on a presumed Care Plus patient load. A handful of practices received different funding for patients under 65 years old. Eighty-seven percent of practices gave fees information. Some of the remaining practices simply left the section blank, but some also described how their complex funding arrangement Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 22 could not be easily represented by summary figures. The range of quoted Care Plus fees was 0 to $42, but the average was only $6.61 and the median was zero. Eight percent of practices charged more than $30. All but one of these practices was an Interim-funded practice. Care Plus was delivered by doctors and nurses equally. In 5 percent of practices the programme was nurse only, and in 5 percent it was doctor only. In the remaining 90 percent of practices Care Plus was GP-led in half and nurse-led in the other half. Ninety-six percent of practices were using Care Plans, but only 87 percent gave the patient a printed copy. Sixty-eight percent of practices were using Care Plus in conjunction with a chronic disease management programme. Half of the practices got support from their PHO with administration of Care Plus and the provision of materials. A quarter of practices received help identifying patients, and a quarter received help through a PHO-funded nurse. The services provided by PHO nurses varied, and included assistance with setting up systems for identifying patients (eg, running programmes to identify patients on the PMS), the development of Care Plans and/or explaining how a Care Plan works, and instruction regarding claiming for Care Plus patient visits. PHOs suggested targeting specific patient groups (eg, diabetes patients, HUHC) in 20 percent of practices, while the remainder applied the normal broader Care Plus criteria. The survey asked what proportion of HUHC patients practices expected to move to Care Plus in the next 12 months. The responses clearly showed two different views of Care Plus, with replies bunched around zero and 100. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 23 Figure 2: Percentage of HUHC patients practices that PHOs intend to move to Care Plus Percent of HUHC patients practices 60 50 40 30 20 10 0 0-19 20-39 40-59 60-79 80-100 The national data shows there has been a small reduction in HUHC numbers since Care Plus was implemented, but the large majority of practices see these as two distinct patient groups. Two-thirds of practices felt the Care Plus payment they received was inadequate. The average payment practices felt would be adequate was $290 (range $200 to $400 – some practices were receiving $160 per patient). One practice suggested $3 per minute as a benchmark for any project. Practices that were not happy with the level of funding considered the payment being offered was not sufficient to cover the costs of delivering the range of services expected in a Care Plus consultation. Practices that did not consider the Care Plus payment adequate were significantly less likely (p < .005) to employ extra staff, and the fees they charged were lower than practices that considered the payment adequate. They were no less likely to have implemented Care Plus using doctors or nurses, nor was there any relationship with whether or not their PHO had provided services. A third of practices had increased staff for Care Plus. The additional staff member was nearly always a nurse, at an average of 0.3 FTE, although this figure was probably raised by some practices employing a full-time nurse on a short-term contract to set up Care Plus. One practice employed a 0.25 FTE GP; no other practices employed additional GP time. Other additional staff mentioned by role were administrative and a dietician. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 24 The survey collected free-form comments about Care Plus. There was a 2:3 proportion of positive versus negative comments, although even negative comments were usually within a supportive context. The concept of Care Plus was strongly supported: Fits well into our Practice. Care Plus is a positive initiative for encouraging chronically ill to manage their conditions. Good idea much better than HUHC. Gives the patient the subsidy prospectively when extra input is required. Likely to require more nurse time as numbers increase. However, some practices were unhappy with the implementation process: A lot of extra work. HUHC seemed to be a pretty good system. Seems to be much improvement for patients. Find it administratively top heavy, not very easy to understand for not much return. Confusing to implement in terms of changing documentation, procedures and unreliable reports eg pts omitted and irrelevant pts added. Some practices were supportive of Care Plus but felt they didn’t have the spare space, time or nursing capacity to implement it properly: Very time consuming for existing staff. Too much cross over with existing programmes eg, diabetes reviews. Very busy surgery with little time to book in Care Plus patients. Care Plus has been looked at positively by our Medical Centre twice we have limited space and staff. Would not be able to commit to it with existing personnel. This is a good role for a community nurse. The business realities of trying to run a profitable practice were also mentioned in the free text replies: Like all Primary Health Care initiatives, it fails to build in profit essential in privately owned businesses. Under the funding model we stand to lose $30K pa currently 5.5% HUHC. CarePlus is not wise business. It ultimately costs money and it creates jobs with no extra return for the Practice. Return to HUHC still more profitable. Needs to be worth more financially for all of the extra work. The initial 210 should be paid directly to the practice and then practice audited if necessary. In practices that had employed extra nurses, Care Plus was enthusiastically endorsed as improving patient care: Excellent patient care good results and those patients who ‘buy in’ and attend all of their appointments receive constant monitoring and support. Fits well with Chronic disease management programme. Excellent way of encouraging and facilitating a team Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 25 approach. Helps to keep pts as well as they can be which may well lower their cost of accessing the system through provision of consistent primary care guidance and intervention. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 26 4: Who is Getting Care Plus Now? Key points Practitioners reported that Care Plus is being targeted at patients with chronic high need. Easy-to-contact patients are probably enrolled first, so there may be some bias towards patients who already have reasonable access to care within this group. Care Plus may not be well suited to patients who need intense interventions (more than four per year). These patients face standard fees for their non-Care Plus visits. Māori and Pacific patients appear more frequently in Care Plus enrolments than their population rates, as would be expected from known greater need. Care Plus is generally not being used as a replacement for HUHC, although this was an early Ministry of Health expectation. The commonest Care Plus entry criterion is two-plus chronic conditions. Diabetes and ischaemic heart disease are the commonest chronic conditions. Some commonly recorded Care Plus chronic conditions may not have been originally anticipated (eg, hypertension, elevated lipids). A previous estimate8 of approximately 8 percent of the population being eligible for Care Plus was confirmed. The age, gender and quintile distributions of the current Care Plus funding formula were broadly confirmed in an analysis of PMS data from 30 sample practices. This section addresses the question, ‘Is Care Plus reaching those individuals with high primary health care need?’. The views of providers and DHBs are presented first, followed by an analysis of national data from PHO data uploads. Finally, practice data is examined to provide more detail about consultation rates and the morbidity profile of Care Plus patients. Practitioners’ views Most health practitioners of those involved in delivering Care Plus in the practice felt that Care Plus is reaching patients with high primary health care needs, and that this is because the programme targets those with chronic illnesses. Most viewed the programme as an excellent approach for these patients, given the increased contact time and lower co-payments. Most PHOs reported good uptake of Care Plus by people from deprived areas, and by Māori and Pacific people, and this seems to be reflected in the ethnicity profile of Care Plus patients from practice downloads. 8 CBG Health Research, Care Plus Investigation: Estimating Case Loads, Prepared for Ministry of Health 2003. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 27 There was a fairly even split regarding the suitability of Care Plus for either mental health patients or people with terminal illness. Some did not believe Care Plus was a good option for either group, and considered that the intensive care required by these patients, often over short periods, did not fit well with the Care Plus model. They also believed that specialist teams, rather than primary health care professionals, were better placed to co-ordinate care in these areas. The data (presented later) on the diagnoses of people enrolled in Care Plus shows that people meeting these mental health and terminal illness criteria were very uncommon reasons for Care Plus enrolment. Care Plus is designed for long term not intense stages of life. Others disagreed, perceiving Care Plus as a good option for both mental health patients and/or terminally ill people. They considered that the programme could effectively relieve the financial burden for both groups. Proponents also anticipated that there are periods where specialist care is not required, and during such times Care Plus can provide patients with more access to primary health care professionals at a reduced cost, and can provide the opportunity to plan their own care. There is a period where Care Plus could be good until more intensive, specialist help is required. Māori and Pacific practitioners described Care Plus as being closely aligned with the holistic service philosophy of many Māori and Pacific providers, with the flexibility to incorporate a whānau or outreach approach to service delivery. These practitioners said they had been able to involve outreach services in Care Plus to provide some care in the home environment for those who did not seem comfortable in the clinic environment. Interestingly, another smaller group of participants viewed Care Plus as an individually focused model of care and thought that, as such, it was best suited to a European audience. It is likely that these differences in perception reflect the manner in which Care Plus was implemented in particular PHOs. DHB perspective DHB representatives also felt that Care Plus was reaching or could reach people with high primary health care needs. There was a caution that the requirement to reach enrolment thresholds may have resulted in practices enrolling those who were easiest to contact and enrol, with the perverse outcome of increasing inequalities in some areas. The harder to reach ones are more difficult to enrol. To get the numbers up, they could be going for those who are easier to enrol. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 28 DHB representatives observed that there was a tendency for organisations that serve the highest-need populations to have the least developed infrastructures to support and track Care Plus activity, such as Māori and Pacific providers and ‘third sector’ providers. Those that have the systems to capture the information are largely the old IPAs who typically serve a lower need population. It’s those that serve the highest needs that have less infrastructure, [and] pay for all of Care Plus because they can’t track what’s happening. DHB representatives also commented that it was difficult to assess the implementation and impact of Care Plus in the detail they would have liked due to the rudimentary nature of the data they received in aggregated PHO reporting. National data An analysis of national Ministry of Health data9 from the April 2006 PHO registers shows that there were 46,965 Care Plus patients enrolled nationally, with approximately equal numbers of Care Plus patients in the 4565 and 65-plus age groups. A breakdown of this data by ethnicity shows that most European Care Plus patients are over 65, whereas most Care Plus patients of other ethnicities are aged between 45 and 65. Table 5: Care Plus patients , by age and ethnicity Ethnicity Age group (years) 04 Asian European Māori Not stated Other Pacific Total 33 128 57 3 5 70 296 514 27 122 73 4 16 98 340 1524 24 311 127 12 17 107 598 2544 505 2571 1148 85 121 1149 5579 4564 1690 9801 3669 320 261 3954 19,695 65+ 1099 15,178 1921 226 170 1863 20,457 Total 3378 28,111 6995 650 590 7241 46,965 Nationally there are slightly more females enrolled in Care Plus (54 percent), and this is true in all age groups except for the 600 Care Plus patients under 15 years old. The breakdown of Care Plus patients by practice funding model in Table 6 shows that Access practices have greater proportions of Care Plus patients enrolled in all ethnic groups. For example, in Access practices 3.14 percent of Pacific patients are enrolled Care Plus patients, whereas only 1.87 percent of the Pacific patients in Interim practices are enrolled in Care Plus. 9 Anonymous raw data from PHO register uploads for 2006 Q1. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 29 Table 6: Access and Interim Care Plus rates , by ethnicity Ethnicity Other Māori Pacific Asian All Access 1.70% 1.55% 3.14% 1.78% 1.87% Interim 0.95% 1.05% 1.87% 0.90% 0.92% The national data for PHOs that have started Care Plus shows a gradual reduction in the number of HUHCs as Care Plus is progressively implemented. Figure 3 shows very clearly that Care Plus is not being treated as a replacement for the HUHC. Figure 3: Care Plus and HUHC compared to target (PHOs implementing Care Plus only) No. of patients 60,000 50,000 40,000 30,000 HUHC 20,000 Recruited to CP 10,000 Apr 05 Jul 05 Oct 05 Jan 06 Apr 06 Practice data Data downloaded from the 30 practices in the practice sample provides much more detailed information than is available from the national data set. Initially this data is analysed to described the demographic features of the Care Plus population in the sample. This allows us to assess how representative it is of the national Care Plus population. After these demographic breakdowns further analyses are presented, looking at reasons for enrolment and morbidity profiles. Table 7 shows that Care Plus is reaching Māori and Pacific clients at greater rates than for ‘Other’ population groups, closely reflecting the national data. The average Care Plus proportion for all ethnic groups is 2.52 percent, but for Māori the figure is 3.66 percent and for Pacific Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 30 peoples 3.96 percent. With the data available it is not possible to say whether these percentages are more or less than would be expected on the basis of increased need. Table 7: Practice sample Care Plus rates, by e thnicity Care Plus patient? No N Yes % N All % N Ethnicity Other 122,607 97.75 2816 2.25 125,423 Māori 29,344 96.34 1115 3.66 30,459 Pacific 10,851 96.04 448 3.96 11,299 Asian 14,298 98.69 190 1.31 14,488 All 177,100 97.48 4569 2.52 181,669 Table 8 considers only Care Plus patients, and examines the age-by-ethnicity structure of this group. As with the national data set, the outstanding feature of this table is that half the ‘Other’ ethnicity Care Plus group are aged over 65, whereas for the other three ethnic groupings half the Care Plus patients are aged 4564. Table 8: Practice sample Care Plus age by ethnicity breakdown Ethnicity Other N % Māori N % Pacific N % Asian N All % N % Age (years) <6 18 0.6 9 0.8 5 1.1 - - 32 0.7 6–18 17 0.6 10 0.9 7 1.6 3 1.6 37 0.8 19–44 305 10.8 136 12.2 68 15.2 35 18.3 544 11.9 45–64 977 34.7 574 51.5 248 55.4 102 53.4 1901 41.6 65+ 1498 53.2 385 34.6 120 26.8 26.7 2054 45.0 All 2815 100.0 1114 100.0 448 100.0 191 100.0 4568 100.0 Evaluation of the roll out of Care Plus CBG Health Research August 2006 51 p 31 Data from the PMS was also downloaded from the Care Plus criteria data tables. (These show the criteria under which a specific patient was deemed by the clinician to qualify for Care Plus.) As reported in the interviews with providers and PHOs, by far the commonest criterion was that a patient had two or more chronic conditions. Clinicians could enter as many criteria as they wished. The commonest combinations are presented first, followed by an analysis by single criterion mentions. All patients had to qualify as needing intensive clinical management. Table 9 shows that in 81.2 percent of Care Plus patients (3551 out of 4372) there was only one other criterion for Care Plus two-plus chronic conditions. Overall, however, two-plus chronic conditions was mentioned for 94 percent of all patients, in many different combinations of criteria. Table 9: Patients’ Care Plus qualifying criteria Commonest criteria and combinations Two or more chronic conditions Has had 6 first-level service primary care visits in the past 6 months and has had 2 or more chronic conditions Is on active review for elective services and has had 2 or more chronic conditions Has had 6 first-level service primary care visits in the past 6 months Is on active review for elective services Has had 2 acute non-surgical admissions in the past 12 months and has had 2 or more chronic conditions Other Total Any mention regardless of combination 2+ chronic conditions 6 visits / 6 months Active review 2 non-acute surgical Terminal illness N 3551 % 81.2 274 137 115 88 6.3 3.1 2.6 2.0 48 157 4372 1.1 3.6 100 N 4105 472 280 108 62 % 94 11 6 2 1 It appears that Care Plus is not being used to provide increased care for patients on ‘active review’ and for those with a terminal illness. There are approximately 25,000 people on active review nationally, and it was anticipated that Care Plus could be used to reduce the costs of review visits for these patients. From a population of 180,000 one would expect around 1100 patients; the 280 patients identified above represent 25 percent of the expected number of patients on active review these practices would have. However, it should be noted that some of these patients may have been entered into Care Plus as ‘2+ chronic conditions’. When a person is enrolled in Care Plus the conditions a person has that are relevant to their Care Plus enrolment are recorded (Read coded) 10 in the PMS. This data was extracted from the 10 “Read” codes are used to record diagnoses in primary care information systems Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 32 30 practices in the sample and is shown in Table 10. There were over 12,000 individual conditions recorded for the 4569 Care Plus patients. The first 10,000 of these (starting with the most common codes) were amalgamated into the broad Read Code categories shown in the table. Table 10: Care Plus qualifying chronic conditions Disease type N % Hypertension 1861 18.4 Diabetes 1846 18.3 Ischaemic heart disease 853 8.5 Elevated lipids 754 7.5 Asthma 581 5.8 Arthritis 373 3.7 Other heart disease 322 3.2 Congestive heart failure 314 3.1 Chronic obstructive pulmonary disease 273 2.7 All other conditions were less than 2.7 percent. The full table for any condition that appeared more than five times is given in Appendix 3. The number of recorded conditions is shown in Figure 4. As can be seen, 94 percent of patients have more than one Care Plus condition recorded, and 3 percent have six. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 33 Figure 4: Number of Read codes recorded as Care Plu s conditions Percentage of Care Plus patients 50 45 40 35 30 25 20 15 10 5 0 1 2 3 4 5 6 Number of Care Plus conditions recorded Table 11 examines the pattern of nominated conditions for the top four diagnoses, for the subset of Care Plus patients who have exactly two diagnoses and were recorded as qualifying for Care Plus under the ‘two plus chronic conditions’ criterion. The table shows that hypertension and elevated lipids are frequently entered with diabetes and ischaemic heart disease. Table 11: Common Care Plus chronic condition combinations Diabetes IHD N 855 337 And BP N 487 115 % 57 34 And lipids N 115 50 % 13 15 Note: IHD = ischaemic heart disease. The analysis was restricted to these four conditions because they clearly illustrate the phenomenon. There will be many other examples in other combinations. The qualifying criteria are quite specific: expected to need ‘intensive clinical management’ (two hours-plus) over the next six months. Hypertension and hyperlipidaemia would not normally fit these criteria on an ongoing basis, although it is entirely feasible for initial management and stabilisation to be reasonably time consuming. Some clarification around expectations regarding hypertension and elevated lipids being considered qualifying conditions may be required. Hospital discharges profile Data from the National Minimum Dataset was also examined. This shows some differences in the primary diagnosis discharge coding between Care Plus and other patients registered at the Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 34 sample practices, as shown in Table 12. Care Plus patients have more ambulatory-sensitive hospitalisations as a proportion of total discharges, and the diagnosis profile is more biased towards chronic conditions. Table 12: Hospital discharge profiles for Care Plus patients Rank 1 2 3 4 5 6 7 8 9 10 Care Plus Primary diagnosis Non-ASH Angina Ischaemic heart disease Diabetes CORD Congestive heart failure Cellulitis Respiratory infections Skin cancers Stroke N 6221 602 363 330 275 205 155 131 121 111 % 68.18 6.6 3.98 3.62 3.01 2.25 1.7 1.44 1.33 1.22 Non-Care plus Primary diagnosis Non-ASH Angina ENT infections Cellulitis Gastroenteritis Asthma Respiratory infections Dental diagnoses Ischaemic heart disease Kidney/urinary infection N 84,487 3030 2227 1853 1519 1465 1331 1122 1098 896 % 79.58 2.85 2.1 1.75 1.43 1.38 1.25 1.06 1.03 0.84 Notes: ASH = ambulatory-sensitive hospitalisation; CORD = chronic obstructive pulmonary disease; ENT = ear, nose and throat. This data illustrates features of the patients that practices have enrolled in Care Plus. This pattern is what one would expect given the targeting of Care Plus at patients with chronic conditions, and provides another, independent, data source to confirm this targeting. HUHC patients to Care Plus PHOs viewed Care Plus as more suited to a capitation environment than a separate item of service fee (an alternative possible funding model) and felt that it was a better approach than HUHC for the majority of high-needs patients. Practitioners representing practices that were using HUHC as well as Care Plus often viewed Care Plus as an option for those patients with high primary health care requirements that would not otherwise qualify for HUHC. They saw Care Plus as an opportunity to provide all high-needs patients with more services at a lower cost (without necessarily changing the services provided). Care Plus is of key benefit to those that don’t qualify for HUHC; high needs/low income. Everyone advised that there were high-needs patients who were genuine high users and required more visits than the Care Plus allocation. Such patients face the usual fee at all their non-Care Plus visits. Some felt that Care Plus patients were disadvantaged relative to HUHC patients because there is no transfer of benefits, such as reduced prescription costs, if the patient has to visit another service. Four visits is not suitable for all. If HUHC was stopped you would need some other funding to compensate practices for those who consult more often. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 35 Care Plus are the ones that you want to get in and are not accessing. HUHC is those that are accessing too often. Two different groups as I see it. Access-funded organisations often noted that the number of HUHC holders has never represented the true disease and/or utilisation burden in their patients (ie, not all/many chronic care patients ever qualified). Therefore, practice staff had not specifically targeted HUHC patients for Care Plus (although they may have qualified under other search criteria). These interviewees viewed Care Plus as the better system, but indicated they were uncertain as to the future of HUHC, and if or when Care Plus would supersede the older system. We have not really pushed HUHC; it’s a lot of paper work. This works a lot better better care. Interim-funded practitioners thought that Care Plus does not always effectively compete with HUHC, which in many instances provides more income for less work. These interviewees thought there are few incentives for them to transfer HUHC patients to Care Plus. They explained that patient co-payments are lower and practice income is higher from HUHC. There is no benefit for the practice or the patients for that [HUHC transfers to Care plus] to occur. Some participants, representing larger PHOs that were proponents of the original Care Plus concept, viewed it as a clinically superior tool to HUHC in terms of its targeting and evidence base, even while recognising that some practices would prefer the HUHC for economic reasons. These representatives noted that their organisations have sought to phase out HUHC by using payment structures that promote the transfer of HUHC patients to Care Plus. In our view, Care Plus is a clinically superior tool to HUHC. We want to kill off HUHC as far as possible. Estimating the potential Care Plus population The data collected from practices could be used to estimate the potential number of Care Plus patients in the 30 practices in the sample. The method employed is the same as that used in the evaluation of the Care Plus pilot, and the same assumptions are used. To work out how many patients have two or more chronic conditions, the Read codes recorded in the PMS were examined and prescriptions were analysed for certain common conditions. Table 13 shows the percentages of patients who have the seven most common chronic illnesses. For three of these (asthma, diabetes and ischaemic heart disease) the table shows the estimates based on prescribing patterns, and the ‘Either’ column shows the calculation using both data sources. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 36 Table 13: Estimated seven most common chronic conditions Read code Prescribing Either N % N % N % 10,035 5.% 13,403 7.4 17,611 9.7 Hypertension 8894 4.9 8894 4.9 Diabetes 4518 2.5 3970 2.2 5414 3.0 IHD 3168 1.7 3134 1.7 4803 2.6 CHF 881 0.5 881 0.5 7542 4.2 7542 4.2 128 0.1 128 0.1 N = 181,669 Asthma Mental health COPD Notes: IHD = ischaemic heart disease; CHF = congestive heart failure ; COPD = chronic obstructive pulmonary disease. Table 14 shows the distribution of the number of chronic conditions: 7490 patients had two or more chronic conditions, from a total population of 181,669 patients, equating to 4122 per 100,000, compared with the previous estimate of 4379 per 100,000 in the evaluation of the Care Plus pilot practices. If hypertension is excluded from the list of chronic conditions, the estimate of the number of people with two or more chronic conditions is 2391. Table 14: Number of chronic conditions for Care Plus patients Number of chronic conditions 1 N % 28461 15.7 2 5972 3.3 3 1247 0.7 4 231 0.1 5 37 0.02 6 3 0.00 The next calculation required is to count how many patients have been seen six or more times in the last six months. The distribution of visits is shown in Figure 5. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 37 Figure 5: Patient consultations in last six months Frequency 35,000 30,000 25,000 20,000 15,000 10,000 5,000 0 1 2 3 4 5 6 7 8 9 10 11 12+ Number of visits A total of 13,501 of 181,669 patients had six or more consultations in the last six months (or 7432 per 100,000). Once again, this estimate is close to the estimate made in the evaluation of the pilots. The final value that could be updated from this data is the HUHC rate for patients not already counted in other categories. Table 15 provides an estimate of the Care Plus case load using this new data. The new estimate is 8.4 percent (the estimate from the pilot practices was 8.5 percent). Table 15: Potential Care Plus population – revised estimates 1 2 3 4 5 6 Pop = 100,000 6 or more visits Inflation for ED (+5%) 2+ acute non surgical admits 12 mths Terminal care 2 or more chronic conditions Less already in 1 Leaving On ‘active review’ HUHC in no other group N 7432 8175 996 162 4122 1254 2868 1738 648 Intensive clinical management Total Care Plus 50% 4088 50% 100% 498 162 Notes From PMS ED guess; GP estimate GP estimate GP estimate Max (GP estimate, PMS) 75% 50% Total 2151 869 648 8416 GP estimate PMS (or 8.4%) Note: Bold values are updated figures from the latest sample of practices. As discussed above, some of the conditions that have been used to allocate Care Plus funding, and in turn are incorporated into the estimate of the total number eligible for Care Plus, might Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 38 not be appropriate qualifying conditions. The main two of these are hypertension and hyperlipidaemia. In Table 15, hypertension has been included as a chronic condition. If hypertension is excluded, the estimate of those eligible for Care Plus reduces to 7.2 percent. Is the current Care Plus formula fair? Comparative characteristics of Care Plus patients To see how Care Plus is targeting particular patient groups, we examined the practice data by ethnicity, deprivation quintile, whether a patient had two or more chronic conditions, whether a patient had had six or more visits in the previous six months, and whether they had a current HUHC (expiry date less than one year ago). Table 16: Care Plus patient ‘clinical need ’ surrogates Practice subgroup (N = 181669) % not Care Plus % Care Plus % all 1.2 3.2 2.5 46.8 1.3 4.4 4.1 37.5 5.0 18.5 22.0 11.2 29.0 34.2 19.3 18.8 22.4 11.5 HUHC 2 or more chronic conditions (from 7 tested) 6 or more visits in last 6 months Quintile 5 Māori or Pacific Māori or Pacific and quintile 5 Note: HUHC = High User Health Card Table 16 shows that 1.3 percent of the sample practices’ population have an HUHC, and 2.5 percent of the enrolled Care Plus patients have an HUHC. The commonest reason for qualifying for Care Plus was two or more chronic conditions (94% percent, see Table 9. Table 16 shows that about half of all Care Plus patients have two or more of the seven common chronic conditions. The deprivation quintile and ethnicity profiles are consistent with known morbidity patterns, and also show that the sample of patients overall is a good match to the national population. Table 17 uses the data in the PMS (two or more chronic conditions and six or more visits in the last six moths) to derive estimates of the likely numbers of Care Plus patients in each age group, gender and ethnicity, and quintile 5 cell. The estimates are slightly higher than those of the current Care Plus estimation table (Appendix 4), with the exception that children under five have higher estimates (the high percentage is because of high visiting rates) and the female and male figures are reversed for the older age groups. Otherwise agreement is quite good. For example, the estimate for the number of patients in the 65+, Male, M+P, quintile 5 cell is 38.5 percent versus 41 percent in the current allocation table. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 39 The pattern of values is more important than the actual values because they can be scaled so that the total estimated Care Plus population equals 5 percent (or whatever figure is agreed) of the total. Table 17: PMS-based Care Plus allocation table Age Gender Non M+P Non M+P M+P M+P (years) Quin 14 Quin 5 Quin 14 Quin 5 F 04 5.39% 6.86% 5.88% 7.45% 6.96% 6.23% 5.85% 7.18% 514 M F 0.85% 0.98% 0.66% 1.17% 1.34% 1.22% 1.73% 1.42% 1524 M F 3.32% 3.34% 3.50% 3.11% 1.20% 1.70% 1.49% 1.46% 2544 M F 4.15% 6.41% 6.16% 7.19% 2.19% 3.59% 4.26% 4.70% 4564 M F 10.2% 22.0% 19.9% 24.1% 8.05% 14.8% 12.5% 21.9% 65+ M F 27.6% 40.3% 36.1% 45.6% M 25.2% 38.8% 35.7% 38.5% Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 40 5 Impact of Care Plus Key points Patients felt their care had improved, and in particular that it was more structured. Patients appreciated having dedicated time specifically to talk about their condition, rather than including it in a general consultation. Eighty percent of patients received a written Care Plan. Consultation rates increased by an average of four visits per annum for Care Plus patients. There was no clear evidence of improvements in prescribing quality for Care Plus patients. Hospital admissions increased by 40 percent for Care Plus patients. Patients’ perceptions of Care Plus: in-depth survey The 24 patients who took part in the in-depth interviews represented those most conscious of their involvement in Care Plus and actively engaged in the process (see methods, Appendix 2). They had all received an invitation to enrol in the programme under the chronic condition criteria. Most reported that practitioners approached them opportunistically and they had accepted the offer of extra care at a lower cost. Many of those interviewed described feeling privileged to be invited into the programme. On their initial introduction to Care Plus, participants recalled being told that it would give them extra care and monitoring, improve their health, and provide regular visits at a reduced cost. No one recalled any preamble from practitioners about goal-setting, Care Plans and/or nurse visits. Participants explained that understanding of such terms had come from experiencing the Care Plus approach. At the outset of their involvement, patients had few expectations because they did not know what they could reasonably expect. Having experienced Care Plus services, they advised that they felt Care Plus provided increased contact time with practitioners, who could then monitor and support patients to be more active in their own care. Patient experiences of care delivery under the programme were positive. Most advised that the programme had provided them with more comprehensive monitoring and service than they were getting previously. Many felt that the structure had simplified their health care and provided them with a way to participate in the care process. A small number of patients transferred from HUHC to Care Plus. These people reported more gains from Care Plus compared with HUHC. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 41 Some had experienced input from other professionals (such as pharmacists and podiatrists) as part of the Care Plus process. This group did not report any access issues resulting from their referral. Participants were treating their Care Plans as an important record of events. They were referring to them to remind themselves of treatment, and some were sharing the information with family and specialists. Some had documented issues and/or questions in the plan for discussion with the practitioners at the next visit. Participants advised that their goals reflected the issues most important to them as an individual. They felt that practitioners had taken a patient-centred approach towards the setting of goals, and the majority felt that their resulting plan was a realistic guide to improved health and wellbeing. Most participants had experienced nursing visits as part of Care Plus, and everyone valued the nursing input they had received. Most portrayed feeling socially close to nurses, and expressed appreciation that the nurses seemed to have more time for them and interest in their general circumstances. Care Plus had increased patients’ affiliation with the practice and practitioners. In particular, nursepatient connections, resulting from the extra time spent with nurses, also seemed to enhance the GPpatient relationship. Patients said that having nurses to deal with some issues and bringing others to the attention of the GP meant that they were more confident about the use of GP time. Patients valued the improved access to care and monitoring that Care Plus affords, and they appreciated the extra involvement and interest from practitioners. Everyone felt that the increased contact, particularly with nurses, had improved their health knowledge. Many said that because of the higher levels of engagement, they were now undertaking self-care activities they had previously avoided. All patients recommended that the programme continue in its current form. Patients’ perceptions of Care Plus: brief telephone survey Three hundred Care Plus patients completed a 15-minute telephone interview. The full results of this survey are summarised in Appendix 6. The first question asked was whether the patient knew they were a Care Plus patient – 95 percent did (285/300). It must be realised that there are a large number of projects going on at any one time in general practice – risk assessment procedures, chronic care management programmes, various services to improve access, green Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 42 prescriptions and many others – and that therefore, in the opinion of the review team, this was a high figure. Respondents were then asked what Care Plus meant to them, in an open questionnaire. Responses were coded by a single researcher into the categories described in the following series of tables. The cell numbers represent themes illustrated in responses, and people could identify multiple themes. The responses are from 300 people and are the commonest replies. Table 18: What does Care Plus mean to you? (multiple responses allowed) Additional care 97 Economical practice visits 76 More regular input and support 69 Extra monitoring 61 Help to encourage self-care 47 Don’t know what it is 43 More reasonably priced prescriptions 36 Input from nurses 36 Other positive feeling towards Care Plus 15 Confidence and security 5 Other 2 Patients reported that Care Plus gave them more time with doctors and nurses, for better care. Most patients saw either a doctor or a nurse (about equal proportions), but very rarely both (11 percent). The average nurse’s visit was longer than a GP visit. The average fee for a Care Plus visit was reported to be $5. The review team was keen to understand the prevalence and use of Care Plans. Eighty percent of patients (240/300) had a written Care Plan. This nearly always involved goal-setting. The next table shows how patients reported they used their Care Plan. Table 19: How do you use the plan of care ? Guide to memory 87 No use 82 Means of documenting self-care 43 Record of care medications, treatment and events 26 Share information with others 19 Recording questions for the practitioners 13 Instructions to follow 11 Journal of important events Evaluation of the roll out of Care Plus CBG Health Research August 2006 5 p 43 Respondents were also asked what Care Plus gave them over and above their usual care. Responses fell into the categories in Table 20. Table 20: What does Care plus give you that you would otherwise not have ? Low-cost consultations 70 More contact with practitioners 48 Don’t know 42 Nothing 41 Systematic care 40 Regular care 39 Input from nurses 35 Support and assurance 31 More self-care 31 Goal-setting 24 Information 16 A third of respondents felt that Care Plus changed their relationship with their provider, most often with the nurse, and always positively. Table 21: Has being a Care Plus patient affected your relationship with: Nurses 59 GPs 24 Practice No change 4 217 Respondents were also asked what they valued most about Care Plus. Table 22: What do you most value about Care Plus? Security and support 64 Low cost 62 Input from nurses 47 Systematic care 46 More contact with practitioners 39 Regular care 36 More self-care 35 Don’t value anything 31 Goal setting 17 Nothing has changed 10 Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 44 Provider perspectives At this early stage there was little information available from providers about the impact of Care Plus on outcomes, due to the short period of time most patients had been on Care Plus. Some interviewees reported that Care Plus was leading to better treatment compliance by many highneeds individuals due to increased practitioner contact time. Some practitioners felt that while Care Plus could potentially have a significant impact on outcomes, there was a proportion of the high-needs audience that had yet to fully engage in using Care Plans or making lifestyle changes. Practice data Consultation rates Dates of encounters were downloaded for the 30 practices in the sample, for all registered patients, from 1 June 2003 to 28 February 2006. This download was cleaned so that only one encounter per day was counted, to avoid artefactual increases in encounter rates as a result of patients seeing multiple providers on a given day (eg, a doctor and a nurse for a single Care Plus visit). The number of encounters for Care Plus and non-Care Plus patients is shown in Table 23. Care Plus patients have high consultation rates – around 13 visits per annum before enrolling, rising to 17 visits per annum after enrolling (ie, a 30 percent increase in consultations). Non-Care Plus patients consulted an average of 3.26 times per annum across the entire data collection period (1 June 2003 – 28 February 2006). In this, and following similar tables, the experience of patients who have been enrolled in Care Plus is split into ‘before’ and ‘after’ periods, with the time of the split being different for each patient (depending on the date each patient was enrolled in Care Plus). The number of events experienced by these patients in each period (‘before’ and ‘after’) is divided by the number of years all Care Plus patients spent in the relevant period, to give rates for Care Plus patients in the ‘before’ and ‘after’ periods. For non-Care Plus patients a comparison rate is calculated, but the experience is not partitioned because there is no Care Plus enrolment date. This approach allows a comparison of Care Plus and non-Care Plus patients in both ‘before’ and ‘after’ periods. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 45 Table 23: Care Plus impact on consultation rates N Care Plus NonCare Plus Period 4569 177,100 Encounters Rate (visits / annum) % change 9482 2642 124,382 45,178 13.12 17.10 30.0 472,105 1,539,562 3.26 Years Before After All Quality of primary health care Quality indicators have been calculated using the prescription ratio procedure described in version 1.1 of the data definitions for the performance monitoring framework. This is the approach used to produce the ‘indicative’ indicator for diabetes prescribing quality: the ratio of the number of metformin prescriptions to the number of prescriptions for sulphonylureas. This procedure calculates ratios based on prescription volumes, and allocates volumes to a period based on the date the prescription was written. As an example, the following prescribing volumes were downloaded for patients with diabetes. Table 24: Sample prescribing data for patients with diabetes Group ACE ASP BAA MET DIU ICS INS NIT SUL Not Care Plus 3066 1956 655 2811 1124 472 1603 478 1735 Before Care Plus 7769 4484 1674 6820 2566 1292 3572 1168 4549 10,615 6276 2556 11,129 2953 1795 5836 1516 6719 After Care Plus Notes: ACE = ACE inhibitor; ASP = aspirin; BAA = beta adrenergic agonist; MET = metformin; DIU = frusemide only (ie, surrogate for CHF); ICS = inhaled corticosteroid; NIT = nitrate (eg, nitrolingual spray); SUL = sulphonylurea. For each group of patients with known chronic conditions, specific quality of care indicators were calculated, as shown in Table 25. Using these measures there was no consistent pattern of improvement in quality of care in Care Plus patients. The only improvement measured was in the ratio of metformin to sulphonylureas in patients with diabetes. The interpretation of this data may be confounded by the possibility that if Care Plus improves access (as has been discussed earlier), patients may be just starting a care pathway, and not in fact having their care ‘fine tuned’. Future research with larger, random data sets seems indicated, but one would certainly expect these indicators to show improvements over time. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 46 Table 25: Prescribing quality -of-care indicators Diagnosis Care Plus status Period Quality indicator Metformin : sulphonylurea Diabetes Not Care Plus Care Plus Before enrolment After enrolment Improvement ? Ischaemic heart disease ACE : hypoglycaemics 1.66 0.95 1.50 1.62 Yes 1.14 1.09 No Aspirin : nitrate Not Care Plus Care Plus 1.36 Before enrolment After enrolment Improvement ? Asthma 1.47 1.36 No Inhaled steroid : beta agonist Not Care Plus Care Plus 0.92 Before enrolment After enrolment Improvement ? 0.76 0.74 No Note: The ACE : hypoglycaemics ratio is calculated as (ACE) / (INS + MET + SUL) for each group (Care Plus or not Care Plus). Outpatients and emergency departments (EDs) Using the same method as described for encounter rates, the number of outpatient (OP) attendances and emergency department (ED) attendances were analysed for Care Plus and non-Care Plus patients. Data was supplied from each DHB from their propriety data management systems. Table 26: Imapct of Care Plus on ED atatendances Care Plus N Period Days OP events ED events 4569 Before 9,268,764 22,348 3073 0.88 0.1210 After 1,309,884 5734 690 1.598 0.1923 All 412,818,480 301,242 80,465 Non-Care Plus 177,100 OP rate 0.266 ED rate 0.071 Table 26 shows that Care Plus patients have a much higher utilisation rate of OP and ED services, both before and after enrolling in Care Plus. Outpatient utilisation after enrolling in Care Plus nearly doubled, and ED attendances increased by 50 percent. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 47 Hospital discharges The National Health Index numbers for patients at participating practices were used to download an extract of all discharges for these patients from the National Minimum Dataset. The download of discharges was coded to identify ambulatory-sensitive hospitalisations, using the first five ICD discharge codes. These discharges were classified as occurring before or after a patient’s first Care Plus assessment visit. To adjust for the variable amounts of time each patient had before and after Care Plus enrolment, the number of days each patient could have been admitted to hospital in each before and after period was calculated. This data can be combined to produce a summary of hospital admissions data, as shown in Table 27. This table shows that Care Plus patients are about six times more likely to be admitted to hospital (for an ambulatory-sensitive hospitalisation) than non-Care Plus patients. The impact of enrolling as a Care Plus patient appears to be to increase the admission rate by 40 percent. Table 27: Care Plus impact on hospital admission rates N ASH only Care Plus Non-Care Plus 4569 Before After Years 11,862 2322 ASH 2273 626 Rate 0.191623 0.269621 516,829 19,165 0.037082 % change 40.1 177,100 Note: ASH = ambulatory-sensitive hospitalisation. The natural progression of a chronic condition will cause some small increase in utilisation, but not 40 percent. This increase is likely to represent increased referral for secondary care, or changes in the utilisation of acute services (ED) as a result of patients changing their hospital contact behaviour. An example would be an asthmatic patient being advised to attend an ED once their peak flow fell to a certain level, which had been ignored (or unmeasured) previously. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 48 6 Conclusions and Implications The data presented in this report on patterns of Care Plus uptake has demonstrated the already well established socioeconomic determinants of health status. The most effective strategies to address these determinants will probably be political and organisational, addressing such issues as providing employment, education, reducing alienation, ensuring adequate housing and reducing poverty. However, there is still much that can be done at a primary health care level, especially in terms of ensuring that high-needs patients get access to high-quality care. The implementation of the Primary Health Care Strategy has recognised this by initially targeting resources to practices with high numbers of Māori and Pacific clients, and people who live in areas of high deprivation. As increased funding is extended to the entire population, other mechanisms for targeting may be required if health inequalities persist. The attraction of the Care Plus funding model is that it makes progress towards a number of strategic goals for primary health care. Not only does it enable additional targeting by need, recognising that a normal-length consultation is not enough for many high-needs patients, but it also begins to provide policy and funding support for the introduction of teamwork, and for expanding the role of nurses to more fully utilise their skills in chronic care management. In an environment where some patients face very high fees (eg, $65) for a consultation, it is not surprising that some practices will use Care Plus to subsidise a patient visit. In this case, the income to the practice might stay the same – the only thing that has changed is the fee barrier faced by the patient. For practices that charge low fees, or for patients already receiving significant subsidies, enrolling a patient in Care Plus is more likely to increase practice income. A large Access-funded group practice, charging low co-payments with a register of 10,000 patients, could expect to be able to enroll at least 500 patients in Care Plus (probably more, as being Access funded they will have more high-needs patients, recognised by the Care Plus funding formula). This represents $100,000 of extra income, less whatever co-payment reductions the practice implements. It is possible that this could fund a full-time nurse and pay for all his or her associated overheads, plus a car. In this practice, resources could be provided to significantly improve the quality of care being delivered to the patient. Thus the extent to which improved quality of care is delivered depends on the balance between these competing uses for the funding: how much of the extra resource provided by Care Plus is used to reduce co-payments, increase profit or provide increased resources. Because increased funding for primary health care is provided from other sources (eg, extending increased subsidies to adults aged 4564), we would expect to see increased opportunities for more fully implementing those aspects of Care Plus that relate to improved quality of clinical care. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 49 Increased funding is also available from Services to Improve Access funding and other sources. The policy environment is quite fluid. The capitation funding formula is being reviewed, and there are opportunities to consider the best ways to deliver Care Plus-type services in the future. This section reviews the major findings presented previously and suggests some implications for the future of Care Plus. The role of the Ministry of Health and DHBs It is clear from the interviews held with various stakeholders that there is a wide range of perceptions of what exactly Care Plus is. At a Ministry and DHB level there is a clear view that Care Plus is an attempt to improve chronic care management, reduce inequalities, improve primary health care teamwork, and reduce the cost of services for high-need primary health users. The manner in which Care Plus has been implemented in a given DHB is very much determined by the attitude of PHOs in that DHB to the opportunities Care Plus presents, and the willingness of practices to implement it. This variation presents an equity dilemma. It is undesirable for patients in one area to have access to different publicly funded services from patients living in another area. The solution to this may be to require practices to deliver Care Plus services if they receive capitation funding. Obviously this would have to be discussed with provider representatives. One way to implement this would be to include the Care Plus budget in the base capitation funding, and modify the schedule of services required from providers to include providing intensive clinical management services to qualifying patients. Recommendation 1: The Ministry could consider the structure of Care Plus funding with a view to ensuring all patients have equal access to services, as far as possible. There was a recurring theme throughout the interviews that Care Plus seems to work best when linked to existing chronic care programmes. Representatives from PHOs that had been able to do this felt these systems gave a sense of purpose and direction for Care Plus. Also, the completion of electronic CCM templates facilitates the collection of essential process and outcome information. It is fully integrated in the DHB chronic care management programme and it’s working well because of that. Our DHB has accepted and encouraged that all patients on the chronic care management programme should also be part of Care Plus. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 50 Recommendation 2: DHBs that have chronic care management programmes could consider how these can be linked to Care Plus. DHBs felt that the data they received was usually not adequate for any assessment of the impact of Care Plus. As the performance monitoring framework is progressively implemented it should be possible to analyse data by Care Plus status. Recommendation 3: Opportunities for monitoring the impact of Care Plus could be explored through the reporting associated with the performance monitoring framework. The role of PHOs and practices Most large PHOs also view Care Plus as an opportunity to improve chronic care management. However, the emphasis on the different components of Care Plus changes as one approaches the primary health care coal face. Many practices see Care Plus simply as a way of delivering an increased subsidy to patients with chronic conditions and no more. If a patient is in a group that receives a low level of subsidy, such as a 50-year-old adult in an Interim-funded practice, then Care Plus presents an obvious way of reducing financial barriers to care for that patient. The more abstract goals of Care Plus, involving enhanced care planning and increased teamwork, while they may be strongly supported are not necessarily easy to implement and it is not surprising that practices have implemented these to varying degrees. According to DHBs, PHOs that are already providing services to socioeconomically deprived populations often do not have the resources (time, space, staff) to deliver Care Plus. Smaller PHOs may struggle with the management overhead required to deliver Care Plus. The development of separate systems in each PHO for what is essentially the same task is highly inefficient. Some sharing of systems and infrastructure could therefore result in significant savings. Recommendation 4: Mechanisms for encouraging the use of pooled resources could be explored by DHBs and PHOs; for example, providing incentives for PHOs maintaining a shared Care Plus workforce and operating via referrals or practice visiting. This could reduce costs by reducing duplicated resources among PHOs (eg, Care Plan development and maintenance, workforce training, and referral systems). A wide range of funding mechanisms whereby PHOs reimburse practices for Care Plus services have been identified. Practices reported varying levels of support from their PHOs, ranging from simply handing on Care Plus payments, to sophisticated systems to assist with identifying patients, developing and providing Care Plan templates, and training staff. Ultimately, however, Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 51 practices themselves decide whether or not to participate in Care Plus, and the funding model offered by the PHO must be economically sensible for each individual practice. National funding Although some providers have felt that the level of overall funding for Care Plus should be increased, this review has not found any strong evidence to suggest the Care Plus funding model itself should be significantly altered. Some PHOs reported difficulties managing cash flow, which might be helped by larger payments, but the general concept of up-front establishment payments was supported, and subsequent staged payments over the year seems sensible (and consistent with all other funding). Earlier estimates of Care Plus numbers have been confirmed, and the general structure of the Care Plus funding matrix has also been validated. Two-thirds of practices thought that funding was not adequate. A small number of practices did not adopt Care Plus at all because the funding was not considered sufficient; other practices enrolled patients in Care Plus but did not deliver extra services. It would be reasonable for the Ministry to expect extra services to be delivered for extra funding. Practices considered that an increase to $290 (average) per patient per annum would be adequate. Recommendation 5: The Ministry could consider increasing Care Plus funding, while tying this to demonstrated delivery of additional services (volumes and/or quality). It seems clear that Care Plus does not overlap very well with some High User Health Card (HUHC) patients, as shown by feedback from providers in interviews, from the survey, and from the analysis of Care Plus enrolments. Practitioners described Care Plus patients as being a different group to those who access the HUHC. More specifically, they saw Care Plus patients as being those people who previously accessed care less frequently than desired, whereas patients accessing HUHC are those who already attended often enough to qualify for the HUHC and its associated benefits. This suggests that it may be desirable to maintain a separate funding stream for these patients, although it may be possible to incorporate them into the general capitation funding calculation, particularly as the increased subsidies associated with the roll-out of the Primary Health Care Strategy become available for more age groups. Maintaining the currency of an HUHC is a major, usually clerical, task for some practices, and can lead to perverse consulting behaviour, such as multiple brief visits for perfunctory monitoring in order to maintain eligibility. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 52 Recommendation 6: A separate funding stream is probably required for HUHC patients, who appear to be a different group of patients to those targeted by Care Plus. National utilisation distribution data could be used to fine-tune the capitation funding formula, and to check these assumptions. The major question with funding streams in primary health care (apart from their size) is whether they can be amalgamated. The management of a large number of small contracts for different types of health care can impose significant administrative overheads. These are reduced at the practice level if the management functions are taken over by the PHO (which may sub-contract them to a management organisation), but any extra administration ultimately removes resources from service delivery. It may also be more efficient to add Care Plus payments to capitation funding payments (to practices from PHOs), and to pay it at some proportion of the estimated total uptake, with regular review of the evidence for improved care from practice data sources, possibly monitored through an enhanced performance management framework. Delivering Care Plus in the practice Most participants reported that Care Plus represents a significant change in primary health care service delivery. As such, they anticipated that it would require significant time to embed itself within primary health care. They strongly recommended that the Ministry not regard delays in the programme’s uptake as a failure of the philosophy. The slow uptake of Care Plus as a national programme, the relative complexity of care delivery (with written Care Plans and changes in practice processes), and the difficulties some PHOs have experienced managing cash flow mean that Care Plus has taken longer than expected to become incorporated into the day-to-day delivery of primary health care. Limited funding, space, time and nursing staff may also be reducing the potential uptake and impact of Care Plus. Those who had offered a free service from within a high-needs Access practice deemed the approach a success, particularly if the Care Plus visits were aligned to patients’ medication requirements. These representatives felt that their patients were attracted to the prospect of free visits, and, as a result, complied with requests to consult. This, in itself, was felt to be a considerable first step for many of their population. They are turning up because it is free. If they do not, the nurse rings them. This population, them turning up, is huge. It’s a real start. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 53 Those services that had a clinical co-ordinator to help establish Care Plus reported that this had underpinned their success. Staff valued the support and training these professionals had been able to offer. They described feeling confident in what they were looking to achieve through the programme because of the efforts of the co-ordinator. Some of the practices have used the PHO nurse support to help them with Care Plus. Finally, interviewees advised that those who had made good use of the PMS for patient selection, data collection, care planning and recall had been successful. Staff who had received on-site IT training and support said this had underpinned the establishment of good systems and efficient service delivery. It was really useful them coming to us because they could train us on our system and they are just there to support if you need them. Informants made a large number of suggestions for the most effective means of organising and delivering Care Plus services, other than those already mentioned. Suggestions offered by interviewees for delivering Care Plus Use electronic templates, if possible. Link Care Plus to other programmes (eg, green prescriptions) and PHO services (eg, diabetes nurses, podiatry). Use Care Plans as the basis for provider communication. Have flexibility about the timing of Care Plus visits, and tailor the visits to suit the needs of the patient, in particular repeat prescriptions. Promote Care Plus as a fundamental care system, where Care Plans and patient-centred goals are the focal point, as opposed to treating it as another Access funding stream. Employ a clinical co-ordinator to work onsite in order to establish Care Plus in practices, and provide ongoing education and support. Obtain explicit practice agreement to use Care Plans, and encourage practitioners to work with patients to facilitate their use of them. Provide some form of incentive to encourage teamwork. This may include extra service payments, integrating Care Plus into programmes, and/or making other PHO resources (such as mobile/outreach nursing) available to support Care Plus. Create funding parity between Care Plus and HUHC patients to encourage the replacement of HUHC (but note the alternative view that these are separate groups). Table 28 summarises the suggestions made by participants for improving the delivery of Care Plus at the DHB and/or PHO level. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 54 Table 28: Summary of practitioners ’ suggestions for improving Care Plus Calculate the next quarter based on the previous one, with an estimated margin for growth. Revise funding mid-quarter. Increase the resource allocation and payment flexibility for practices to provide more than the current number of visits, where required by the patient. Link funding to performance monitoring of Care Plus activity (as opposed to funding visits without taking account of the care employed). Replace the changing quarterly denominator with a 612-month target. Provide reporting by ethnicity Detail decile codes across the entire population. Profile patients by all conditions and important demographics. Illustrate the reach of Care Plus within populations. Levels of engagement/actual activity (Care Plans) /process/outcomes. Explain deficits between HealthPac findings and PHO claims. Provide more online materials/information (in different languages) / PMS templates. primary health care performance indicators Align/integrate whānau ora contracts with: the pharmacy framework. Encourage: Care Plus as a basic care approach for CCM and other programmes PHOs piloting methods to improve systems and teamwork the use of clinical co-ordinators ongoing training and support, particularly for nurses in CCM effective use of Care Plans/teamwork. nurse involvement accountability for implementation of the care approach national communications about the programme education about teamwork involvement of secondary care, national and local workforce committees, and other professionals bodies focus on implementing a change in general practice rather than providing a low-cost entitlement for chronic care patients to access GPs. Revise the funding scheme Improvements to: Monitoring Administration / IT support There is a need for increased: Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 55 It has been noted throughout this review that Care Plus seems to work best, in terms of improved care, when linked to a CCM programme. One suggestion is that this is because of the increased structuring of care that formal CCM programmes require. This review has shown considerable variation in the degree to which Care Plans have been implemented. While 80 percent of patients reported having a Care Plan, over a third reported that it was of ‘no use’. Recommendation 7: If Care Plus were to continue it would be worth considering whether some specific elements should be required in order to qualify for funding. Enrolment in a CCM programme could be one requirement, or at least the construction of a detailed Care Plan, possibly with specified components. Formal completion of a Care Plan could be relatively easy to implement, because the completed templates could be submitted electronically, as national data collections (eg, Get Checked II) were built. It could be helpful to tie these templates to best practice guidelines, maintaining a set of required activities/measurement for any template for a given chronic illness. It would also be important to have a generic template. There will always be high-needs patients (eg, mental health patients or those with disabilities) who will not fit into rigid templates, and such an approach would not be desirable for many conditions. In addition, some chronic conditions would be too rare to warrant a detailed template. However, even a generic template could provide useful structure for CCM (eg, exploring access to social welfare benefits, screening for depression, medication review). Who gets Care Plus? Although uptake has been slower than expected, Care Plus appears to be reaching the major intended recipient groups those with chronic illness. Practitioners reported that Care Plus is being targeted to patients with chronic high needs. National data from the Ministry of Health shows that Māori and Pacific patients appear more frequently in Care Plus enrolments than their population rates, as would be expected from known greater need. The pattern of uptake by age also reflects known distributions of chronic illnesses. The commonest qualifying criteria for Care Plus was ‘two-plus chronic conditions’. However, two of the top four conditions recorded by practices as Care Plus qualifying conditions were hypertension and hyperlipidaemia. These conditions do not usually require ‘intensive clinical management (2 hrs per 6 months)” as required by the Care Plus criteria. They may, however, require regular monitoring at times, and illustrate the possible difference between Care Plus and Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 56 HUHC patients. In any event, further clarification of expected Care Plus qualifying conditions would probably be useful. Recommendation 8: Guidance on the status of conditions that require routine monitoring as Care Plus qualifying conditions would be helpful. This raises the more general question of whether the Care Plus criteria as they currently stand are in fact too restrictive. It would seem highly desirable that patients who have diabetes or asthma should in fact qualify for Care Plus if they need significant clinical input. They may not require high levels of input at all times, or even four times a year, but there will be times for most of these patients when extended consultation times (‘double consultations’) are indicated. The Care Plus criteria should not require doctors and nurses to stretch the definitions for these patients to be eligible for funding. A related issue is the delivery of services to patients with disabilities or those with mental illness. A more flexible definition would allow these patients to qualify unequivocally for Care Plus funding. Recommendation 9: The Care Plus criteria could be revisited to make sure that services can reach patients that need them within the contractual criteria. The combination of ‘two or more chronic conditions’ and the requirement that each require ‘intensive clinical management’ may be too restrictive. The key role of nurses Many practices are embracing a more team-oriented approach to delivering chronic care, which has the potential to lead to improved outcomes, and continued funding through Care Plus will support this paradigm shift. Half of practices in the survey of practices reported that Care Plus was a nurse-led or exclusively nursing service. Free text responses suggested that this represents significant progress towards increased utilisation of nursing skills in chronic care management. Practice income is not dependent on who delivers a Care Plus service. In order to increase this proportion it may be necessary to get a fuller understanding of the barriers to expanding nursing practice further in the current primary health care environment. Recommendation 10: It would be useful to conduct qualitative research to explore incentives and barriers to independent nursing practice within the primary health care team. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 57 Most participants from services that had involved nurses in key roles in Care Plus delivery agreed that this had worked well. They thought that where nurses had become fully involved and actively supported the approach, the programme has run smoothly and proved successful. It’s really the nurse; she is driving it – having good nursing staff that is the key. The majority of GP participants valued nurse involvement in chronic disease areas, and nurses themselves reported increased job satisfaction. However, interviewees suggested that the programme must make more provision for nurse training in chronic disease areas and this was confirmed by comments from nurses Without up-skilling, I could not have done this. I have done diabetes course, asthma and COPD, and some post-grad papers in chronic disease. The training needs to be practically based. At present nurse specialisation requires a significant sacrifice of time and income for nurses undertaking further education. As recommended in an earlier review of Reducing Inequalities Contingency Funding it would be worth facilitating co-ordination across a number of organisations – Nursing Council, Clinical Training Agency, Health Workforce Advisory Committee, among others – to develop a series of free, short (say three-month) courses whereby nurses could gain further training and qualifications, including prescribing rights, in the management of specific conditions. It is notable here that one of the recommendations from providers was that Care Plus visits be aligned with medication repeat visits. Unless a nurse is merely handing a standing order to a GP to sign, this should be an opportunity to titrate medication while reviewing overall management, and this requires prescribing rights. Recommendation 11: Primary health care nurses need access to short, affordable training courses to allow them to deliver chronic care services most effectively, including prescribing, to maximise the role they could play in the delivery of Care Plus. For many patients with chronic conditions, physical access to services is difficult. This suggests the need to develop the nurse home visitor undertaking chronic care management in the home, which is the best place to undertake comprehensive needs assessments. A large proportion of chronic care is concerned with developing strategies to live with a condition, and an assessment of the living situation including social supports, family dynamics and physical environment is often essential. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 58 Recommendation 12: Many Care Plus services could be efficiently delivered as part of a home-visiting programme. Any Ministry of Health development work on home visiting should consider how such a service would work with Care Plus. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 59 Appendices Appendix 1: Summary of findings from pilot evaluation. Practices elected to be part of the Care Plus pilot because the initiative appeared to target patients with chronic conditions, had the potential to improve patients’ access to general practice and encourage more regular consultation. Most practices favoured the selection of patients under the chronic conditions criterion. The transfer of High User Health Card (HUHC) patients to Care Plus was seen as problematic by most of the pilot practices, both from a patient and practice finance perspective. Patient responses to an invitation to take part in Care Plus were favourable, with a limited number of refusals. The level of involvement expected from patients by practitioners varied from an expectation that patients take an active part in their health care and make appointments for review visits, to lower expectations of involvement where the practice actively recalls the patient. In the experience of most of the practices, the Care Plans are largely unread by patients. Many practitioners tried to encourage patients to write in the booklets but advised that this had been relatively unsuccessful. It was advocated that the programme focus on the use of brief interventions and simple one-page documentation. Opportunistic recruitment of patients returning to the practice for a prescription appeared to be a successful recruitment process. Active recruitment also yielded good results, but practices had been unable to sustain it because of the nursing time involved. A good recall system was considered to be imperative to the success of the programme. In the experience of the pilot practices, the time involved for patients and practitioners, patient apathy towards a more active role in their own care and staffing were the main barriers to implementing the programme. Patients who have limited interest, education, time and understanding about the management of their condition have difficulty engaging with Care Plus. Two patient groups were identified as more likely to have problems with the approach: older males and the very elderly. Most practices thought there should be a nurse co-ordinator at the PHO and/or national level. It was thought that Care Plus fully utilises nursing skills and increases their profile with patients. Nurses appeared to be taking a lead in care planning in most practices, but the input of GPs and nurses in Care Plus visits, particularly reviews, was varied and constrained by funding, time and a practice’s support of autonomous nursing practice. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 60 Getting the right staff involved in the Care Plus programme at the practice level was most strongly predictive of successful implementation. Establishing the number of nursing and GP hours required in relation to patient numbers and implementing a plan to stagger the introduction of the programme were seen as key to success. The majority of pilot practices thought that Care Plus was not an easy scheme to run in the busy and time-restricted environment of general practice. Practices advised that the length of time required for Care Plus consultations does not always fit with the time available during everyday general practice. The provision of nursing consultations had required, in some practices, extra nursing cover and limiting appointments to specific times and/or days. Discussions highlighted that limiting Care Plus visits to specific times can present access issues for some patients, and difficulties integrating nursing and GP input into the programme. Practices had not reached the capped rate because, for the most part, they had insufficient time to implement the programme for all of the eligible patients. Some practices were experiencing problems with patient drop-out rates (between 5 and 50 percent, typically 50 percent) at the review stages. The reasons included: no active recall for review appointments negative perceptions of nursing consultations where nurses were completing the review Care Plus being offered at limited times because of the need for extra nursing cover. Some practitioners warned of hidden costs, in terms of the extra nursing and GP time required to complete Care Plans for more complex cases. Providing training for nursing staff, so that they could be more involved in chronic care management, was also seen as a hidden cost for both practices and PHOs. The funding of patient care reviews was not viewed as sufficient to support both nurse and GP input. The key issues perceived by practitioners as being likely to face Care Plus if it is extended to all practices to replace HUHC were thought to be the loss of prescription subsidies for A3 patients, ensuring practice revenue exceeds that already derived from HUHC funding (given more work is required), and improving the funding of review visits to allow the incorporation of both nursing and GP inputs. Some practitioners warned that the programme could experience a lack of support in practices that have not previously promoted either nurses’ independent practice and/or a care planning approach. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 61 Increased use of electronic systems to support the programme was recommended, to remove disincentives associated with increased paperwork. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 62 Appendix 2: Review methods The review used both qualitative and quantitative research approaches to review the implementation of Care Plus. The research design consisted of: PHO case studies DHB interviews Ministry of Health interviews key informant and ‘affinity pair’ interviews with practices in participating PHOs PMS data collection and clinical management analysis (prescribing/utilisation) PMS data extract correlation with hospital discharge data in the National Minimum Dataset secondary care utilisation review from hospital records (ED / OP) patient focus groups a computer-assisted telephone survey (CATI) of 300 patients a survey of 300 providers. The key idea is that each PHO, and to a lesser extent practices within PHOs, implement Care Plus differently. While there will be a comprehensive collection of quantitative data, this data must be examined with the knowledge of how Care Plus was implemented in a particular instance. By adopting a case study approach, quantitative data can be better interpreted. Having chosen the review PHOs, we examined how they have worked with their DHBs, how practices within each PHO have implemented Care Plus, and patients’ experiences of the programme. This detailed examination of specific Care Plus implementations was backed up by a comprehensive look at the impact of Care Plus as measured by data from PMS, DHB and national data sets. The next sections describe the qualitative research tools we utilised, and the methods we used to collect quantitative data. Qualitative research The qualitative work included 12 case studies of PHOs (the case study approach combines quantitative and qualitative work); 12 key informant interviews with practices associated with the selected PHOs; and eight focus groups with patients (four groups, 24 patients), DHBs (three groups, 18 DHB representatives) and the Ministry (one group, six Ministry representatives). We offered a series of four key informant or ‘affinity pair’ interviews (where two individuals are interviewed together) to replace one focus group, where a group discussion was not practical for the participants. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 63 An inductive study approach that utilises a causal coding frame, based on a grounded theory model of analysis, guided the research. Interview guides were created in consultation with the Ministry, and included the key themes identified in the research tender. Sample selection and recruitment Representatives from the DHBs were selected, in consultation with the Ministry, to take part in focus group discussions. We sought support for the research from the selected DHBs and related PHOs. DHBs and PHO participants were contacted by telephone, and an information pack containing a summary of the research approach, aims and use of the information was forwarded to them. An accompanying letter invited them to identify people who should take part in the group discussions or interviews. Twelve PHOs were selected, in consultation with the Ministry and DHBs, to take part in the qualitative case studies. We attempted to represent different PHO compositions, according to funding types, ethnic mix, location, economic and social indicators, and levels of high-need patients. Key informant or affinity pair interviews were completed with the person/s responsible for implementing Care Plus in the practices. Twelve practices belonging to the case study PHOs were selected, in consultation with the Ministry and PHOs, to take part in the key informant interviews to inform the case studies. We sought to represent different practice compositions, according to funding types, ethnic mix, location, economic and social indicators and numbers of high-need patients. These practices were asked to provide a list of Care Plus patients who could take part in the focus group discussions. Twenty-four patients, matched to the ‘case study practices’, were selected to take part in four group discussions, representing different ages, needs, ethnicity, gender mix and Care Plus selection criteria. Basic patient contact details were required by the research team. Māori and Pacific facilitators helped to complete the groups where the patient composition required a facilitator of matched ethnicity. Potential participants were contacted by telephone by a qualified nurse not involved in the patient’s care and invited to take part in a group. A research nurse made a minimum of three calls to selected individuals. Patient participants were recruited under a protocol that included two clear opportunities for them to end the call prior to a final offer to take part, and the recruiter gave assurances that there would be no negative consequences from participating or declining. The initial call was made in English by a research nurse who had experience of recruiting consumer participants. Participants were told the purpose of the study, what was going to be asked, how the information would be used and how their privacy would be protected. The contribution of participants was acknowledged with a koha. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 64 The Ministry was asked to provide a list of key people who had been or were responsible for the implementation of Care Plus. Six key informants were selected, in consultation with the Ministry, to take part in a focus group discussion in November 2005. Ministry representatives were given findings, to date, from the PHO case studies. Comments were invited during the focus group discussion and representatives were asked to contribute to the design of the patient and practitioner quantitative surveys. All professional research participants were contacted by a research manager and invited to take part in an interview with the researcher at a time and date convenient to them. The research manager negotiated a timeframe for the interview that allowed participants 2030 minutes to read the guide and make some notes (where applicable). Participants were sent a letter of confirmation of the focus group date and time and the interview schedule to facilitate preparation for the discussion. Data capture Semi-structured interview guides were created to ensure that all relevant research aims were covered during each group or interview. The guides were sent to the participants 7 to 10 days prior to their interview. Interviewees were asked to complete some notes (spending no more that 2030 minutes) to facilitate their interview discussion. Our research manager negotiated with all interviewees to ensure they were able to read the guide and complete some notes in the timeframe allocated. The Ministry was asked to ‘sign off’ on the guides to ensure that they captured all of the information required. Groups and interviews were 6080 minutes in duration. Discussions were recorded with the permission of the participants, and where possible the researcher took notes during the discussion. Discussion themes Discussions with DHB, PHO and Ministry participants covered: the organisation and delivery of Care Plus how Care Plus is planned to reach, and is reaching, high-need patients support provided to organisations the provision of information to support the implementation of Care Plus defining the Care Plus identification process (including use of ED/OP data, etc) allocation of Care Plus patients to PHOs uptake of the programe by high-need individuals from deprived areas and/or Mäori and/or Pacific people. perceptions of Care Plus Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 65 the impact of Care Plus on the organisation requirements to set up the programme monitoring of Care Plus cost and resource use the effects of the programme relationships, links and networks necessary to support the programme workforce issues, innovations and training requirements fit of the programme in the wider health care environment recommendations for organising and delivering Care Plus services areas for improvement in the implementation of the programme. Discussions with practices addressed the following areas: how well Care Plus is reaching those individuals with high primary care need processes used to identify Care Plus patients at a practice level how high-needs patients are being reached practitioners’ selection of Care Plus patients with reference to any subjective judgement criteria methods employed by practice staff to select potential Care Plus patients, particularly the use of ‘head held’ patients lists the use, if any, of hospital and ED admission list and disease code guidance to identify Care Plus patients interpretation of each criterion for Care Plus eligibility, especially ‘two or more chronic conditions’ uptake of the programme by high-need individuals from deprived areas and/or Mäori and/or Pacific people PHO support, guidance and management use of any PHO’s tools for identifying Care Plus patients incentives, time and other resources involved in the identification/implementation process for practices fit of the Care Plus approach in the working general practice environment factors associated with the successful implementation of Care Plus time involved in Care Plans, recall, reviews, patient identification and management of the Care Plus portfolio professionals’ roles and scopes of practice in the Care Plus process the training requirements of each professional teamwork, necessary for Care Plus, within the practice, PHO and wider community understanding the clinical and quality-of-life impacts of the programme relationships, links, networks necessary to support the programme Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 66 workforce issues, innovations and training requirements recommendations for organising and delivering Care Plus services. Discussions with Care Plus patients covered: the patient’s experience of care delivery patient perception of Care Plus the value of Care Plus from a patient’s and their family’s perspectives impact of Care Plus cost incurred by the patient outcomes from the patient’s point of view areas that could be improved / should be further developed in the wider patient survey. Data analysis and validation The interview data was openly coded (ie, examined, compared and categorised). Each category of information was identified as a theme and developed using the following frame: 1. theme category description of the event /issue 2. intervening conditions factors that affect(ed) the event/issue 3. interaction/action outcome of the event/issue 4. consequences effective or not effective. The categories were linked and developed through comparing and asking questions to understand the types of relationships between the themes. Each interviewee was provided with a summary of the findings from the coding and analysis and asked to validate that it was a true and correct interpretation of the discussion. Only validated findings were used to create the case study report. Quantitative data Existing data sources From the 12 PHOS selected for the case studies we chose 30 practices representing high and low users of Care Plus services, as measured by their PHO. Twelve of these were included in the qualitative research with practices, as described above. These 30 practices were offered a financial incentive ($250) in return for allowing us to download data using automatic queries from their PMS system, and for assistance in identifying 10 Care Plus patients each for a CATI survey. Patients were offered a small incentive for participation. We used existing data from five data sources: Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 67 practice management system (PMS) data hospital databases (ED and OP) National Minimum Dataset HealthPAC data sets – the PHO uploads. Linkages between these databases were utilised to describe the patients receiving Care Plus services and the associated outcomes. PMS data was used to describe utilisation patterns of Care Plus patients before and after the introduction of Care Plus. PMS data was also used to see if patients eligible for Care Plus were actually getting access to the service. The National Health Index number of Care Plus patients was used to describe changes in the use of ED and OP services by matching these with hospital databases. The National Health Index number of Care Plus patients was also used to track the use of secondary care services nationally by extracting data for these patients from the National Minimum Dataset. Surveys After completing the qualitative research with patients and providers, we designed, in consultation with the Ministry, two questionnaires: one that was administered to a random sample of 244 Care Plus patients and the other to a random sample of 300 Care Plus providers. These sample sizes were chosen to allow rate estimates of around 50 percent to be estimated +/- 6 percent, and estimates around the 10 percent level to be estimated +/- 3 percent (95 percent confidence interval, power = 80 percent). We based these power calculations on an estimate of the precision required for policy assessment; ie, we regarded smaller margins of error (and therefore larger sample sizes) as being an inefficient use of resources. The content of these surveys was determined by the themes identified in the qualitative research. In general terms, the patient survey explored satisfaction with aspects of the Care Plus process, any improvement in the patient’s health status, and financial impacts. The provider survey asked about remuneration, workforce issues and the process of delivering care. The provider survey also asked about potential areas for improvements in the Care Plus programme. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 68 Appendix 3: Care Plus conditions Disease type N % Disease type Hypertension 1861 18.4 Other mental health 16 0.2 Diabetes 1846 18.3 Chronic disease monitoring 15 0.1 IHD 853 8.5 Pulmonary embolism 15 0.1 Elevated lipids 754 7.5 Acute bronchitis 15 0.1 Asthma 581 5.8 MS 15 0.1 Arthritis 373 3.7 Chronic sinusitis 14 0.1 Other heart disease 322 3.2 Menorrhagia 14 0.1 Congestive heart failure 314 3.1 Hyperthyroidism 13 0.1 COPD 273 2.7 Endometriosis 13 0.1 Obesity 263 2.6 Prostatism 13 0.1 Gout 245 2.4 Peripheral neuropathy 13 0.1 Stroke / TIA 188 1.9 Other peripheral vascular disease 13 0.1 Depression 186 1.8 Heart disease screen risk 13 0.1 Thyroid 157 1.6 Warfarin monitoring 12 0.1 Other GI 144 1.4 Deafness 12 0.1 Cancer 135 1.3 Spinal stenosis 12 0.1 Gastro-oesophageal reflux 123 1.2 Chronic lymphoid leukaemia 12 0.1 Kidney disease 99 1.0 Aortic aneurysm 12 0.1 Osteoporosis 95 0.9 Carpal tunnel syndrome 11 0.1 IGT 61 0.6 Vitamin B12 deficiency 10 0.1 Epilepsy 60 0.6 Non-alcoholic fatty liver 10 0.1 Smoker 55 0.5 Dementia 10 0.1 Other respiratory 52 0.5 Recurrent urinary tract infection 10 0.1 Diabetes complications 49 0.5 Hyperparathyroidism 9 0.1 Connective tissue disorder 47 0.5 FH IHD 8 0.1 Anxiety 45 0.4 Haemochromatosis 8 0.1 Eczema 44 0.4 FH DM 8 0.1 Migraine 42 0.4 Paget's disease of bone 7 0.1 Sleep apnoea 37 0.4 Hearing loss 7 0.1 Allergic rhinitis 37 0.4 Chronic bronchitis 7 0.1 Back pain 35 0.3 Piles haemorrhoids 7 0.1 Glaucoma 34 0.3 Cholecystectomy 7 0.1 Parkinsons 23 0.2 Otitis media 7 0.1 DVT 23 0.2 Cervical intraepithelial neoplasm 7 0.1 Peripheral vascular disease 22 0.2 Obsessivecompulsive disorder 6 0.1 Evaluation of the roll out of Care Plus CBG Health Research August 2006 N % p 69 Psoriasis 20 0.2 Raynaud's syndrome 6 0.1 Bipolar 18 0.2 Intermittent claudication 6 0.1 Cataract 18 0.2 Acute rheumatic fever 6 0.1 Hepatitis 18 0.2 Meniere's disease 6 0.1 Hepatitis carrier 17 0.2 Chronic fatigue syndrome 6 0.1 Gastritis 17 0.2 Iron deficiency anaemias 6 0.1 Schizophrenia 16 0.2 Pernicious anaemia 6 0.1 Polycystic ovaries 16 0.2 Cardiac syndrome X 6 0.1 Benign prostatic hypertrophy 16 0.2 Varicose veins of legs 6 0.1 Alcoholism 16 0.2 Cholelithiasis 6 0.1 10091 100% Total Notes: IHD = ; COPD = ; TIA = ; GI = ; IGT = ; DVT = ; MS = ; FH IHD = ; FH DM = ; Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 70 Appendix 4: CP funding formula 1. Calculating the expected number of Care Plus patients Each quarter HealthPAC will calculate the expected number of Care Plus Patients as follows. a. The percentages in each cell of the table are applied to the numbers in the corresponding cell of the PHO register. Table A1: Expected Care Plus population distribution Māori or Pacific peoples Not Māori or Pacific peoples Age group Gender Deprivation Deprivation Deprivation Deprivation quintile < 5 quintile 5 quintile < 5 quintile 5 04 Female Male 514 Female Male 1524 Female Male 2544 Female Male 4564 Female Male 65+ Female Male 2.0% 2.6% 1.5% 2.2% 2.0% 3.1% 1.7% 1.9% 0.6% 0.8% 1.1% 1.2% 0.5% 1.6% 0.7% 0.7% 3.3% 3.4% 1.4% 2.5% 0.8% 1.4% 0.5% 1.5% 3.8% 4.3% 2.4% 2.6% 3.1% 3.6% 1.3% 1.6% 13.8% 13.9% 4.8% 8.5% 15.9% 16.7% 6.0% 9.3% 29.2% 33.8% 18.4% 22.4% 37.2% 41.0% 21.2% 24.7% b. The resulting numbers in each cell are totalled. c. The existing number of individuals with High Use Health Cards is deducted from this total to give the expected Care Plus population. 2. Calculating funding The full funding the PHO will receive to deliver Care Plus services to the expected Care Plus population is calculated by multiplying the Care Plus residual population by the rates for Care Plus: $199.51 (plus GST) for Access practices and $211.75 (plus GST) for Interim practices. 3. Roll-out of funding Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 71 It is recognised that it takes time to enrol Care Plus patients and that there are higher costs in the initial periods. For this reason, Care Plus funding will increase as more Care Plus patients are enrolled. Initially all PHOs will receive 50 percent of their full funding, even though they have not enrolled any Care Plus patients. Once a PHO has enrolled 50 percent of the expected total, Care Plus patients enrolled in Care Plus then receive 65 percent of full funding. When Care Plus enrolment reaches 65 percent, funding increases to 80 percent. Once 80 percent of the expected numbers have been enrolled, then, provided at least 70 percent of the expected numbers in deprivation quintile 5 and in Mäori and Pacific groups in high-need sub-groups are enrolled, the PHO will get the full Care Plus funding. 4. Current funding is (from July 2005): 2005/06 rate (increased from Funding formula initial funding level) Access $205.05 Interim $217.64 Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 72 Appendix 5: Qualitative research report See separate stand-alone report, available on request. Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 73 Appendix 6: Patient survey: summary of responses From each of the 12 PHOs in the review, two to three practices were chosen to build a sample of 30 practices for further research. Each of these practices invited the next 10 Care Plus patients they saw, after a nominated start date, to take part in a phone interview with a researcher, for which they received a small koha (a $20 petrol voucher). The response rate was 82 percent (300/367). 1a Did you know you were a Care Plus patient? N = 300 Yes 285 No 15 One person mentioned that because people did not expect to be interviewed about the programme, and that the name ‘Care Plus’ is not necessarily marketed , it may cause the programme to be under-recognised and undervalued. Many confused the name with the Home Help Care schemes. 1b What does Care Plus mean to you? Additional care 97 More regular input and support 69 Economical practice visits 76 More reasonably priced prescriptions 36 Extra monitoring 61 Help to encourage self-care 47 Input from nurses 36 Don’t know what it is 43 Positive feeling towards Care Plus 15 Confidence and security 5 Other 2 2. Who do you usually see for your Care Plus visits? Nurse only 149 GP only 138 Nurse and GP Evaluation of the roll out of Care Plus CBG Health Research August 2006 38 p 74 3. How much time do you spend with each professional at your Care Plus visits? Nurse GP Less than 20 minutes 87 115 2040 minutes 71 47 40–60 minutes 25 4 60 minutes plus 10 - 4. Who recruited you to take part in the programme? Nurse only GP only 94 167 Receptionist/practice 13 Couldn’t remember 26 5. Why did you decide to take part? Low-cost visits 60 More time with practitioners 23 Increased monitoring 48 Struggling to cope with their situation 67 Good idea to support the programme 59 Practice initiated 72 Other Didn’t decide to take part 2 16 6a. How much are you charged for a Care Plus visit? Average $5 a mixture of GP and nurse consultations. 6b. What do you normally pay for a consultation? Usually a doctor consultation. $05 3 $610 11 $1115 80 $1620 38 $2125 18 Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 75 $2630 48 $3135 26 $3640 8 $40 plus 44 Unsure 25 7a. What have you come to expect from your involvement in Care Plus? More contact with practitioners Regular care 47 109 Systematic care 91 Goal-setting 25 More self-care 45 Input from nurses 38 Support and assurance 7 Lower cost 25 Information 10 7b. What does the nurse do as part of this programme? Initial observations (eg, blood pressure) Dressings/wound care Vaccinations 217 7 13 Referrals 8 Write Care Plan with client 16 Blood tests 2 Other 2 8a. During your Care Plus visits, did a nurse or a GP set goals with you? Yes 222 No 73 (Yes = goals set by either GP or nurse) 8b. Do you have a copy of those goals? Yes 178 Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 76 No 35 8c. Do the goals reflect things that are most important to you? Yes 201 No 4 8d. What do the goals mean to you? Increasing wellbeing 174 Increasing independence/self-care 108 9a. Have you received a plan of care? Yes 240 No 55 9b. If yes, how do you use the plan of care? No use 82 Record of medications, care and events 26 Guide to memory 87 Share information with others 19 Means of documenting self-care 43 Recording questions for the practitioners 13 Journal of important events Instructions to follow 5 11 Other health care services were impressed with the Care Plus Care Plan when the patient presented it.. 10a. Were you transferred from High User Health Card to Care Plus? Yes 98 No 192 Many confused prescription discount schemes at the local chemist with CarePlus. 10b. Which programme do you prefer? Care Plus High User Health Card Evaluation of the roll out of Care Plus CBG Health Research August 2006 34 3 p 77 Don’t know /N.a. 57 10c. What are the reasons? More contact with practitioners 7 Regular care 6 Systematic care 10 Goal-setting 4 More self-care 6 More input from nurses 8 N.a. /don’t know 3 Lower cost 7 Information 8 Those who had to go at the HUHC rate because of their condition felt penalised. They got fewer subsidised visits. 11a. Have you seen other professionals, other than the GP and nurse, as part of Care Plus? Yes 116 No 172 11b ….if so, who? Someone from the practice 2 Someone from the PHO 4 Specialists-medical/surgical 98 Dietitian, ophthalmologist or podiatrist 12 11c. Did you experience any difficulties accessing that person or service? Yes 6 No 110 A few had long waiting times 11d. What does Care Plus give you that you would otherwise not have? More contact with practitioners 48 Regular care 39 Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 78 Systematic care 40 Goal-setting 24 More self-care 31 Input from nurses 35 Don’t know 42 Nothing 41 Low cost 70 Support and assurance 31 Information 16 12a. Has being a Care Plus patient affected your relationship with: Nurses 59 GPs 24 Practice 4 No change 217 Most people said that their relationship was already good. All change was positive. 13. What do you most value about Care Plus? More contact with practitioners 39 Regular care 36 Systematic care 46 Goal-setting 17 More self-care 35 Input from nurses 47 Don’t value anything 31 Nothing has changed 10 Low cost 62 Security and support 64 Information 17 14a. Would you change anything about the programme? Yes 21 No 248 Unsure 25 14b. If yes what? Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 79 More visits 2 More time with Dr 2 Group sessions 3 More information 4 Fewer visits unless required 4 Should be expanded to other services 8 See the same nurse each time 1 Evaluation of the roll out of Care Plus CBG Health Research August 2006 p 80