3.5 Model of Simple/Complex Discharge

Discharge and Home of Choice
Policy
CPCT/001/017
Document Number:
Date ratified:
Date issued:
Review date:
POLICY STATEMENT:
This policy is for use by the multi-disciplinary, multiagency team and sets out the requirements to ensure the safe and efficient discharge of patients from hospital.
Discharge and Transfer of Home of Choice Policy September 2010
1 of 114
Title
POLICY DOCUMENT CONTROL SHEET
Title Cumbria Discharge and Transfer
Policy
Version 2
Supersedes
Accountable
Director
Policy Author Lead
Consultation
Circulation
Approval by
Supersedes 1
Description of amendments Updated in line with new legislation
Lead for NHS Continuing Care
Moira Angel
Designation
Designation
Circulation List
Committees/Groups
Consulted Date
Executive Director
Name/Date
Associate Director of Nursing and
Quality
Johnette Irving
Nurse Development Lead
Joint Commissioning Group
Public Engagement Team/Patient
Voice
Clinical Leads for Provider Services
Joint Commissioning Group
DATE: July 2009
Circulation
Trust Board Date
Issue Date
Circulated by
Chief Operating Officer approved circulation of the document to participating organisations July
2009
Review
Monitoring
Audit Tool
Equality
Impact
Assessment
Issued to
Review Date
Responsibility of
Use standard template and attach to policy
See Appendix
Initial Assessment completed
Full Assessment completed
April 2012
Johnette Irving
YES
YES
NO
Discharge and Transfer of Home of Choice Policy September 2010
2 of 114
Version Control Sheet
Version Date
1
2.0
2.1
2.2
2.3
2.4
2.5
2.6
2.7
09/09
11/09
04/10
04/10
04/10
04/10
Author
J. Irving
J. Irving
J. Irving
J. Irving
J. Irving
20/09/2010 J Irving
28/09/10
28/09/10
J.Irving
J.Irving
Status Comment
Archived to S:drive
Update - NHS Continuing Care
(Section 6)
Add - Information Governance relating to sharing patient information between organisations (Section 24)
Added to Responsibilities for Paediatric
Services reference to Safeguarding
Children’s policy and Cumbria Local
Safeguarding Children Board
Added to Complex Discharge Planning
- 5.17 Reference to Safeguarding
Adults Policy & Safeguarding Adults reporting process
Home of Choice became Section 8 of this document
Added Section Carers, Definition
Nurse-led Discharge to Glossary
Updated PVG Comments
Updated Standards and Quality
Committee comments - shorten policy statement, discharge to take place over
7 days a week.
Added to introduction - consent of patient must be obtained…, changed
“cases” to patients in Simple
Discharge, added patient consent to
Home of Choice - sharing, section
24.9.8
Discharge and Transfer of Home of Choice Policy September 2010
3 of 114
TABLE OF CONTENTS
3.3 Quick Reference - Flowcharts - Discharge Process ........................................ 9
SECTION 1 – Discharge Processes and Role Responsibilities ............................. 10
3.4 The Start of the Discharge Process for: Emergency and Elective
3.6 Department Of Health Discharge Pathway ..................................................... 12
Consideration of NHS Continuing Healthcare .......................................... 20
Initial Screening - NHS Continuing Healthcare Needs Checklist ....................... 20
SECTION 2 – Referral to Social Services/ Delayed Discharge & Reimbursement 24
Additional Responsibilities for Referral to Social Services / Delayed
Discharge and Reimbursement - ................................................................... 24
Hospital Referrals to Social Services ........................................................ 24
Transfer of Care and Reimbursement Liability ......................................... 26
Local Agreed Definitions of Delayed Transfers of Care ........................... 27
SECTION 3 – Multi-Disciplinary Team, Liaison Nurse, Discharge Co-ordinator etc.
8. Responsibilities of the Multi-disciplinary Team ........................................... 29
Roles of other Multi-disciplinary Team Members ..................................... 29
Discharge and Home of Choice Policy September 2010
4
Of
114
9. Additional Responsibilities of the Liaison Nurse Discharge Co-ordinator /
Nurse in Charge-Community Hospitals / Step-Up/Step-Down Units .......... 31
– Transport and Transfer to Community Hospitals/Services ............. 33
Responsibilities Relating to Arrangements for Transport .......................... 33
Additional Responsibilities for Transfer or Admission to Community
VERBAL HANDOVER FORM FOR STEPDOWN PATIENTS ...................... 37
12. Additional Information on “Short-Term Interventions” [STINT] .................. 41
SECTION 5 – Issue and Prescribing of Medicines, Dressing & Appliances, Home
13.5 Process – ordering Take Home Medications ......................................... 45
Process - ordering Take Home Dressings and Appliances ..................... 46
Responsibilities relating to the supply of Intermittent Home Oxygen ....... 47
Responsibilities Relating to Infection Control .............................................. 48
SECTION 6 – Responsibilities for Patients with Added Needs .............................. 49
Additional responsibilities relating to
Additional Responsibilities for Maternity Services ...................................... 51
18. Additional Responsibilities for Paediatric Services ..................................... 53
Additional Responsibilities for Palliative Care ............................................. 56
20. Additional responsibilities for Homeless Persons or Persons with Housing
Additional Responsibilities for Transfer of Prisoners ................................. 59
– Refusal of Treatment / Self-Discharge .............................................. 62
Additional Responsibilities where Patients Self Discharge ........................ 62
“Home of Choice” - additional guidance .......................................... 64
24.5 Process to apply for Patients Waiting in Hospital for a Nursing Home or
Discharge and Home of Choice Policy September 2010
5
Of
114
24.8 Process To Apply For Patients Waiting In Hospital For A Nursing Or
24.9. Guidance Notes Agreed By Partners Which Apply To Home Of Choice . 73
SECTION 9 – Monitoring the Discharge & Transfer Policy and benefits achieved
25.5 Discharge Policy Audit Tool - Primary / Community Care ................... 84
SECTION 10: - Governance of Information Related to Discharge and Transfer of
APPENDIX 2: Supporting Policies, Protocols and Documentation ....................... 92
APPENDIX 3: Underpinning Principles for Effective Discharge and Transfer of
Discharge from Hospital Pathway Process and Practice DOH 2003 ....... 94
3.2 Community Care [delayed discharges] Act [2003] ................................... 95
3.3 National Framework for NHS Continuing Healthcare and NHS Funded
3.6 Patient’s And Carer’s Discharge Standards ................................................ 102
DIX 4: Example of DH “DISCHARGE CHECKLIST” ................................. 103
TEMPLATE 1 – Training Needs Analysis and Training Plan ... Ошибка! Закладка не определена.
TEMPLATE 2 - Document Implementation Effectiveness Audit Tool ..........
Ошибка!
Закладка не определена.
TEMPLATE 3 – Generic Policy Equality Impact Assessment . Ошибка! Закладка не определена.
TEMPLATE 4– Glossary of Terms ...................... Ошибка! Закладка не определена.
TEMPLATE 5 – Consultation Circulation List ..... Ошибка! Закладка не определена.
TEMPLATE 6
– CONSULTATION CHECKLIST FOR INDIVIDUAL USE ........ Ошибка!
Закладка не определена.
TEMPLATE 7 – CONSULTATION CHECKLIST FOR PATIENT VOICE GROUP
..................................................................... Ошибка! Закладка не определена.
TEMPLATE 8
– AUTHOR’S SUMMARY OF CONSULTATION COMMENTS (FOR
AUTHOR USE ONLY) ................................. Ошибка! Закладка не определена.
TEMPLATE 9 – IMPLEMENTATION TEMPLATE . Ошибка! Закладка не определена.
Discharge and Home of Choice Policy September 2010
6
Of
114
TEMPLATE 10 - POLICY ADVISORY GROUP CHECKLIST ...... Ошибка! Закладка не определена.
Discharge and Home of Choice Policy September 2010
7
Of
114
1 Introduction
A review of the discharge and home of choice policies was undertaken in order to take account of a number of initiatives which have been introduced since the original policies in 2006, which have a bearing on the discharge process.
These include:
Case Management - as an integral part of practice
NHS Continuing Healthcare - NHS Funded Nursing Care
Closer to Home - Transforming Community Services
Development of Community Hospitals & Step-Up / Step-down Units
Community-based, integrated Health & Social Care Teams - Short term interventions [STINT] which integrates rapid response, intermediate care, generic domiciliary care, rehabilitation, re-enablement & interim care
Community Hubs
Primary Care Assessment Service
Long-Term Conditions Specialist Teams
Extended role of Community Physiotherapists
Locality Commissioning
Discharge is a process and not an isolated event. It has to be planned for at the earliest opportunity across the primary, hospital and social care services, ensuring that people who use the services and their carer (s) understand and are able to contribute to care planning decisions as appropriate. It is part of an ongoing process that should start prior to admission for planned admissions, and as soon as possible for all other admissions. This involves building on, or adding to, any assessments undertaken prior to admission.
For people who are receiving care from mental and learning disability services or midwifery services, hospital discharge may not be a point of discharge from care, but a transfer in location in the delivery of care.
For the successful discharge/transfer of the patient to take place it is essential that there is good communication in an appropriate language/format between all parties involved. And, adherence to information sharing / disclosure agreements supports respect of the patient throughout the management of consent and confidentiality. The consent of the patient or their appointed representative must be obtained and any transfers of information should be accurately recorded in the patient’s health record.
2 Purpose of Policy
The purpose of this policy is to facilitate a timely, appropriate, safe discharge, for patients who no longer require acute and or/ inpatient care.
Discharge and Home of Choice Policy September 2010
8 of 114
The objective of the policy and benefits to be achieved are to:
Ensure that people who use services and their carers are actively engaged in the planning of discharge
Ensure effective communication between in-patient and community services
Facilitate the discharge of people who use services in a timely manner
Ensure a safe and supportive discharge
Ensure that information, medication and equipment, as appropriate is provided to facilitate appropriate care
Ensure that discharge planning starts before or on admission with full multi-disciplinary assessments
Ensure the identification of a key person, usually the named nurse/care coordinator who will co-ordinate the discharge process
Ensure that people who use services who may be vulnerable are given particular attention when planning discharge
Ensure that funding decisions are made in a way that does not delay discharge
3 Scope of Document
The revised document covers Discharge and Transfer and Home of Choice and is a working document. It uses the pathways for simple, complex and continuing care discharge processes which include clearly defined actions and time-lines. It recommends audit trails which can be used to ensure that best practice for discharge is in place throughout the patient journey.
3.1 Statement of Intent
In order to improve patient experience and patient flows, the Discharge and
Transfer and Home of Choice Policy advises the following takes place:
Regular training for health and social care professionals to ensure there is a wide range of staff readily available who are competent to initiate and expedite discharge
Ensuring issues that might affect discharge are identified at the earliest stage
Ensuring there is a process in place to systematically evaluate “lessons learned” from discharges and a mechanism to ensure improvements are implemented where needed in a timely manner
Ensuring the discharge process is effective so that discharge from hospital takes place over 7 days a week.
3.2 Staff Groups Policy is applicable to:
All staff who participate in or facilitate the discharge or transfer of patients from inpatient settings in both Acute and Community Hospitals and Step-
Discharge and Home of Choice Policy September 2010
9 of 114
Up/Step-Down Units in Cumbria. The Policy is relevant to staff working in
Adult Social and Cultural Services, Cumbria County Council; Cumbria
Partnership NHS Foundation Trust; NHS Cumbria, North Cumbria University
Hospital NHS Trust; Northwest Ambulance Service NHS Trust and University
Hospitals of Morecambe Bay - South Cumbria.
3.3 Quick Reference - Flowcharts - Discharge Process
Start of Discharge from Emergency and Elective Admissions [p.10]
Model of Simple / Complex Discharge [p.11]
Department of Health Discharge Pathway [p.12]
Flowchart Mapping Process of eligibility for NHS Continuing Care / NHS
Funded Care [see section 6.7]
Pathway for Long Term Care [Residential Placement] [see section 5.18, p.19]
Discharge and Home of Choice Policy September 2010
10 of 114
SECTION 1 – Discharge Processes and Role Responsibilities
3.4 The Start of the Discharge Process for: Emergency and Elective
Admissions
Emergency Elective
TRIAGE
Identify those on
Liverpool Care
Pathway for the
Dying - refer to pathway - discharge to patient’s preferred place of care
Initial Assessment,
Intervention, Treatment
Patient
Agree - NO
Decision to Admit - discuss with patient and/or carers
Patient
Agree - YES
Follow-up
Required -
NO
Follow-up
Required -
YES
Further assessment and diagnosis
Clinical
Functional
Social
Pre- admission assessment
Clinical
Functional
Social
Length of Stay
Complete Refusal of Treatment
Form / Take Home medications, dressings, prescriptions
Contact GP and/or DN
OR
Community Hub
OR
Out of Hours- Cumbria-
24/7 immediately to arrange follow-up [document]
Referral to MDT Professional for Assessment of
Complex Need if Necessary
Initial Clinical
Management Plan -
Patient admitted for elective episode
Estimated Date of Discharge is based on Anticipated Length of Stay – determined at preadmission or within 24 hrs of admission . Reviewed daily – becomes Expected Date of
Discharge – and finally 11 of 114 based on criteria - patient no longer requires acute care & is safe to discharge.
Make appropriate referrals to
AHP’s, social services,
STINT
& community services
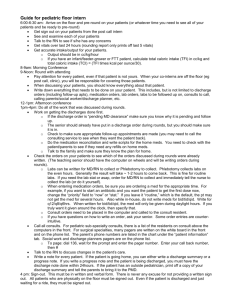
3.5 Model of Simple/Complex Discharge
COMPLEX
Discharge
DECISION TO
ADMIT
Requires multidisciplinary input
INITIAL ASSESSMENT by professional, involving patient/carers
Identify need for multidisciplinary input to facilitate discharge/transfer of care (refers to input other than existing care package
MDT to confirm discharge date & transfer destination in consultation with patient/carers
Not mentally & physically independent, and/or carers unable to fulfil care needs
SIMPLE
Discharge
No predicted requirement for multidisciplinary input to facilitate discharge
Inform patient/carers of anticipated discharge date
Continuing assessment/review pre-discharge
Continuing assessment/ ongoing arrangements for transfer/discharge
Mentally and physically independent or care arrangements fulfil care needs.
Finalise discharge arrangements.
Document in patient record
DISCHARGE
/TRANSFER
Finalise discharge arrangements.
Document in patient record
Mentally and physically independent or care arrangements fulfil care needs
Discharge and Home of Choice Policy September 2010
12 of 114
3.6 Department Of Health Discharge Pathway
[NOTE: Key Worker = use title appropriate to local arrangements e.g Care Coordinator etc.]
Care Options
Home with extra support
Short-term Intervention Team placement
Admit patient to Acute Inpatient
Allocated to Key Worker to support MDT and Co-ordinate assessment
Identify and engage Carer/s
Provide patient and Carer with relevant information
Agree estimated date of discharge based on anticipated length of stay
Pre Admission Screening
Assessment A&E + MAU + PCAS
Complete Admission Assessment and documentation
Identify any additional health and social care discharge needs
Additional Needs No
Within
24 Hours
Key worker – co-ordinate assessment during hospital stay
Daily review of Care Plan -
Expected Date of Discharge
Progress/chase referrals
Co-ordinate discharge plan
Key worker to coordinate referral (using
Referral Protocols)
Yes
Any problems
No
Hospital Based Services
Medical Team therapy diagnostics
I ntegrated Health & Social Care
Discharge Planning Team:
Community based health and social care services
NHS Continuing Care & application of Eligibility
Criteria (EC)
Does not meet EC for NHS
Continuing Care
Multi Disciplinary Assessment involving Patient and their Carer – Determining Care options: Short term Interventions, Community Hospital ,Care at
Home
Transitional/step-down facility
NHS Continuing Care/Care Home
Transfer to
Short Term interventions
Additional Needs
Patient having a new/ increased package of care at home or a new
Care Home Placement
Any problems
Non complex Needs discuss with patient and carer outcome of assessment and agree needs
No additional needs
Application Eligibility Criteria for Continuing Health &
Social Care
Patient and carer agree
Yes
No Key worker liaise with Discharge Planning Team to review assessment and care pathway
Consider transfer to stepdown or transitional facility awaiting outcome of arbitration
Arbitration
Await Outcome
Services if any arranged
Key worker to complete Discharge Information and co-ordinate Discharge Plan . Patient must agree services arranged – decision documented in notes. Give preliminary Discharge Letter & information sheet to patient and carer and Discharge Summary to GP- within 48 HRS [2009] .
Discharge Transfer
Discharge and Home of Choice Policy September 2010
13 of 114
4 Simple Discharge Planning
4.1 Definition
The action needed in the discharge planning for these patients does not usually require the involvement of a full multi-disciplinary team or require the involvement of another agency.
Patients with simple discharge needs are defined as those;
being discharged to their own home or usual place of residency having simple ongoing care needs that do not require complex planning or delivery
In addition they;
are identified on assessment as having a predicted length of stay
no longer require acute care
can be discharged from Accident & Emergency, Primary Care
Assessment Service, Step-up/Step-down Units,
In-Patient wards or other assessment units
4.2 Process
Staff should refer to the Simple pathway section of the simple/complex flowchart (3.5, p11)
Following admission to accident & emergency, primary care assessment service, step-up/step-down unit or in-patient ward an initial assessment, intervention/treatment regime will be undertaken. A clinical management plan will be formulated.
Further assessment and diagnosis of the clinical, functional and social needs of the patient will be determined.
4.3 The estimated date of discharge will be discussed with the patient and will be documented in the patient record. The estimated date of discharge is identified early as part of the patient’s assessment and within 24 hours of admission [or pre-assessment for elective patients].
It is based on the anticipated time needed for tests and interventions to be carried out and for the patient to be clinically stable and fit for discharge.
The patient and carer are involved and informed about the clinical management plan and the estimated date of discharge.
Discharge and Home of Choice Policy September 2010
14 of 114
4.4 A daily review of the patient’s condition and response to treatment will determine if the estimated date of discharge needs to be revised. A firmer date for discharge will be given; this will constitute the expected date of discharge.
4.5 A discharge checklist will be completed 24 hours before discharge by ward staff to ensure all discharge requirements are in place, and this will be retained in the patient record. [Example of DH discharge checklist in
Appendix 4 pp 104 - 110]
4.6 On the day of discharge the patient will meet the criteria for discharge which is acute care is no longer required and the patient is safe. This will be recorded in the patient record.
4.7 The Patient will be given a discharge letter at the time of discharge and any Social Services Benefit Sickness Certificate requested by the Patient.
(Guidance on Social Security Benefits should be available for patients who require information).
4.8 The letter is for the Patient to use in the event of any query or concern immediately following discharge, containing information about the
Patient’s treatment, including without limitation:
the Patient’s demographics
the dates of the Patient’s admission and discharge details of any clinical procedure undertaken the name of the Patient’s responsible Lead Clinician, Consultant or Doctor at the time of the Patient’s discharge
details of any medication prescribed at the time of discharge
[medications stopped during admission / reason, change in
dosage / reason] any other relevant or necessary information or instructions contact details for Provider’s facility
4.9
A discharge summary will be sent to the Patient’s GP within 24 hours of the patient’s discharge. The discharge summary needs to be available to the receiving doctor when the patient is next seen.
4.10 The discharge summary shall be easily legible and contain without limitation:
the date of the Patient’s admission the date of the Patient’s discharge details of any Services provided to the Patient, including any operation(s) and diagnostic procedures performed and their
outcomes a summary of the key diagnosis made during the Patient’s admission details of any medication prescribed at the time of the Patient’s discharge [medications stopped during admission / reason, change in dosage / reason]
Discharge and Home of Choice Policy September 2010
15 of 114
any adverse reactions or allergies to medications or treatments observed in the Patient during admission
the name of the responsible Consultant / Doctor at the time of the Patient’s discharge
any immediate post-discharge requirement from the primary healthcare team
any planned follow-up arrangements whether the Patient has any relevant infection, for example
MRSA
the name and position of the person to whom questions about the contents of the Discharge Summary may be addressed, and complete and accurate contact details (including a telephone number) for that person
4.11 Discharge summaries need to be multi-disciplinary where multidisciplinary care is to be continued.
The Discharge Summary should be validated by a responsible clinician.
4.12 The patient must be informed as to what information will be communicated to which other doctors involved in their care, and given the opportunity to consent. This should be documented in the patient record in accordance with the GMC guidance.
4.13 Where patients wish to leave a care setting against professional advice the process must be followed - refer to section 7 in this document.
4.14 Patients who follow the simple discharge pathway will not be subjected to a case conference.
4.15 Arrangements for transport of patients are to be found at section 4-10 of this document.
4.16 Arrangements for medications, dressings and appliances are to be found at section 5-13 of this document.
4.13 For out of hours discharge refer to Complex Discharge 5.12 in this document.
Discharge and Home of Choice Policy September 2010
16 of 114
5 Complex Discharge Planning
5.1 Definition
Patients who are in hospital with complex needs will require referral for assessment by a range of members of the multi-disciplinary team, or the involvement of another agency or care provider.
Patients who have complex discharge needs are defined as;
Patients would be discharged home or to a carers home or to intermediate care or to a residential or nursing care home.
And
Who have complex ongoing health and social care needs which require detailed assessment, planning and delivery by the multi-disciplinary team and multi-agency working.
And
Whose length of stay is more difficult to predict (Source DOH).
5.1.1 Following admission of a person to an acute or community hospital ward or step-up/step down unit, multi-disciplinary assessment and discharge planning will commence.
5.1.2 Where a patient has a known community matron/care manager/care coordinator, district nurse or social worker, they should be contacted as soon as possible to ensure that they are fully involved with, and where appropriate co-ordinate, the discharge planning process. This information may be available in some areas by contacting the
Community Hub.
5.2 Process
Staff should refer to the Complex pathway section of the simple/complex flowchart [2, p11]
5.2.1Following admission to accident & emergency, primary care assessment service, step-up/step-down unit or in-patient ward an initial assessment, intervention/treatment regime will be undertaken. A clinical management plan will be formulated [see flowchart 1, start of discharge process].
5.2.2 Further assessment and diagnosis of the clinical, functional and social needs of the patient will be determined. This will require referral to
Discharge and Home of Choice Policy September 2010
17 of 114
members of the multi-disciplinary team, social care and in some cases other agencies.
5.2.3 The patient and carer are involved and informed about the clinical management plan and assessments.
5.2.4
A daily review of the patient’s condition and response to treatment will determine how soon the estimated date of discharge can be established. This is based on the anticipated time needed for tests, interventions and assessments to be carried out and for the patient to be safe for discharge.
5.2.5 During the course of assessment, a named person will be identified to co-ordinate the discharge. This could be the nurse or if appropriate another member of the multi-disciplinary team.
5.2.6 During the course of intervention the estimated date of discharge will be reviewed daily by the appropriate members of the multi-disciplinary team and a firmer date of discharge will be given. This will constitute the “Expected Date of Discharge”. Following further intervention/ treatment the multi-disciplinary team will confirm a discharge date stating when the patient will be ready and safe for discharge. This is the “Proposed Date of Discharge”; when there is a statutory duty to notify Adult and Cultural Services of the Proposed Discharge Date.
5.2.7 Patients with complex needs may require a case conference, if the patient requires packages of care for the first time; or the patients needs have changed significantly during the admission; or the patient is being considered for transfer to long-term care. This should be considered on an individual basis by the case coordinator / community liaison nurse.
5.2.8 Where long term care [residential placement] is being considered the pathway to long term care should be followed (refer to 5.14).
5.2.9 Where patients can be pre-assessed prior to admission, discharge planning will commence during the pre-admission phase in liaison with the community matron/care manager/care co-ordinator if there is one designated to the patient.
5.3 Upon admission, the Single Assessment Process will be used as the initial assessment tool.
5.4 Following admission, the discharge/transfer of care pathway will be followed (flowchart 3)
5.4.1 The nursing staff will, in liaison with other people identified in the discharge plan, ensure that treatment and discharge plans are followed as indicated in the relevant care pathway.
5.5 Throughout the process, Trust and Professional documentation standards will be adhered to. For content of Discharge Letters and
Discharge and Home of Choice Policy September 2010
18 of 114
process follow guidance 4.8, for Discharge Summaries refer to guidance at 4.10.
5.6 A discharge planning check list will be completed and retained in the patient record [example of discharge planning checklist from DH –
Appendix 4]
5.7 When a patient is to be transferred to another care setting, an up to date clinical management plan will be copied and forwarded [for transfer to community hospital, see section 4/10 in this document ]
5.8 The patient must be informed as to what information will be communicated to which other doctors involved in their care, and given the opportunity to object. This should be documented in the patient record in accordance with the GMC guidance.
5.9 Where patients wish to leave a care setting against professional advice the process must be followed - in section 7/23 of this document
5.10 Arrangements for transport of patients are to be found at section 4/10 in this document.
5.11 Arrangements for medications, dressings and appliances see section
5/13 in this document.
5.12 Out of Hours
Wherever possible patients should not be discharged / transferred out of hours, as this should be planned. When out of hours discharge/transfer occurs the local agreed dispensing procedure whereby medical or agreed nursing staff can dispense certain drugs in order to facilitate the discharge/transfer can take place. Any outpatient appointments can be made in hours and forwarded onto the patient, and if transport is required the staff will follow the transport guidelines and policy.
5.13 Safeguarding Adults
All concerns regarding the safety or abuse of a vulnerable adult needs to be reported and properly investigated before discharge arrangements are finalised. For further information see “Safeguarding
Adults Policy CPCT/001/027 - with particular reference to Appendix 3 -
Safeguarding Adults Reporting Process.
Discharge and Home of Choice Policy September 2010
19 of 114
5.14 Pathway to Long Term Care
[Residential Placements]
1. Patient admitted to Acute - Community Hospital
2. Information gathering and Discharge Planning
Document:
Expected Date of Discharge
[EDD] based on
Anticipated
Length of Stay within 24 hours
3. Single Assessment Tool completed
4. Care Plan developed using Single Assessment
5. Case Conference/MDT involvement of family where appropriate
Follow Home of Choice Policy
6. Follow Continuing Care Process
Review
Expected Date of Discharge
DAILY
Agree Date of
Discharge
Review Progress with Agreed
Date of
Discharge
DAILY 7. If Residential Placement is discharge destination- then the patient’s home of choice will further assess if they are able to meet patient’s needs
NO
Select another residential place and continue until suitable placement is found
Re-establish agreed Date of
Discharge
YES
Care plan drawn up, signed and agreed to include medical issues
Note: for a small group of individuals transition into the community becomes delayed for numerous reasons. See escalation in
Home of Choice policy which is intended to aid the resolution of any difficulties that patients are experiencing with being discharged from hospital in a timely manner
Admit to Residential Place
Follow up with Post-
Admission Review [Joint
Review]
Discharge and Home of Choice Policy September 2010
20 of 114
6 Planning for Continuing Care
NHS bodies and Local Authorities carry a responsibility to ensure that the assessment of eligibility for and provision of, continuing care takes place in an appropriate and consistent manner.
Definition
Continuing Care is a term that describes care needed over an extended period of time as a result of:
Disability
Accident
Illness
Care provided may cover both physical and mental health needs and it may be provided in a range of settings:
NHS Hospital
Nursing Care Home
Residential Care Home
Independent Hospital
Patient’s Own Home
6.1 NHS Continuing Healthcare
Is a package of continuing care arranged and funded solely by the NHS.
The actual services that are provided as part of that package should be seen in the wider context of best practice and service development for each client group.
6.2 Consideration of NHS Continuing Healthcare
Every patient over age 18, who may have continuing care needs must be screened for eligibility for NHS Continuing Healthcare before any long term plans are put in place.
NHS Continuing Healthcare links with the complex discharge planning process. The nominated person to manage the NHS Continuing Healthcare assessment process is identified at the multidisciplinary case conference.
The screening is undertaken when the patient is ready for discharge, and in sufficient time for all assessments to be completed so not to delay discharge.
Initial Screening - NHS Continuing Healthcare Needs Checklist
6.3.1. In the first instance, the patient is screened using the NHS Continuing
Healthcare Needs Checklist, which must only be filled out by health and
Discharge and Home of Choice Policy September 2010
21 of 114
social care staff who have completed training as supported by the
Clinical Leads for NHS Continuing Healthcare in the localities. The initial screening is undertaken once all relevant clinical, social, risk assessments and care plans have been completed. These assessments provide evidence which is necessary to support the outcome of the screening tool and help towards the completion of the decision-support tool.
6.4 Full consideration
6.4.1 A Decision-Support Tool for NHS Continuing Healthcare is completed when the NHS Continuing Healthcare Needs Checklist indicates any of the following:
Two or more ticks in column A
Five or more ticks in column B
One tick in column A in one of the boxes marked with an asterisk* and any number of ticks in column B [*these are the domains which carry a priority level in the Decision Support
Tool]
Where circumstances dictate a full consideration be undertaken, even though the individual does not apparently meet the indicated threshold
6.4.2 The Decision-Support Tool for NHS Continuing Healthcare and verification evidence is sent to the appropriate / relevant Clinical Lead for NHS Funded Care for presentation to a county-wide, multidisciplinary panel when:
Criteria from the NHS Continuing Healthcare Needs Checklist is met
Clear recommendations from the Multidisciplinary Team are agreed and documented
Assessments and verification evidence is complete
6.4.3 Verification evidence is crucial. The process will be delayed if evidence has not been provided. The coordinator collates the evidence supplied by Health Professionals and Carers, and only up to date and relevant evidence used at the Multi-disciplinary Team is appropriate.
6.5 Notification of Panel Decision
6.5.1 The Clinical Lead for NHS Funded Care will notify the Care Coordinator of the panel decision by telephone, on the same day.
6.5.2 A formal notification will be sent to the Care Coordinator, Patient or their Power of Attorney as indicated, by post.
Discharge and Home of Choice Policy September 2010
22 of 114
6.6 Fast Track
6.6.1 Clients with a rapidly deteriorating condition or who may be entering a terminal phase will be considered a priority, and a decision on eligibility
/ NHS Continuing Healthcare will be made as a matter of urgency.
[Note: Fast-track requires specific health needs to be identified, and cannot be enacted on diagnosis alone].
Discharge and Home of Choice Policy September 2010
23 of 114
6.7 Flowchart -Mapping Process of eligibility for NHS Continuing
Healthcare and NHS Funded Nursing Care - in Cumbria
DRAFT - REVISED GUIDANCE JULY 2009.
PROCESS FOR NHS CONTINUNG HEALTHCARE NHS FUNDED
NURSING CARE IN CUMBRIA
Individual identified as having ongoing care needs (when all other enablement options e.g.
Intermediate Care, Step Up-Step Down and Rehabilitation have been completed
Informed consent obtained if consent cannot be gained refer to National Framework and
Mental capacity act
NHS CHECKLIST
Checklist completed as per National Framework
Recorded decision on file
Professional Health lead initiates appropriate onward pathway. When
Guidance – Checklist Tool
Best practise advises Checklist should be completed jointly with Health and Adult Social Care professionals
Individual to be given copy of Public Information
Screened out
Adult Social Care are involved a copy should be sent to the Team Manager
Where Adult Social Care are in disagreement proceed via Dispute documentation
Send completed checklist to Locality CHC clinical lead
Procedure
Where FNC is required copy to PCT to notify of review
Where family is in disagreement proceed via Review Procedure
PROCEED TO COMPLETION OF DECISION SUPPORT TOOL (DST)
Refer to Appendix 1 of this Guidance on ‘How to facilitate a successful
Multi-Disciplinary Team (MDT) meeting’
Key Points
Membership
Timescales
Clear Recommendation and Recording
All DST completed to be sent to Locality CHC clinical lead
ELIGIBILITY MET FOR
FULLY FUNDED
CONTINUING HEALTH
CARE
Primary Health need established then clear recommendation made
DST and documentation sent to
Clinical Lead
JOINTLY
COMMISSIONED
PACKAGE
Health needs to be clearly identified above and beyond mainstream services
Adult Social Care needs to meet Fair
Access to Care Criteria
ELIGIBILITY
NOT MET
TO PCT FUNDED CARE PANEL FOR RATIFICATION
Fully funded CHC packages to be commissioned and care managed by Health
Joint packages – determine respective funding responsibility and care management
arrangements
If disputed refer to dispute policy http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuida nce/DH_076288
ALL CASES INCLUDING FNC TO BE REVIEWED AFTER 12 WEEKS THEN ON
ANNUAL BASIS OR SOONER IF APPROPRIATE
Discharge and Home of Choice Policy September 2010
24 of 114
SECTION 2 – Referral to Social Services/ Delayed Discharge &
Reimbursement
7. Additional Responsibilities for Referral to Social
Services / Delayed Discharge and Reimbursement -
Adherence to information sharing / disclosure agreements must support respect of the patient throughout the management of consent and confidentiality.
7.1 Hospital Referrals to Social Services
In order to comply with the Community Care (Delayed Discharges) Act
(2003) it is important that referrals to, and communications with, social workers are documented and the agreed procedure is followed. The good practice of identifying potential social care needs as early as possible after admission is assumed to continue. Patients will be screened to determine whether they meet NHS continuing care criteria.
If they do not meet NHS Continuing Care criteria, Adult Social Care will be informed and will carry out an assessment. A copy of the screening assessment will be sent to the Team Manager in Adult Social Care.
When predicting future care needs, consideration should be given to the potential for further rehabilitation or the impact of any treatments that may affect the outcome for the patient. Referrals to social workers will only be made with the consent of the patient.
The referral will be submitted on a Single Assessment contact one referral form.
This constitutes Section 2 Notification
7.1.1 Upon receipt of the contact one referral the Adult Social Care and Cultural Services Directorate will undertake the necessary assessment and arrange for a social care package to support the safe discharge from hospital.
7.1.2 The discharge date will be agreed by the clinician and the multidisciplinary team when care in an acute setting is no longer required and the patient is safe for discharge. Patients may be fit for discharge who are not clinically stable, but who can be managed safely at home or in the community with input from services for example: Short-Term Interventions [STINT].
This constitutes Section 5 Notification
Note
Please note Section 2 and Section 5 Notifications can be given at the time that the initial referral is made provided that the discharge date is known and it is made clear that it is the proposed / agreed discharge date.
Discharge and Home of Choice Policy September 2010
25 of 114
7.1.3 Referral to Social Services
YES
Contact
STINT
Is the patient suitable for referral to
Short Term Interventions [STINT]
NO
Discuss with the patient and relatives regarding agreement to refer to social services
NO
Cannot be referred to
Social
Services
YES
Complete SECTION 2 NOTIFICATION
WHEN
As indicated by assessment of individual patient
If issues regarding discharge develop during patient journey
WHY
Gives notification to Social Services of patient who will potentially need new or restart of services on discharge
Begins planning process jointly between NHS and Social Services
Identifies patients who need assistance re. Personal care, support on discharge, has long term need or no rehab potential
Present care placement identified as no longer adequate
A reassessment identifies need to increase care package
HOW
Complete Section 2 notification documentation, send to Social Services Team
Complete Continuing Health Care Screening Tool
Ensure Expected Date of Discharge is written in the allocated space
WHAT NEXT
Social Services will prioritise assessments for urgent discharges and those with special circumstances such as “care for the dying” Maximum time for commencing assessment is 48 hours
Completion of Section 5 Notification
WHEN
Agreed at MDT discussion
Communication ongoing with Social Service during the assessment period on their visits to see patient
When patient safe to discharge
WHY
10 This communication finalises the notification process confirming the date of discharge to Social Services.
HOW
11 Verbal agreement at MDT
12 Record agreed date of Discharge.
WHAT NEXT
Ensure organisational systems in place eg. Transport, pharmacy, documentation
Discharge and Home of Choice Policy September 2010
26 of 114
REIMBURSEMENT POLICY - SECTION 7 - UNDER REVIEW
7.2 Transfer of Care and Reimbursement Liability
7.2.1 Delayed transfers of care will be identified as described in the locally agreed definition document [see 7.3.]
7.2.2 Reimbursement liability commences on the day after the proposed / agreed discharge date as described in the Cumbria
Partnership Executive Reimbursement Protocol.
7.2.3
A patient’s status will only be identified as constituting a delayed transfer of care with a liability for reimbursement from the
Directorate of Adult Social Care and Cultural Services when the delay has been identified as solely the responsibility of Social
Services:
The assessment of social care needs has not been completed within the timescale specified in the local agreement (Cumbria Partnership Executive Reimbursement
Protocol).
Funding for long-term care is not available (NB current guidelines recommend that no patient should be transferred from an acute hospital setting direct into long-term residential or nursing care).
The local authority has not been able to make available a community care service that has been identified as essential to enable a safe transfer of a person to their own home.
7.2.4 The period of liability for reimbursement will end on the day that the local authority has completed the assessment of social care need and the identified social care resources are in place OR if the multi-disciplinary team assess that the patient is no longer fit for transfer from an acute hospital bed.
7.2.5 There will be no liability for reimbursement from the Adult
Social Care and Cultural Services Directorate for the following:
Lack of non-acute services, nursing home places
Lack of primary and community health care services.
Patient choice (refer to Patient Choice Directive and
Guidance)
Patient refusing to be transferred when considered fit for transfer.
The absence of intermediate care if it is assessed that the person could benefit from such a service.
Where the Adult Social Care and Cultural Directorate are assisting in procuring services for patients who will fund their own ongoing package of care.
Discharge and Home of Choice Policy September 2010
27 of 114
7.3 Local Agreed Definitions of Delayed Transfers of Care
7.3.1 A delayed transfer of care is when a patient is ready for transfer from an acute hospital bed but is occupying such a bed.
7.3.2 A patient is ready for transfer when:
A clinical decision has been made that the patient is ready for transfer
And
A multi-disciplinary team decision has been made that the patient is ready for transfer
And
The patient is safe to discharge or transfer
7.3.3 Reasons for Delay
Delay awaiting assessment
All patients, whose transfer of care is delayed due to waiting for the completion of an assessment of their future care needs and identifying and appropriate care setting. This can include any assessment by health and or social care professionals of a patients future care needs. Therefore delays can be due to either NHS, social services or a combination of both.
Delay Awaiting Public Funding
All patients whose assessment are complete but transfer has been delayed due to awaiting social service’s funding for residential or nursing care. This should also include cases where social services and NHS have failed to agree over funding for a joint package of care or an individual is disputing a decision over full funded NHS continuing care in the independent sector.
Delay Awaiting Further NHS Care, Including Intermediate Care
All patients whose assessment is complete but transfer is delayed due to awaiting further NHS care i.e. any non-acute health care including intermediate care. Also continuing care full funded by the NHS in the independent sector.
Delay Awaiting Residential/Nursing Home Placement Availability
All patients whose assessment is complete but transfer is delay awaiting residential/nursing home placement because of a lack of a suitable place to meet their assessed needs.
Discharge and Home of Choice Policy September 2010
28 of 114
Delay Due to Awaiting Domiciliary Care Package; Home
Adaptations and or Equipment
All patients whose assessment is complete but transfer is delayed due to awaiting a package of care, adaptations and equipment for their own home.
Delay Due to Patient or Family Exercising Choice
All patients whose assessment is complete but their transfer is delayed due to the patient and/or their family exercising their right of choice to choose a residential or nursing home under the
Direction of Choice following the agreement of social services funding. Or where patient who will be funding their own care are creating unreasonable delay in finding a place e.g. insisting on placement in a home with no foreseeable vacancies
Delay Due to Other Reasons
All patients whose assessment is complete but their transfer is delayed due to any other reason not previously stated.
Length of Delay
This should be measured from the point at which the patient was assessed as ready for transfer.
Discharge and Home of Choice Policy September 2010
29 of 114
SECTION 3 – Multi-Disciplinary Team, Liaison Nurse,
Discharge Co-ordinator etc.
8. Responsibilities of the Multi-disciplinary Team
The Multi-disciplinary team includes medical staff, nursing staff, a range of other hospital or community based healthcare professionals and social care staff. On occasions the voluntary sector may have a role to play in the discharge planning.
8.1 Role of Medical / Nursing Staff
8.1.1 The Medical or Nursing staff or Nurse Consultant will agree an expected discharge date with the multi-disciplinary team and the patient or their carer as appropriate, in accordance with section
5.2.6
of this policy.
8.1.2 The Medical or Nursing staff or Nurse Consultant will, as part of their role in the multi-disciplinary team, reach a decision on a proposed/ agreed date of discharge and the patient or their carer as appropriate, in accordance with section 5.2.6 of this policy.
8.1.3 Discharge documentation will be completed 24 hours prior to the proposed discharge or transfer date by the designated member of the Medical team.
8.1.4 Prescriptions and requisitions for appliances and dressings will be completed 72 hours prior to discharge / in time to ensure they are available at the time of discharge and discharge is not delayed. It should be documented that medicines reconciliation
/ adherence has been checked and is complete [as per 13.2
in this document].
8.1.5 A discharge letter will be compiled and given to the patient at the time of discharge as per guidance 4.8 in this document, by the designated medical and nursing staff.
8.1.6 A discharge summary will be compiled and sent to the Patient’s
GP within 24 hours of patients discharge as per guidance 4.10 in this document, by the designated medical staff. It will be validated by a responsible Consultant / Doctor [or Senior Nurse - in Nurse-led Units].
8.2 Roles of other Multi-disciplinary Team Members
8.2.1 Any member of the multi-disciplinary team who has been trained to undertake discharge responsibilities can be the responsible
Discharge and Home of Choice Policy September 2010
30 of 114
person for co-ordinating the transfer/discharge of the patient.
This will be determined by the needs of the patient and the skills of the relevant professional. At present it is usually the Named
Nurse who undertakes the role.
8.2.2 The nominated professional will ensure that all processes, investigations and interventions have been undertaken and completed prior to discharge or transfer. This will also include ensuring any identified carer is willing and able to continue in the caring role. Individual carers should be offered an individual carers assessment as required – see 16.2, 22.1.
8.2.3 The nominated professional will ensure that arrangements for discharge or transfer are in place 24 hours prior to the agreed discharge/transfer date.
8.2.4 The nominated professional will aim to ensure that all requirements to facilitate a safe discharge are in place. This may include dressings, medication and equipment.
8.2.5 Where patients and /or carers require education or training in the use of medicines, dressings or equipment this must be carried out prior to discharge and the patient and/or carer must be given all relevant information in written form. This training will be carried out by the relevant health professional involved. - see
13.4.2
8.2.6 Follow up appointments and referrals to other professionals or agencies will be discussed with the patients and/or carers.
Arrangements for these will be made prior to discharge or transfer.
Discharge and Home of Choice Policy September 2010
31 of 114
9. Additional Responsibilities of the Liaison Nurse Discharge
Co-ordinator / Nurse in Charge-Community Hospitals
/ Step-Up/Step-Down Units
9.1 The role of the Liaison Nurse/Discharge Co-ordinator/Nurse in Charge -
Community Hospital or Step-up/Step-down Unit is to ensure that the transfer of care is as appropriate, efficient and effective as possible.
This involves facilitating liaison and communication between all agencies involved in discharge / transfer planning. The Liaison Nurse /
Discharge Co-ordinator / Nurse in Charge Community Hospital or Stepup / Step-down Unit will help identify appropriate referrals to a range of services for example; Community Hospital, Short-term Interventions,
Primary Care Teams, Social Care Directorate and Voluntary Agencies.
9.2 The Liaison Nurse / Discharge Co-ordinator / Nurse in Charge -
Community Hospital or Step-Up/Step-down Unit may facilitate:
Input of information about community nursing care provided prior to admission.
Communication between the Community Nursing team, Community
Matron/Care Manager, Community Hospitals and Acute Hospital nursing teams, whilst the patient is in hospital.
Attendance of a member of the Community Nursing team or the
Care Manager at case conferences and home visits.
Attendance of Community Nursing staff on ward visits for observation of new treatments which may need to be continued at home.
Information exchange with Social Care Directorate.
Input of information on community policies or resources which may affect discharge or transfer. This may include information about
Voluntary Agencies within the community.
9.3 The Liaison Nurse / Discharge Co-ordinator / Sister - Community
Hospital or Step-Up/Step-down Unit can advise on procedures for arranging the loan of nursing equipment according to local provision.
9.4 The Liaison Nursing / Discharge Co-ordination team / Community Hub is responsible for providing wards and other relevant departments with contact numbers for Community Nursing services and for providing information about Community Hospitals. When the Liaison Nurse /
Discharge Co-ordinator / Nurse in Charge - Community Hospital or
Step-Up/Step-down Unit makes arrangements for discharge or transfer they are responsible for documenting this in the patient record.
Discharge and Home of Choice Policy September 2010
32 of 114
9.5 The Liaison Nurse / Discharge Co-ordinator / Nurse in Charge
Community Hospital or Step-Up/Step-down Unit is responsible for undertaking the NHS Record of Nursing Needs for patients transferring to nursing homes, including the NHS Continuing Healthcare Checklist and progression to Decision Support Tool as required for consideration for NHS Continuing Care Funding.
9.6 The Liaison Nurse / Discharge Co-ordinator / Nurse in Charge
Community Hospital is responsible for facilitating Complex Discharges including NHS Continuing Care and Joint Packages of Care.
9.7 The responsibility for co-ordinating case conferences lies with the lead professional, who may be the Liaison Nurse / Discharge Coordinator /
Nurse in Charge- Community Hospital or Step-Up/Step-down Unit.
9.8 The Liaison Nurse / Discharge Co-ordinator will represent NHS
Cumbria at the Adult Social Care Resource Monitoring meetings, per local arrangements.
Discharge and Home of Choice Policy September 2010
33 of 114
SECTION 4 – Transport and Transfer to Community
Hospitals/Services
10. Responsibilities Relating to Arrangements for Transport
10.1 All efforts should be made for the patients’ relatives to take the patient home unless there is a medical necessity for them to travel by
Ambulance. Provision of Ambulance Service transport for discharge can only be provided on medical grounds and must be authorised by the key worker co-ordinating the discharge.
10.2 The Ambulance Service will accept bookings for transport (normally
Patient Transport Service) on the day preceding discharge, exceptions to this will be made for patients being transferred for end of life care.
The Ambulance Service will take bookings based on the “predicted date of discharge”.
10.2.1 At the time of booking a unique reference number will be issued this must be used in any communication regarding the patient’s transport.
10.2.2 Special requests, which include the transportation of wheelchairs and zimmer frames, or where an escort is required, must be made at the time of the booking.
10.3 Patient luggage is restricted to two items only. It can only be transported if it can be secured within the vehicle. Items that cannot be secured will not be transported and the patient needs to be advised of this. The Healthcare Professional with the responsibility for coordinating discharge should ensure that alternative arrangements for transport of personal effects are made.
10.4 Patients should be collected from the discharge lounge/area. They will have been allocated to either morning or afternoon transport services.
Patients must be at the discharge lounge/area by either 0930hrs or
1300hrs.
10.4.1 Where there are unforeseen delays or higher than usual volumes of work the Patient Transport Services Control will inform the discharge lounge/area.
10.4.2 Patient Transport Services Control will provide the discharge lounge/area with information about the time slots allocated for the following day. Discharge lounge/area staff will notify the wards of the times allocated.
Discharge and Home of Choice Policy September 2010
34 of 114
10.5 Any requests for transportation should be made at the earliest opportunity. Early communication around a patient discharge should be made with the Ambulance Service to ensure all discharge issues have been addressed and that suitable transport is arranged well in advance.
10.6 Risk assessments and access information prior to patient discharge may be necessary. Early communication with the ambulance service regarding home transport and assessments should be made at the earliest opportunity when discharge planning is discussed. Contacting
Patient Transport Services 72 hours in advance gives time for assessment and issues which could prevent discharge home, to be addressed. Transporting patients upstairs is high risk and can only be undertaken if crews are able to safely manage the risk, which may require support from more than one crew.
10.7 Bariatric patients may need special transport and home assessment.
Early communication with the Ambulance Service is vital to ensure that adequate arrangements are in place to transport a Bariatric patient to their home.
10.8 It is the discharge teams ’ responsibility to ensure that all relevant medical history (including infection status, Do Not Resuscitate etc) is reported when transport is booked for ambulance crews information and appropriate action.
10.9 Patients with syringe drivers or subcutaneous pumps can be transported by Patient Transport Service (PTS) and Paramedic
Emergency Crews if the devices are “self-managing” and no intervention is required, other than stopping the machine if it is empty.
Please inform PTS control when booking transport.
10.10 Any requests for transportation out of hours, weekends or Bank
Holidays must be made in advance, before the day of discharge , as fewer crews and vehicles are available for patient transport services on these days/times. Unscheduled requests may put emergency services at risk if A&E vehicles are used for non-emergency activities.
Discharge and Home of Choice Policy September 2010
35 of 114
11. Additional Responsibilities for Transfer or Admission to
Community Hospitals
11.1 See 11.6 for a list of the conditions/requirements which may be considered suitable for admission to a Community Hospital.
Notify community hospitals before transfer of patients who require IV infusions, IV antibiotics and blood transfusions . To ensure arrangements are in place, for those hospitals where support from
District Nurses or IV Nurse Specialist may be required.
11.2 See 11.6 for a list of conditions / requirements unsuitable for admission to a Community Hospital.
11.3 IF YOU WISH TO TRANSFER A PATIENT, BUT ARE UNSURE IF
THEY ARE SUITABLE PLEASE DISCUSS WITH THE SISTER AT
THE COMMUNITY HOSPITAL
Hospital
Alston
Telephone
01434 381218
Brampton
Cockermouth
Keswick
Maryport
016977 2534
01900 820763
017687 67000
01900 812634
Millom
Penrith Carleton Ward
Penrith Jubilee Ward
Reiver House Carlisle
Wigton
Workington
Langdale North WGH
Langdale South WGH
Abbey View FGH
01229 772631
01768 245247
01768 245243
01228 592741
016973 66620
01900 705190
01539 795209
01539 795210
01229 491177
Copeland Unit WCH
11.4 Process
01946 693181
11.4.1 Follow local processes for identifying available beds in
Community Hospitals i.e. via Bed Managers
11.4.2 Irrespective of how the transfer of the patient has been arranged, (i.e. Step Down, from A&E etc) a verbal handover is given over the telephone and recorded using the
“Verbal
Handover Sheet ” (11.5). “ Cumbria Community Hospital /
SUSD Units Transfer Form for Stepdown Care” (11.6) should also be completed prior to the transfer of Step Down patients to a Community Hospital, by the Nurse responsible for transferring the patient from the Acute Trust.
Discharge and Home of Choice Policy September 2010
36 of 114
11.4.3 Except under exceptional circumstances the transfer should be a planned part of the care pathway for the patient and the patient should agree to the transfer, and the patients’ relative or significant other should be informed of the impending transfer.
11.4.4 Ideally patients who transfer to the units should reside in the locality to which they are being transferred to ensure efficient communication with other community services. However there will be exceptions to this, which will be managed on an individual basis.
11.4.5 Whenever possible admissions should occur within the normal working week. However Community Hospitals should if necessary admit patients 24 hours per day, 7 days per week.
11.4.6 On completion of the appropriate documentation the Nurse in charge can accept the patient, this decision can be supported by the GP, Matron / Bed Manager; should the care needs of the patient appear to be complex or out with the admitting criteria.
11.4.7 The ward staff must ensure that the transferring area sends the following with the patient
Transfer Letter / Management Plan
Medical and Nursing Notes
Transfer Medication
X-rays
Specialist equipment, where appropriate
“Cumbria Community Hospital / SUSD Units
Transfer Form for Stepdown Care”
11.4.8 It is the responsibility of secondary care to arrange patient transfer and, if required, to provide a Nurse Escort.
11.4.9 It is respons ibility of secondary care to ensure that the patient’s condition is assessed as safe to transfer and to inform the receiving ward if the patient’s condition changes following handover.
11.4.10 Failure by the transferring secondary care to provide the above must result in the completion of a NHS Cumbria Incident
Reporting Form so that systems can be improved, where appropriate and incidents investigated.
Discharge and Home of Choice Policy September 2010
37 of 114
11.5 VERBAL HANDOVER FORM FOR STEPDOWN PATIENTS
ENSURE “CUMBRIA COMMUNITY HOSPITAL / SUSD UNITS TRANSFER FORM FOR
STEPDOWN CARE” IS COMPLETED AND WILL BE TRANSFERED WITH THE
PATIENT
COMMUNITY HOSPITAL
PATIENTS NAME DoB
NHS No
NEXT OF KIN CONTACT No
AWARE OF TRANSFER YES NO
CONSULTANT
GP IS GP AWARE OF EXPECTED TRANSFER
INITIAL DATE OF ADMISSION TO HOSPITAL -
PLANNED EMERGENCY (PLEASE STATE)
REASON FOR ADMISSION
DIAGNOSIS
TRANSFER FROM HOSPITAL WARD
EXPECTED DATE OF TRANSFER TO COMM HOSP
PATIENT SCREENED FOR MRSA YES NO *
RESULTS
* please note all patients to be screened prior to transfer
PREDICTED DATE OF DISCHARGE
PREDICTED OUTCOME
OF ADMISSION
(PLEASE CIRCLE)
HOME
PALLIATIVE / TERMINAL CARE
RELOCATION TO NUSRING HOME / RES
CARE / SHELTERED ACCOMODATION OR OTHER
(Please Specify)
OTHER (Please Specify)
PAST MEDICAL HISTORY
TISSUE VIABILITY MOBILITY WASHING/
DRESSING
Discharge and Home of Choice Policy September 2010
38 of 114
DIET/SWALLOWING ISSUES COMMUNICATION CONTINENCE /
ELIMINATION
MENTAL STATE
ANXIOUS ABOUT TRANSFER
CONFUSED
WANDERING
A DANGER TO OTHERS / THEMSELVES
OTHER RELEVANT INFORMATION
SOCIAL
CIRCUMSTANCES
OTHER PROFESSIONAL INVOLVEMENT / REFERRALS MADE
MEDICATION ON TRANSFER SUPPLIED YES NO
CURRENT UP TO DATE DRUG CHART TO BE TRANSFERRED WITH THE PATIENT
HANDOVER RECEIVED FROM
HANDOVER RECEIVED BY
SIGNED DATE
SIG
Discharge and Home of Choice Policy September 2010
39 of 114
11.6 Cumbria Community Hospital/SUSD Unit transfer form for step down care
Step 1 - Contact nurse in charge at Community Hospital to agree transfer
Step 2 - Fix this form to front of patient note Step 3 Inform your bed manager of transfer
Name of Patient Date Time
Address
DOB Age
GP
Ward
Name and title of person making request for step down care
Is patient aware and accepting of this transfer
Yes
No
If patient unable to consent have NOK been informed Yes
No
Care management
When was the patient last medically reviewed? Date Time
Who medically reviewed the patient? Name Title
( Medical Review within the last 24 hrs is a requirement for transfer)
Have they clearly stated in the patients notes that this person is medically stable for step down care?
Yes
No
Diagnosis : current medical status: Include same day observations (important) and documented DNR notices
Clinical reason for move to Step Down Care. What care is being requested ?
Ongoing investigations - List any outstanding results
Has the patient an allocated social worker ? Please give name and progress:
Follow up plans/appointments
Discharge and Home of Choice Policy September 2010
40 of 114
Medications
Does the patient have an up-to-date, clearly written medication sheet? Yes
No
Are there sufficient medications being sent with the patient to cover the next 48hrs? Yes
No
(Adequate Medication for the next 48 hrs is a requirement for transfer)
Have any previous long term medications been stopped and why?
Infection Control Status -
What is the patient’s current status?
Patients suitable for admission to a
Community Hospital:
11 Patients with a condition not requiring
District General Hospital care, but who require nursing, medical or therapeutic invention.
12 Patients with an exacerbation of a known chronic illness who require treatment or rehabilitation.
13 Patients who require palliative or terminal care.
14 Patients who require a programme of rehabilitation.
15 Blood transfusion where cause of anaemia is known.
16 Intermittent or continuous intravenous or subcutaneous fluids.
17 Intravenous antibiotics in appropriate circumstances.
18 Patients who require a period of further medical / social assessment prior to determining long term care needs.
19 Patients who require step up – step down care.
Persons able to request step down care:
Consultant/specialist registrar/speciality doctor
Specialist nurse/nurse practitioner
Patients not suitable for admission to a Community Hospital include:
Acutely unwell patients with no known diagnosis.
Acute haemorrhage (e.g. GI bleeds).
Significant / severe stroke or any suspected stroke (in acute phase).
Acute chest pain / breathlessness.
Suspected pulmonary embolism.
Overdose – Drug overdose or alcohol intoxication
Surgical emergencies.
Gynaecological and surgical emergencies.
Acute onset of unconsciousness.
Children under the age of 16.
Patients having disruptive behaviour or complex psychiatric problems.
Persons able to request step up care:
GP
District nurse/case manager
Physiotherapist
Nurse practitioner/specialist nurse
PCAS doctor
Discharge and Home of Choice Policy September 2010
41 of 114
12. Additional Information on “Short-Term Interventions”
[STINT]
STINT is an integration of community-based services designed for rapid access which includes initiatives such as: intermediate care, rehabilitation, re-enablement, generic domiciliary care, rapid response and interim care.
The STINT service is accessible - 24 hours per day and 7 days per week. There are STINT services based in each locality.
Access is determined on need.
STINT offers short term care services for up to six weeks for adult service users aged 18 and over and their carers regardless of age or condition.
The service is aimed at people who do not require specialist acute care, but who require a short period of rehabilitation or intervention in a less intensive setting and where safe to do so, this will be the individual’s own home.
Each person will have an individualised care and management plan to inform and guide continued management of their care.
On-going problems will be addressed using management plans that reflect short, medium and longer term needs and include contingency plans and self-management strategies.
Individuals will have a robust discharge/exit plan included in their care plan, which might include onward referral to alternative support.
Discharge and Home of Choice Policy September 2010
42 of 114
12.1 Short Term Intervention Process Flow
Delivered by single service made of multiple functions
Includes Nursing, PT, OT, SW, Mental Health, Primary Care
Supported by single system of work
Includes documentation, budget, joint working, policies & systems
Aligned with other core services
Includes prevention, promotion & on-going care, specialist teams
Discharge and Home of Choice Policy September 2010
43 of 114
SECTION 5 – Issue and Prescribing of Medicines, Dressing &
Appliances, Home Oxygen, Infection Control
13.
Responsibilities Relating to Issue and Prescribing of Medicines
[dressings and appliances]
Medication errors are one of the leading causes of injury to hospital patients.
Therefore, every time a transfer of care takes place it is essential that accurate and reliable information about the patient’s medication is transferred at the same time.
13.1 Discharge Letter
13.1.1 It is imperative that the discharge letter contain a full and comprehensive list of all medications that a patient is currently taking
– including the name, dosage, frequency and route. This information should be clear, unambiguous and legible and available to the GP [or other Primary Care Prescriber] within 24 hours of the patient’s discharge. It should also be included in the District Nurse letter, especially in cases where the District Nurse is likely to visit before the
GP letter arrives, within the first 24 hours of discharge.
13.1.2 Information relating to medicine which should be included in the discharge letter:
A list of all medicines prescribed for the patient on discharge [and not just those dispensed at the time of discharge]
Dose, frequency, formulation and route of all the medicines listed
Medicines stopped and started, with reasons
Length of courses where appropriate [e.g. antibiotics]
Details of variable dosage regimes [e.g. oral corticosteroids, warfarin etc.]
Known allergies, hypersensitivities and previous drug interactions
Any additional patient information provided such as corticosteroid record cards, anticoagulant books, etc.
13.2 Medicines Reconciliation
13.2.1 Defined as the process of obtaining up to date and accurate medication list that has been compared to the most recently available information and has documented any discrepancies, changes, deletions or additions, resulting in a complete list of medications accurately communicated.
13.2.2 The person in-charge of coordinating the discharge is also responsible for ensuring the list of medication on the discharge letter is legible, accurate and complete. This can be done more easily and effectively if medicines reconciliation has been carried out, soon after admission by a pharmacist, doctor, experienced pharmacy technician or suitably
Discharge and Home of Choice Policy September 2010
44 of 114
trained nurse. A full medicines reconciliation will document and explain:
When a medicine has been stopped, and for what reason
[including topical preparations]
When a medicine has been started and for what reason
The intended duration of a treatment [e.g. antibiotics or hypnotics]
When a dose has been changed, and for what reason
When the route of the medicine has been changed, and for what reason [this is particularly important, when the route or administration has changed from parenteral, often intravenous, to oral]
13.2.3 For further information on medicines reconciliation refer to the hospitals medicines management policy and “Medicines
Reconciliation, A Guide to Implementation” www.npci.org.uk/medicines_management/safety/reconcil/library/guide
_reconciliation.pcp
And “Technical patient safety solutions for medicines reconciliation on admission of adults to hospital” www.nice.org.uk/nicemedia/pdf/PSG001GuidanceWord.doc
13.4 Medicines Adherence
13.4.1 It is the person coordinating the discharge responsibility to make certain that the patient [or their carer, where appropriate] will be able to use their medicines as prescribed either by assessing them themselves or checking that an assessment has been carried out and documented within 72 hours of discharge.
This will include but should not be limited to:
What the medicine is, how to use it and likely benefits
Likely adverse effects and what to do if they thing they are experiencing them
What to do if they miss a dose
Whether another prescription is needed and how to get further supplies
13.4.2 It is the person coordinating the discharge responsibility to ensure that:
the patient has all relevant information in the format and content that meets their individual needs.
And any individual issues or concerns have been addressed by the most appropriate person, before the patient is discharged.
Link with services to check where relevant, that Domiciliary Care
Workers can manage the patient’s medicines
13.4.3 NICE has published guidelines on interventions to increase adherence.
These include:
Finding out if non-adherence is because of beliefs and concerns
[intentional non-adherence] or practical problems [unintentional non-adherence]
Identifying solutions to practical problems
Suggesting patients record their medicine-taking
Encouraging patients to monitor their condition
Discharge and Home of Choice Policy September 2010
45 of 114
Simplifying the dosing regimen
Using alternative packaging
Using a multi-compartment medicines system
Determining if side effects are a problem
Discuss benefits, side effects and long-term effects and how the patient would like to deal with side effects
Consider adjusting the dosage, switching to another medicine, and other strategies such as changing the timing of medicines
Asking if prescription costs are a problem and consider options for reducing costs.
13.4.4 Further information can be found in, “Medicine Adherence, Involving
Patients and supporting adherence” http://www.nice.org.uk/nicemedia/pdf/CG%2076%20Medicines%20ad herence%20QRG%20FINAL.PDF
13.5 Process – ordering Take Home Medications
Medications should be re-ordered / restocked 72 hours before planned discharges
13.5.1
One-stop dispensing – medication will already be labelled for discharge, as it has been provided as a patient pack and kept in a locked cabinet by the patient’s bedside. The supply will be regularly topped up by the Pharmacist Technician. Checks on discharge include:
Supplies – the patient should have at least 14 days supply to go home with
Whether the patient is “self-medicating” and checking adherence with medicines, as described above
13.5.2
Patients’ Own Drugs
- where patients’ own drugs [PODs] have been brought in and been assessed on admission, usually by pharmacy staff, and found to be of satisfactory quality, they may be used during the inpatient stay and on discharge. Checks on discharge include:
1. Obtaining permission from the patient to destroy any medicines no longer in use
Supplies
– the patient should have at least
14 days supply to go home with
Whether the patient is “self-medicating” and checking adherence with medicines, as described above
13.5.3
Monitored Dose Medication / “Blister” Packs
A list of medications should be faxed to the Patient’s GP, who will request the community pharmacist to dispense the medication in a monitored dose system or “blister” pack. This may be collected by the patient’s family or carer, to be available on discharge.
Adherence should still be checked and documented, as described above, before discharge.
13.5.4
Discharge – less than 72 hours / out of hours
Discharge prescriptions ordered from the Pharmacy, Monday
– Friday,
9 – 5 pm will take 24 hours before they are ready to collect. See policy for obtaining medications from pharmacy out of hours. Patients should have a minimum of 14 days supply of medication on
Discharge and Home of Choice Policy September 2010
46 of 114
discharge. Adherence with medication should always be checked before discharge.
13.6 Process - ordering Take Home Dressings and Appliances
Dressings and appliances should be ordered 72 hours before planned discharges. A minimum of 7 days supply of dressings and appliances should be sent with the patient on discharge / transfer.
Discharge and Home of Choice Policy September 2010
47 of 114
14. Responsibilities relating to the supply of Intermittent
Home Oxygen
14.1 Home oxygen is supplied in compliance with national guidelines. [Clinical
Component for the Home Oxygen Service in England and Wales, British
Thoracic Society, January 2006] http://www.britthoracic.org.uk/Portals/0/Clinical%20Information/Home%20Oxygen%20Servic e/clinical%20adultoxygenjan06.pdf
14.2 In most circumstances involvement with a Respiratory Nurse Specialist [RNS] prior to discharge is advisable to ensure guidelines are followed and appropriate follow up arranged.
14.3 The Clinical Team, with help from the RNS if appropriate, are responsible for the completion of the Home Oxygen Order Form [HOOF], the Home Oxygen
Consent Form [HOCF] and the Home Oxygen Record Form [HORF].
14.4 The HOOF form is faxed to the home oxygen supplier [Air Products] at the latest by 5 pm the day before discharge is planned. Copies of the HOOF form are sent to the patients GP, PCT and RNS. In exceptional circumstances home oxygen can be requested in an emergency. In this situation four hours notice is required .
14.4 A member of the clinical team discharging the patient must confirm that the home oxygen is in place before the patient is discharged.
14.5 A member of the clinical team discharging the patient must ensure the patient
/ carer understands and can manage 02 therapy as required.
Discharge and Home of Choice Policy September 2010
48 of 114
15. Responsibilities Relating to Infection Control
Infection Control risks must be identified with any patient discharge and plans instigated to deal with these in compliance with the Infection Control Policy,
Healthcare Act and Hygiene Code. There will be liaison with the Infection
Control Nurse on identification of risk. Any infection control risks must be shared with those delivering care following discharge. A member of the clinical team ensures the patient /carer understands and can manage infection control as required.
Discharge and Home of Choice Policy September 2010
49 of 114
SECTION 6 – Responsibilities for Patients with Added Needs
16. Additional responsibilities relating to – learning disability, mental health or dementia
16.1 Extra time is needed both for care and communication. It is well recognised that some people with learning disability, mental health problems or dementia are anxious about receiving medical treatment. For this reason, preparation is essential to eliminate any fears and minimise concern. Engage with members of the specialist learning disability, substance misuse and mental health teams for assistance / advice early on where:
Communication challenges make it difficult to assess whether the patient is able to provide consent and/or understand the processes he or she is to undergo
Vital information on health, social care, family carers or housing services to plan discharge is missing
Expert input is required for a more detailed assessment or rehabilitation
Anxieties which the patient may have can be alleviated with input from the specialist team
The activity of daily living assessments done in hospital are not a true reflection and picture of what the individual’s abilities are in their familiar home environments
A person with learning disabilities lives independently and additional support may be required on discharge from the community team for learning disabilities.
16.2 Carers’ needs should be assessed as part of the planning for discharge. As the demands on carers, when the patient has severe and / or enduring mental health problems or dementia can lead to unrealistic or inappropriate discharge planning if not considered. This needs to be done early on, to avoid unnecessary delay in discharge. For further information, see: Practitioners
Guide to Carers Assessment under the Carers’ and Disabled Children Act,
2000, OR DH Carers at http://www.dh.gov.uk/en/SocialCare/Carers/index.htm
OR Carers UK at www.carersonline.org.uk
16.3 Learning Disabilities
16.3.1 Since 2005, every person with a learning disability who wants a health action plan [HAP] will have one. A HAP will cover day-to-day issues such as diet, exercise, medicines, going to the dentist and the optician etc, and the contact details for parents [where appropriate], family carer or residential Carer. Information for discharge may be added to this document. If the person does not already have a HAP, this would be a good time to start one. Good practice guidance on HAP’s is at website: www.doh.gov.uk/learningdisabilities
16.3.2. A hospital book may be available for people with learning disabilities.
This includes pictures that can be used to explain events in the hospital and going home. It is recommended that a copy of this book is kept by the person with a learning disability or if the patient has given consent,
Discharge and Home of Choice Policy September 2010
50 of 114
it may be kept with the patient’s records for easy access by the multidisciplinary team.
16.4 Books beyond Word is a series of books which are very useful for people who can’t read or do not speak English. The series is published by the
Royal College of Psychiatrists, Booksales, 17 Belgrave Square, London,
SW1X 8PG Tel. 0207 235 2351
Discharge and Home of Choice Policy September 2010
51 of 114
17. Additional Responsibilities for Maternity Services
17.1 The length of stay in the Maternity Unit is flexible and determined by the mother’s medical and obstetric needs.
17.1.1 The Midwife will liaise with the mother and other relevant members of the multi-disciplinary team regarding the discharge. This may include
Health Visitors and District Nurses.
17.1.2 The midwife will ensure that any discharge medications required are given to the client prior to discharge.
17.1.3 It is expected that the client will arrange their own transport home, ensuring the safety of the baby as appropriate.
17.2 Antenatal Discharge
17.2.1 The Midwife will ensure that the patient held record and medical records are fully completed in accordance with Trust and Professional documentation standards.
17.2.2 The Midwife will ensure that all investigations required have been carried out and recorded in the medical records.
17.2.3 The midwife will notify the community midwife of discharge.
17.2.4 Follow up ante-natal clinic appointments will be discussed with the client prior to discharge.
17.3 Postnatal Discharge
17.3.1 The midwife will ensure postnatal records and transfer letters are fully completed.
17.3.2 The midwife will ensure any investigations have been completed, recorded and followed up prior to or following discharge as necessary.
17.3.3 The midwife will ensure that the mother is aware of all follow-up arrangements and emergency contact numbers.
17.3.4 The midwife will inform the Community Midwife of the discharge.
17.3.5 The midwife will be responsible for ensuring that discharge letters are completed and sent to the General Practitioner within 24 hours of the patient’s discharge.
17.3.6 Where the mother and/or baby require intervention from other members of the Primary Health Care Team or other health/social care professionals, arrangements for this follow up will be made by the
Midwife in liaison with the Community Midwife and General
Practitioner.
Discharge and Home of Choice Policy September 2010
52 of 114
17.3.7 In the event of maternal death, foetal loss or transfer to a specialist unit, the mother’s General Practitioner, Community Midwife and Senior
Midwife will be informed as soon as possible. In the event of maternal death the on-call supervisor of midwives will also be informed.
Discharge and Home of Choice Policy September 2010
53 of 114
18. Additional Responsibilities for Paediatric Servi
ces
18.1 The planning of a child’s discharge will begin on admission by the Paediatric
Team. Information obtained during the initial nursing interview will be used to begin the planning process. It will be established whether hospital transport will be required and the named nurse will make the appropriate transport arrangements. [See 18.12 for example of discharge checklist].
18.2 Discharge advice/information will be given to the child and the family/carer by the named nurse. Advice may be given verbally and supported by easy to understand written information.
18.3 A registered sick children’s nurse or doctor should complete the initial discharge letter, a copy of which will be given to the family at the time of discharge , as per guidance in 4.8 and a copy retained in the patient record.
18.4 A discharge summary will be sent by the Consultant Paediatrician/Specialist to the GP within 24 hours of the discharge as per guidance in 4.10 and standards listed in Appendix 5.
18.5 All children and their family/carer will be given a hotline contact number, which they can access for up to 48 hours following discharge . This enables parents/carers to directly re-access the paediatric service if they are concerned about their child in the early post discharge phase. On occasions the child may be readmitted to the Children’s Ward.
18.6 A health visitor form [See example 18.13] will be completed both on admission and discharge, where applicable, to ensure the child’s health visitor/school nurse is fully aware of the admission. The health visitor will be contacted directly where there are concerns about a child. This may include accidental injury, faltering growth syndrome or Child Protection issues.
18.7 Any concerns regarding Child Protection will have already been referred to the appropriate Child Protection Officer. In cases involving an emergency protection order complex multi-agency planning will be required to determine discharge plans. For additional information on “Safeguarding Children” see policy CPCT/001/037 or refer to Cumbria Local Safeguarding Children Board
(LSCB) website at: www.cumbrialscb.com
18.8 Children will be referred to the paediatric nursing team, if it is considered necessary, prior to discharge home. Children with complex care needs will require a full multi-agency discharge plan. Agencies involved may include community children’s nursing team, physiotherapy, occupational therapy, dietician, GP, education, social services and respite carers.
18.9 Children with life limiting illnesses or chronic diseases are given open access to the children’s ward. This enables parents/carers to contact the ward directly for a determined period of time without having to access the paediatric service through their GP or accident & emergency department.
18.10 If required, children will be issued with medication from the hospital pharmacy on discharge. If this is not possible they will be given a prescription for a community pharmacy. Some medication can be dispensed directly from the ward in accordance with hospital policy.
Discharge and Home of Choice Policy September 2010
54 of 114
18.11 Parents will receive details of out-patient follow up appointments either prior to discharge or by appointment letter. Some children will be seen as ward attenders and this will be arranged with the ward clerk or ward attender’s nurse.
Discharge and Home of Choice Policy September 2010
55 of 114
18.12
EXAMPLE: PAEDIATRIC DISCHARGE CHECKLIST
Discharge Date:
Discharge Diagnosis:
Time:
Discharge authorised by:
Written information given to parent/carer
Verbal information given to parent/carer
Understanding of information given checked
Discharge letter given to parent/carer
Take home medication supplied
Yes No N/A Comment
State which info given:
State which info given:
Understanding of medication checked
Follow-up appointment required
Appointment made or Request form completed
[delete as appropriate]
Discharge letter sent to GP
Health Visitor liaison sheet completed
Social Worker informed of discharge
Community Nurse informed of discharge
Name of Social Worker:
Name of Community Nurse:
Referred to other Health
Professional
Open Access Arranged
State: e.g. Dietician / Fairfield Centre
State: duration
Cannula / Butterfly removed
Parent held record available
Parent Record completed
Checklist completed by: NAME:
SIGNATURE:
18.13 Example: Referral
Discharge and Home of Choice Policy September 2010
56 of 114
Health Visitor / School Nurse - Notification of discharge from Children’s Ward
Hospital Label: Name and Contact
GP:
Consultant:
Health Visitor:
School Attended:
Date of Admission:
Reason for Admission:
Does the Health Visitor / School Nurse need to contact ward?
Discharge Date:
YES NO
Medication [frequency, route, dosage]:
Discharge Diagnosis:
Follow-up:
Children’s Community Nurse Informed?
Relevant Information:
Signature of Discharge Nurse:
YES NO
Copy to HV on admission, Second copy to HV on discharge
For 5-16 years olds - Copy to School Nurse
Third copy Hospital Notes
19. Additional Responsibilities for Palliative Care
19.1 Where a patient is in a hospital setting the named nurse for the patient remains accountable for co-ordinating discharge arrangements.
19.2 The Palliative Care Team can be accessed to provide specialist advice and assessment of both patients and families and where appropriate to facilitate
Discharge and Home of Choice Policy September 2010
57 of 114
access to services including specialist services in the community.
Involvement of the Palliative Care team must be documented in the patient records.
19.3 Due to the progressive nature of the illness in palliative care it is of paramount importance that the patients and families wishes regarding future care are assessed upon admission and throughout the period of the in-patient stay.
Where possible a Preferred Priorities of Care form [PPC] should be completed and retained by the patient.
19.4 It is essential that discharge planning is commenced as early as possible to address any potential barriers or complex needs. This may require early referral to a wide range of social, medical, nursing or AHP’s as appropriate.
Verbal and written communications with the primary health and social care team is essential to contribute to the assessment of any discharge issues and to ensure that a patient with palliative care needs will be discharged from an acute setting expediently. If Social Services are involved with a rapid discharge [to die at home] NHS Continuing Care fast track should be completed. Other palliative discharges were Social Services are involved require Continuing Care Screening to be completed.
19.5
Plan ahead for any potential problems that may occur due to disease progression. Medication for use if required can then be provided and future action discussed with patient and family to minimise future crisis. Where possible a patient held medication chart should be provided.
19.6 Good communication is key in planning discharge and informing families and relevant professionals on discharge eg. GP, District Nurse, Social Services and Cumbria Health On Call [CHOC]. If patients are being discharged for end of life care anticipatory prescribing should be undertaken a Special Patient
CHOC form completed and faxed to CHOC office.
19.7 A rapid discharge of a patient close to end of life who wishes to die at home and not in hospital is an emergency situation. Time is of essence. Please contact the Palliative Care Team as soon as possible for help and advice.
Discharge and Home of Choice Policy September 2010
58 of 114
20. Additional responsibilities for Homeless Persons or
Persons with Housing Issues
20.1 For those persons who declare at admission that they are of “no fixed abode” or those with significant housing issues, special plans must be made.
With the permission of the patient, Staff should contact the local housing office in their area for advice or refer issues as soon as actual or potential needs are identified
Allerdale Borough Council 01900 702660
[out of hours] 01900 871080
Barrow Borough Council
[out of hours]
[email]
01229 876332 or 01229 876489
01229 833311 housing@barrow.gov.uk
Carlisle City Council
[out of hours]
01228 817499
01228 511061
Copeland Borough Council 08450548600
[out of hours] 01946 815500
[email] housing.options@copeland.gov.uk
Eden District Council
[out of hours]
South Lakeland District
01768 861400
0800 3581401
Council
[out of hours - Kendal
& East]
[out of hours - Lakes,
01539 733333
0870 4286905
Ulverston & West] 0870 4286906
The Housing Officer will make arrangements with staff to meet with the patient
[and family and carers, where appropriate] to undertake an initial assessment.
The Housing Officer should be provided with a named contact from the multidisciplinary team to coordinate discharge plans.
The Housing Officer may arrange a case conference, and should be invited to attend case conferences as appropriate.
Discharge and Home of Choice Policy September 2010
59 of 114
21. Additional Responsibilities for Transfer of Prisoners
21.1 It is important to maintain an appropriate balance between the demands of patient care and custody. Prison discipline staff will be present at all times with prisoners to ensure they behave and do not escape.
21.2 Prisoners will be constantly supervised by prison staff [referred to as
“bedwatches”.
21.2.1 Cutting delays in the patient journey through hospital is a priority for both NHS trusts and the Prison service. Prisoners represent a patient group where there are clear advantages to all concerned in working through the partnership process to cut delays.
21.2.2 To reduce delay in discharge:
1. All prisoners should have a treatment plan within 24 hours of arrival in the hospital
2. An expected date of discharge should be set within 24 hours of arrival or in many cases before admission for elective procedures and communicated to the prisoner and the prison discipline staff who accompany the prisoner.
3. The date of discharge should be proactively managed against the treatment plan
4. Where a multidisciplinary case conference is required, a representative from the HMP Haverigg Healthcare Team should be included
21.3 Continuity of Care
21.3.1 HMP Haverigg is able to offer the same level of care as a normal general practice.
21.3.2 It is the responsibility of the hospital to send with the prison discipline staff required information to ensure standards of continuity of care.
This includes a clinical summary and medication, appropriate to clinical need, to ensure supply until a GP prescription can be obtained, and outpatient appointments where required. Complex needs should be communicated directly with the healthcare team at HMP Haverigg in advance of transfer. The contact number for Prison Healthcare is
01229 713038 [office hours].
21.3.3 There is no restriction on time of day or night which prisoners may be transferred, as their bed at the prison is kept.
21.3.4
“The Continuity of Healthcare for Prisoners” Prison Service Order
3050, 10/02/2006 should be used in conjunction with this policy.
Discharge and Home of Choice Policy September 2010
60 of 114
22. Additional Responsibilities for Carers
It is the responsibility of the multi-disciplinary team to ensure the actions taken throughout the discharge pathway reflect an understanding of the impact on carers and the need for better overall outcomes for carers and the cared for person.
Carers from minority ethnic groups, carers of people with dementia and “young carers” have specific issues which need to be addressed.
22.1 UK Carers have put together a guide for carers on what to expect when a patient is coming out of hospital. It can be found at: http://www.carersuk.org/Professionals/Orderpublications/Factsheetsbook lets#1014
22.2 For assistance from the Carers Association contact:
South Lakeland Carers
– 01539 815970
Furness Carers
– 01229 822822
Eden Carers – 01768 890280
West Cumbria Carers – 01900 810101
Carlisle Carers
– 01228 542156
Refer also to the UK Carers Checklist (2003) as good practice on the following page:
Discharge and Home of Choice Policy September 2010
61 of 114
Discharge and Home of Choice Policy September 2010
62 of 114
SECTION 7 – Refusal of Treatment / Self-Discharge
23. Additional Responsibilities where Patients Self
Discharge
23.1 There are occasions when patients will be determined to leave hospital against medical advice
23.1.2 Every effort must be made by members of the multi-disciplinary team to persuade the patient to continue with their treatment.
A senior practitioner will have discussed and explained all the risks of premature discharge to the patient. When this fails, certain action MUST be taken protect the patient as much as possible. The patient should be asked to sign the Refusal of
Medical Intervention form [see 22.5
] .
Should the patient refuse to sign the form, this must be documented in the nursing records and counter-signed by another member of staff.
23.2 Is the responsibility of the Medical Staff to document all information in the patie nt’s medical record.
23.3 The following action must be taken by the ward team in all instances where patients are discharging themselves:
23.3.1 Inform the patient GP and/or other primary health care professional as required, as a matter of urgency.
23.
3.2 Where appropriate contact the patient’s Next of Kin
23.3.3 Where appropriate for patient and/or public safety inform the police.
23.3.4 Where a patient is known to Adult Social Care the social worker should be informed.
23.3.5 Inform the relevant Senior Nurse in the Directorate
23.3.6 Inform the Discharge Liaison / Coordinator if relevant.
23.3.7 Arrange appropriate transport if necessary
23.3.8 An entry must be made in the patient record and a copy or the refusal of medical intervention form be filed in the patient record.
23.4 Patients who refuse to return to hospital following a home assessment, period of leave, or those who leave the ward and fail to return, will be considered as taking their own discharge.
23.4.1 Staff escorting patients for home assessments should carry a refusal to medical intervention form with them.
Discharge and Home of Choice Policy September 2010
63 of 114
23.5 REFUSAL OF TREATMENT
Patient Details:
______________________________________________________________ of ____________________________________________________________ hereby declare that I am leaving the hospital by my own choice and contrary to medical advice.
I have had the risks of doing so explained to me and I accept the full responsibility for my action.
Date ________________________________
Signature ________________________________
In the presence of:
Signature ________________________________
Name of Witness
_____________________________________________(please print)
Address ______________________________________________
________________________________________________
________________________________________________
Signature __________________________________________
Name of Witness
_____________________________________________(please print)
Address ____________________________________________
______________________________________________
_____________________________________________
Comments:
Discharge and Home of Choice Policy September 2010
64 of 114
SECTION 8 - “Home of Choice” - additional guidance
24. Patient Group
This guidance applies to all adult patients over 18 years irrespective of diagnosis and in any NHS hospital setting.
Home of Choice applies to patients who meet any of the following criteria:
The agreed assessment shows that the patient can be discharged from hospital, needs a placement in a nursing home or residential care home and this placement will be funded by either the patient, Adult
Social Care or the NHS or a combination of the above.
The patient has identified a preferred home, or is having difficulty in identifying one.
The patient is unwilling to be discharged until a placement in the chosen home is available.
An interim or alternative long term placement exists which meets with the patient’s assessed needs.
The patient is from within or outside the Cumbria’s catchment area. In the case of patients who usually reside outside the Cumbria area before coming into hospital, the Adult Social Care Directorate covering their area of residence will be responsible but may invite Cumbria Adult
Social Care Directorate to assist with arrangements on their behalf.
24.1 Following a multi-professional assessment the multidisciplinary team* will indicate when care in a nursing or residential home is the most appropriate place for the patient. As part of this process the patient and their carers should play an active role in choosing a suitable and available home of their Choice. [*The multi-disciplinary team would normally consist of the Consultant or Medical Representative, Nurse, any Allied Health Professional, Social Worker and if appropriate,
Mental Health Nurse].
24.1.2 The decision to live in a nursing home or residential care home is a major one and it will be necessary to weigh up factors such as the proximity of relatives, the quality and cost of accommodation and the quality of life which the patient will experience. The decision should involve a good deal of thought, and once a home has been chosen, people may have to consider the process they should follow until a vacancy becomes available in the home of their Choice.
24.1.3 It is important to recognise that it is not always appropriate or in the best interest of the patient to remain in a hospital bed until such time as a bed in a particular home becomes available. This guidance seeks to deal with these situations. It should be noted that whilst the Choice
Directive guidance is referring primarily to hospital beds that no one has the right to occupy a bed in any care setting if hospital-based treatment is no longer required. The spirit and application of this guidance will therefore need to be considered for other settings. This
Discharge and Home of Choice Policy September 2010
65 of 114
will have to be balanced by the fact that transitional care has been developed to enable further rehabilitation and support on discharge.
This step in the care pathway also needs to be explicit.
24.1.4 The National Health Service is under great pressure to only use hospital beds for those who need specific hospital services due to their physical or mental illness. If beds are occupied by people waiting for arrangements outside the hospital to be made, including waiting for a place in a chosen home to become available, this effectively denies access to these hospital beds for people who need them.
24.1.5 Those responsible for arranging discharge care for patients, (social workers,doctors, nurses, therapists, case managers/co-ordinators), have the difficult task of finding the right balance between these , often competing, pressures.
24.1.6 If patients lack mental health capacity it will be necessary to have a clearly identified advocate, relative or guardian to ensure appropriate decision making at all stages. This should follow current policy and good practice in mental health. It is essential that a worker with this knowledge advises.
24.2 National guidance In guidance LAC (2004)20 “National Assistance
(Residential Accommodation) (Additional Payments and Assessment of
Resources) (Amendment) (England) Regulations 2001 states that where a persons care needs can be met in a residential or nursing care home “Waiting for the preferred care home should not mean that the person’s care needs are not met in the interim or that they wait in a setting unsuitable for their care needs, and this includes an acute hospital bed, until the most suitable or preferred accommodation becomes available. These arrangements should meet the needs of the individual and sustain or improve their level of independence.”
The guidance goes on to say:
“In all but a very small number of cases where an individual is being placed under Part 2 of the Mental Health Act 1983, individuals have the right to refuse to enter a care home. This includes patients awaiting discharge from hospital. In such cases the social services department should work with the person, his or her family and carers, and NHS partners, (and potentially housing partners), to explore alternative o ptions, including a package of health and social care in the person’s own home or suitable alternative accommodation”
A charge may be payable by the person to the Adult Social Care and
Cultural Directorate for the social care element of the package. Costs can vary according to the type of care provided. One of the conditions associated with the provision of preferred accommodation is that such accommodation should not require the council to pay more than they would normally expect to pay, having regard to assessed needs (the
‘usual cost’). In setting and reviewing their usual costs, councils should
Discharge and Home of Choice Policy September 2010
66 of 114
also have due regard to Best Value requirements under the Local
Government Act 1999.
The Community Care (Delayed Discharges) Act 2003 introduced a financial incentive for local authorities to provide any community care services or carer’s services that are needed for the patient’s safe transfer to a more appropriate setting. The first part of the Act set out the mechanisms that the NHS and Social Services were required to have in place by October 2003 and introduced charging requirements in January
2004. Further guidance set out in a Local Authority Circular and DOH letter in October 2004 provides further clarity with regards to fees in relation to Choice of accommodation.
This patient Choice policy will be reviewed regularly in the light of changing guidance.
24.3 Underlying Principles
All patients are treated fairly and without discrimination.
Patients should be fully involved from the beginning in the discharge planning process which should be initiated when the patient is admitted to hospital and a proactive approach is taken to ensure the discharge is appropriate, safe and timely. This is in line with Hospital Discharge and
Transfer Policy, good practice and the National Service Framework for
Older People, if appropriate.
The patient will continue to receive an appropriate standard of care during the process of choosing a home of Choice.
The patient, where practicable, should agree with the discharge destination.
The multi-professional team will always seek the permission of the patient to allow full involvement of relatives/carers/ advocate in the discharge planning process. Where patients are unable, for whatever reason, to speak for themselves or present their own views, the wishes and views of the relatives/carers/advocate will be obtained, ensuring wherever possible that their interests or wishes do not conflict with those of the patient, underpinned by the Mental Capacity Act 2007.
The application of this Choice Policy does not affect the right of the patient to challenge any other care or care process. For example, if there is a view expressed that the NHS Continuing Care eligibility has not been applied correctly, this does not affect the right of the patient to challenge this. The process outlined in the NHS Continuing Care
Guidance should be followed.
Formal discussions with the patient and records of all decisions will be recorded in the patient’s discharge planning documentation and signed and dated.
Discharge and Home of Choice Policy September 2010
67 of 114
At all times, Health and Adult Social Care staff should act in the best interest of the patient. Whilst it is not in the patient’s best interest to remain in a hospital bed longer than is necessary, it is in the interest of other patients who require the service that beds are made available in a timely manner.
Where a patient is discharged to an interim placement, the allocated
Social Worker/Care Manager (Social Care & Cultural Directorate) will maintain contact with the patient and will ensure that, when a place becomes available in the patient’s Choice home and where funding permits, arrangements will be made to transfer the patient to that home if that is still their wish.
24.5 Process to apply for Patients Waiting in Hospital for a Nursing
Home or Residential Care Home (SEE flowchart 24.8)
24.5.1 This guidance will be followed where the multi-professional assessment of the patient indicates that the patient is medically fit for discharge, and they would not benefit from further inpatient care. The full MDT should be satisfied that the patient’s condition cannot be further improved by in-patient rehabilitation or Intermediate care, and placement in a Nursing Home or Residential Care Home is the most appropriate option to meet the patient’s assessed needs.
24.5.2 In some instances patients can move on to an interim care setting to have their needs further assessed and/or receive further treatment from the multi-professional team. The use of interim or transitional care is consistent with the Choice of Accommodation Directive as long as the interim placement meets the needs of the individual; it is acceptable for the person to move from an acute setting to an interim placement until a permanent/alternative Choice becomes available.
24.5.3 A key component of the assessment process will be the involvement of the patient at all stages. Patient also includes advocate, where required, by the Mental Capacity Act.
24.5.4A discharge/case coordinator will be identified from the hospital to be responsible for ensuring that appropriate discussions take place with the patient at all stages of the assessment and care planning process.
All such discussions will be recorded in the patients discharge planning documentation. For some patients a social worker may already be involved and some may need to have one identified early in the hospital stay/discharge process. This may be a particular issue for those patients with mental health needs where there may be more complex issues. The discharge and transfer policy gives further guidance and emphasises the need for starting discharge on admission to hospital.
24.5.5On completion of the assessment, the Discharge/Case Coordinator should inform the patient, the family, the carer that the assessments have been completed and confirm that:
Discharge and Home of Choice Policy September 2010
68 of 114
They are ready for discharge from Hospital.
Discharge to a Nursing Home or Residential Care Home will be necessary.
It is expected that they should find a suitable home within 7 days from the date of the MDT decision that a nursing and residential home was the most appropriate place for the patient. The support of Adult Social
Care should be made available if necessary (not all those choosing a home want or need this support)
The name of the person who will be responsible for assisting them in the process.
An information leaflet on Home of Choice which outlines help needed when moving from hospital in to residential or nursing home care has been issued. This leaflet should include details of the discharge process and timescales involved in choosing a care home.
It may be necessary for the patient to consider alternative Nursing
Homes or Residential Care Homes where a vacancy exists until the home of the Choice becomes available.
24.5.6Where the decision has been made for the patient to go into Nursing or
Residential Care, the discharge / case coordinator will ensure that the patient has all the relevant information to enable them to choose an appropriate home. This may include details of the patient’s care needs; financial limits appropriate to meet such needs, lists of homes likely to meet such needs and details of homes with current vacancies.
24.6 Guidance to be followed in the event that a patient has yet to identify a suitable vacancy, after following completion of assessment
In the event that the patient has not identified an appropriate placement within agreed timescales, the discharge/case coordinator should first ensure that all necessary information and support have been given to achieve this.
When the Multi-disciplinary Team [MDT] are assured of the reasons the key principles have not been met;
the patient’s eligibility for Continuing Care has not altered,
the patient or relatives/carer/advocate have not been forthcoming in relation to identifying a suitable vacancy,
consequently the patient refuses to leave the hospital unless a place in the Nursing Home or Residential Care Home of their choice is available,
The following guidance should be followed .
24.6.1 The discharge/case coordinator should arrange a meeting (Review meeting) with the patient and/or family, MDT member and Social
Worker/Care Coordinator within 3 working days . This meeting should
Discharge and Home of Choice Policy September 2010
69 of 114
be chaired by the relevant hospital manager. This should be documented in the discharge pathway.
24.6.2At the review meeting with the family and/or carers, it should be confirmed that the patient no longer requires an NHS bed and that they should make alternative arrangements and the following points should be established.
The patient is fit for discharge.
It is inappropriate for the patient to remain in hospital, as this may be detrimental to the patient’s health and well being.
There is a defined time period within which a suitable Nursing
Home or Residential Care Home placement should be found.
The period of time normally expected for a patient to choose their accommodation is within 7 days and commences from the point at which their discharge / care coordinator informs the patient of the need for a Nursing Home or Residential Care Home
Placement and provides written information to support the process.
The nursing or residential home will want to carry out their own assessment of the persons needs before offering a place. The time scales outlined will need a proactive approach from all concerned to ensure this happens particularly if more than one option is being considered.
24.6.3 The relevant Hospital Manager with responsibility for leading the meeting should:
Ensure that all the information and support is available to enable an appropriate placement to be made.
Confirm with the Social Worker/care coordinator that an appropriate and reasonable placement is available.
Explain to the patient that a further time period , up to a maximum of 7 days from the date of the meeting, is available in which to find an appropriate (local) placement.
Explain, if an appropriate placement is not available and Adult
Social Care has funding responsibility for the patient, then the reimbursement process should begin.
24.6.4 Adult Social Care should give individuals an indication of the likely duration of the interim arrangement. Providers should place the individual on the waiting list for the preferred accommodation and aim to move them into that accommodation as soon as possible.
Information about how the waiting list is handled should be clear and agreement should be made with the individual about how they would like to be kept informed of progress. If the duration of the interim arrangement exceeds a reasonable time period e.g. 12 weeks, the individual should be reassessed to ensure that the interim and
Discharge and Home of Choice Policy September 2010
70 of 114
preferred accommodation, are still able to meet the individual’s assessed needs and to prevent any unnecessary moves between care homes that are unable to meet the individual’s assessed needs. As part of this reassessment, individuals should also be asked if their preference is now to remain in the interim accommodation or whether they wish to continue waiting for their original preferred accommodation.
24.6.5 If an individual continues to unreasonably refuse the interim care home
Adult Social Care is entitled to consider that it has fulfilled its statutory duty to assess and offer services, and may then inform the individual, in writing, they will need to make their own arrangements. This position also applies to the unreasonable refusal of a permanent care home, not just the interim care home. In such circumstances Reimbursement does not apply. If at a later date further contact is made with social services regarding the individual, they should then re-open the personcentered planning process, if it i s satisfied that the individual’s needs remain such to justify the provision of services and there is no longer reason to think that the individual will persist in refusing such services unreasonably. Adult Social Care should refer to Annex A of LAC
(2003)21
– The Community Care (Delayed Discharges etc) Act 2003
Guidance for Implementation. Councils may wish to take their own legal advice in such circumstances.
24.7 Guidance to be followed in the event that a patient has not identified a suitable placement, with a vacancy, within 7 days of the Review meeting.
24.7.1 If, after the extended time period, the patient has still not been discharged from hospital and there is no indication from the patient/family that discharge is imminent, the discharge / case coordinator should inform the responsible Clinician and Ward Sister, Adult Social Services
Team Manager and Hospital General Manager or Clinical Services
Manager (Mental Health).
24.7.2 As this situation is now escalating a Senior Hospital General
Manager/Clinical Services Manager should convene and chair a meeting (Final Review meeting) within two days inviting the patient/family to attend in order to finalise the discharge plans. This should be confirmed in writing. If an individual continues to unreasonably refuse the interim care home, adult social care is entitled to consider that it has fulfilled its statutory duty to assess and offer services, and may then inform the individual, in writing, they will need to make their own arrangements.
24.7.3 If, at this final review meeting, it becomes apparent that the patient
/ family/ carer does not intend to find a placement immediately, the
Senior Hospital Manager should advise the patient that the Trust may instigate legal proceedings to ensure that the patient is discharged from
Discharge and Home of Choice Policy September 2010
71 of 114
hospital so as to safeguard the health and well being of other patients by making the bed available.
24.7.4 The details of this meeting must be confirmed in writing, with a copy being sent to all present at the meeting and t he patient’s or relevant family/carer, and documented in the Discharge Documentation.
24.7.5 A planning meeting should be convened to ensure risk issues have been considered with the following personnel:
Hospital Trust Directorate Manager
Adult Social Care, Area Manager
Hospital Trust Executive Director / Representative
Hospital Trust Legal Services Officer
Primary Care Trust manager
24.7.6 This stage of proceedings is likely to be declared as a dispute and be dealt with under the hospitals usual disputes policy and legal advice sought accordingly.
24.7.8 The patient and /or relative would maintain the right to use the relevant complaints procedure at any stage.
Discharge and Home of Choice Policy September 2010
72 of 114
24.8 Process To Apply For Patients Waiting In Hospital For A Nursing
Or Residential Care Home (Discharge Policy)
Multidisciplinary Team decide patient ready for discharge . E.g. reimbursement definition
(Point)
Inform patient/ family/ carer of expectation to find an appropriate placement within 7 days
(Point)
No identified suitable vacancy – Discharge /
Case Coordinator to convene Review meeting within 3 working days
(Point)
Review Meeting should clarify options indicating a further time period of up to a maximum of 7 days from the meeting date to find an appropriate placement.(Point
Still no vacancy identified or placement agreed within a further 7 days of Review Meeting.
(Point
Final review Meeting to take place within 2 days Patient informed Trust may instigate legal action to discharge.
(Point)
PATIENT DISCHARGED
DISCHARGED
Interim arrangement (12 weeks)
Continuing Care needs assessment
Inform : Responsible Clincian,
Ward Sister, Hospital General
Manager or Clinical Services
Manager (Mental Health), Adult
Social Care Team Manager
( Point )
Planning meeting to consider risks:
Manager, Hospital Social Services
Team Manager, Executive
Director, Legal Services Officer
(Point )
Permanent Placement
Discharge and Home of Choice Policy September 2010
73 of 114
24.9. Guidance Notes Agreed By Partners Which Apply To Home Of
Choice
24.9.1 Human Rights
No one has the right to remain in a hospital bed if they do not require hospital care or further assessment, with the exception of patients who are in receipt of palliation and are likely to die in the near future.
24.9.2 Advocacy
Patients have the right to involve an ‘advocate’ at any stage of their care in hospital or discharge. Staff can direct patients to appropriate bodies who provide advocacy services and or offer support with decision making about their care. Paid advocacy may be available in some circumstances in accordance with the hospital trust or adult social care policy. Legal advocacy is by choice of the patient or relative/carer. This may be particularly important to anyone who lacks mental capacity.
24.9.3 Distance
There should be no artificial geographical boundary, in relation to the distance, patients and relatives may be expected to travel to initiate the discharge from hospital. However, this would be seen as an initial move to a home where capacity was available, with the ultimate move back to the home of Choice, when this becomes available. Every effort would be made to be reasonable, however, the Choice Policy clearly specifies that the Choice is in relation to where capacity is available, not specifically where the patient/client may wish to reside.
24.9.4 Self-funders
The policy for self funders should be no different to people whom Adult
Social Care fund and be consistent with regard to home of Choice directive, with self-funders being encouraged to look at places where capacity exists.
24.9.5 Private home contracts
With regard to transfer of patients from one home to another, where the first home may be requiring one month’s notice for the patient to move.
Where Adult Social Care is commissioning the package, this is a commissioning decision for the Adult Social Care & Cultural Directorate
(ASCD) to agree the way forward. However, this could be a potential issue, for self-funders specifically, where the Health and possibly Social
Discharge and Home of Choice Policy September 2010
74 of 114
Service Officers have encouraged the self-funder to take up another option. It would not seem appropriate to penalise that individual to fund the month notice period however there is no agreed policy statement to deal with this therefore each case will be dealt with individually.
Self funders should be advised about the likely cost implications of giving notice to one home when transferring to another .
24.9.6 Age
This policy will not lead to discrimination with regard to age but there is recognition that younger people, especially those with pre-senile dementia or certain other disabilities may have to travel further for their interim and possibly their preferred Choice of home.
24.9.7 Listing
Where clients/patients have agreed to move to another home prior to their move to home of Choice, where Adult Social Care are in contact with these clients, this will be followed up by social workers. However, for self-funders, this would have to be clearly specified in the information provided to them, that this would be the families’ responsibility, to continue to pursue the home of Choice and their appropriate return to that home.
24.9.8 Sharing
Some homes have rooms that are shared. Sharing of a room can only be enforced if the home is able to deliver the care appropriately within that setting, for the specific individuals and the patient’s consent. This clearly needs discussion with the patient, careful deliberations and risk assessment.
24.9.9 Home prices
There is recognition of the fact that many homes are now charging prices greater than Adult Social Care’s usual price and there may be a need for relatives to negotiate top-up fees. Decisions should be based on guidance in Appendix 3
24.9.10 Financial assessment
If a patient refuses to complete the financial assessment process requested by the ASCD the individual user/patient becomes responsible for the totality of the package until the financial assessment documentation is completed.
Discharge and Home of Choice Policy September 2010
75 of 114
24.9.11List of Choice
The variety of Choice should be confined to those homes available and who are able to meet the assessed needs of individuals. However, consideration also needs to be given to alternative options, such as interim care, intermediate care or other forms of community care service which may be able to support specific individuals.
Any list of Choice should make reference to National Guidance LAC
(2004) 20.
24.9.12Partnership responsibilities
There should be joint ownership of and preferably any joint press release and press statements would be made on a multi-agency basis.
It was recognised that the Chief Executives in the health system were backing this process and would front the potential challenges from the media. However, it was specifically noted that patients should not be physically removed from hospital wards or any other setting and that difficulties would need to be pursued through relevant processes of ongoing communication, discussion and negotiation with all parties concerned. This is about making sure patients understand, at the point of entry to the hospital/care system, what their rights are and that the right to remain in a hospital bed following treatment is not appropriate and patients would be expected to move on following the completion of their treatments.
It should be noted that whilst the Home of Choice Guidance is referring primarily to hospital beds that no one has the right to occupy a bed in any care setting if treatment is no longer required. The spirit and application of this policy will therefore need to be considered for other settings. This will have to be balanced by the fact that interim care has been developed to enable further rehabilitation and support on discharge. This step in the care pathway also needs to be explicit.
24.9.13Communications
All of this underlines the importance of clear and accurate communication by all health and social care staff with patients and their carers about discharge arrangements in order to encourage appropriate and realistic expectations from the onset .
When difficulties arise:
It should be noted that this process had top-level support and that consultants would become involved with any areas of resistance in ensuring the policy was adopted consistently across the Trusts.
Discharge and Home of Choice Policy September 2010
76 of 114
24.9.14Disputes
Legal advice has been sought by the PCT regarding Home of Choice; the guidance is seen as robust.
Legal advice has been sought by the PCT regarding the policy; the policy is seen as robust.
24.10 Sample -
Patient Leaflet “Home of Choice”
Discharge and Home of Choice Policy September 2010
77 of 114
Progress towards discharge from hospital will proceed as follows:
You, your family and carers have agreed that your needs are best met in a Residential or
Nursing Home
You should make a choice of accommodation that is currently available
If you are unable to make a choice within the identified timescales, you will be provided with a suitable alternative that is available to meet your needs to enable discharge from hospital
Discharge and Home of Choice Policy September 2010
78 of 114
NHS Cumbria
North Cumbria University Hospitals NHS Trust
Morecambe Bay University Hospitals NHS Trust
Cumbria County Council
Cumbria Partnership Foundation NHS Trust
Information to help you when discussing your move from
Hospital to a
Residential or
Nursing Home
Moving on from Hospital
Since you were admitted to Hospital, you the doctors, nurses, therapists and social workers who have been involved in your care, have been working together to assess your health and social care needs for when you leave hospital. You and your family have agreed that these needs may be best met in a
Residential or Nursing home. We are seeking to make this move so that someone else who is waiting treatment can come into the hospital.
We understand that the decision to live in a Residential or
Nursing Home is a major one and that it will involve important and significant changes for you and your family or carers.
This leaflet provides you, your family and carers with information you need to help you make your decisions once you no longer need hospital treatment or are ready to be discharged to a Residential or Nursing Home.
Advice and Guidance for Choosing a Home
Social Workers and nursing staff will offer you advice and guidance about planning for your discharge from hospital. This will involve discussing your care needs with you and your family and/or carers and deciding on the best kind of accommodation to meet your needs.
Social Workers will offer advice and assistance with funding that you may be entitled to and can provide information on
Residential and Nursing Homes to meet your needs.
Independent advice can be sought from other agencies e.g.
Age Concern.
Discharge and Home of Choice Policy September 2010
79 of 114
Timetable of Events
It is important that you continue to receive care and support in the most appropriate environment. To help us to do this, we need your co-operation and support to find a Residential or Nursing Home.
We will therefore ask you, your family and carers to make a choice of accommodation that is suitable and available without undue delay.
Once you, your family and carers have chosen a home you may have to wait until a place in that home becomes available. If this wait is likely to be more than 7 days, then we will work with you to find an acceptable alternative accommodation until the home of your choice has a vacancy.
If you fail to identify a choice of accommodation, or refuse the alternative temporary accommodation offered within a further 7 day period, the Trust will be required to take the necessary steps to discharge you to an alternative place of care.
A flow chart summarising the process is on the back of this leaflet. This leaflet follows the Discharge Policy and Cumbria
Care Home of Choice Policy
Version 3 5/09
Discharge and Home of Choice Policy September 2010
80 of 114
SECTION 9 – Monitoring the Discharge & Transfer Policy and benefits achieved
25. Monitoring the Discharge & Transfer Policy
A Discharge & Home of Choice Policy Review Group which meets quarterly was established in September, 2009 with representatives from each
Organisation with the relevant, up to date knowledge of processes, policies and performance relating to discharge and transfer of inpatients, who also represent their organisation at a senior level. The Group Chairperson is the
Senior Commissioner for Unscheduled, Complex and Continuing Care for
NHS Cumbria. The function of the Group is: o To identify / monitor performance against the policies - including actions for required change o To evaluate the impact of implementing policies & raise any issues which arise o To identify required changes to policies which maintain them as “relevant”, live, working documents” applicable to practice o To recommend actions; refer to relevant care stream boards o Escalate urgent issues
25.1 Monitoring - Benefits achieved
The purpose of this policy is to improve the quality of discharge planning and patient experience so that discharge results in timely and safe discharges and patients receiving care in the environment most appropriate to the level of their care needs.
A number of benefits are intended to be achieved with this working document including some suggestions of monitoring to ensure expectations are met:
Improving patient experience by involving patients in their discharge planning early and throughout the process
As indicated in patient notes / representation at case conferences
Feedback from case conferences
patient agreement with plans for discharge - documented in patients notes or indicated in discharge checklist
Empowered and informed patients
as reflected by patient satisfaction surveys
feedback e.g. post discharge telephone follow-up
monitoring complaints / PALS
use of voluntary services where appropriate / type of information given on which services - do cumented in patient’s notes or discharge checklist
Discharge and Home of Choice Policy September 2010
81 of 114
ability to manage care and / or self-care - documented in patient’s note
advice on lifestyle and preventative health measures - documented in patient notes - delivered by which professional group / service
Improved patient experience with the use of care pathways
evidence of the use of patient care pathways- in patients notes
mapping for example: older patients’ pathways through hospital care as an aid to identifying bottlenecks within the system
Improved provision of consistent and integrated care and transfer of care
comprehensive discharge documentation including discharge letters and summaries -
audit of discharge letters / summaries using Academy of
Royal Colleges guidance
proportion of discharge summaries to GPs within 48 hours
feedback from Primary Care / Community Services
looking at days of the week, time of discharges / transfers - any delays in prescriptions not available or wait for ambulance transfer etc
Increased numbers of patients discharged on the “expected date of discharge” [EDD] [as this is based on anticipated length of stay and is set within 24 hours of admission and reviewed daily if stay longer than 24 hours for simple discharges and as soon as daily, clinical assessment deems possible for complex discharges]
When EDD recorded during the hospital stay / how often reviewed
What proportion were actually discharged before or after the
EDD and the reasons for this variance
Increased number of bed days saved / reduction in length of hospital stay
Feedback from bed managers / standardised reports
Analysis of pattern of discharge - days of the week & times to ensure discharge 7 days a week & bank holidays
Increased number of patients discharged on the “proposed date of discharge” and a reduction in numbers of delayed discharges
Feedback from Discharge coordinators
standardised reports - Delayed Transfer of Care
Case note review - determine reasons
Improved medicine management and patient concordance
Within 72 hours of patient discharge - as per guidance in
Section 13 of this document - documented in patient’s notes
Appropriate utilisation of medical, nursing and other professional skills
Review of case conferences - where specialties / specialists input required but not available
Discharge and Home of Choice Policy September 2010
82 of 114
Number of NHS Decision Support tools returned from NHS
Continuing Healthcare Panel for lack of evidence
Review of Referrals by Professional Group - proportion of inappropriate referrals / total number of referrals / response times
Review of proportion of documentation / prescriptions completed by Medical team as per standard - within 24 hours of agreed date of discharge
Reduction in readmission within 48 hours for same condition
Standardised report - emergency readmissions - case note review to determine reason - if diagnostic code appears to be different
Reduction in hospital-acquired infections
Infection Control team / standardised reports
Some examples of useful Audit Tools -
25.2
For organisational audit tool - Self Assessment for Discharge
Planning See: http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/P ublicationsPolicyAndGuidance/Browsable/DH_4924381
25.3
For medical staff audit of documentation - covering discharge See audit tool at: http://hiu.rcplondon.ac.uk/clinicalstandards/recordsstandards/rec
_summary.asp
The following two, audit proformas have been included with this policy
25.4 Audit of Inpatient Records - to analyse the quality of discharge planning
25.5 Audit of the quality of discharge from the Community / Primary
Care perspective, caring for the patient immediately post-discharge
Discharge and Home of Choice Policy September 2010
83 of 114
25.4
Discharge Policy Audit Tool - INPATIENT RECORDS
Please select 10 case notes of patients whom have been in patients over the last year for a minimum of 3 consecutive nights and examine their case notes for evidence of the following information:-
Patient’s Study
Number
Admission
Date
Discharge date
INPATIENT RECORDS Yes No Exceptions Details of
Exception
Discharge planning began early, as evidenced by:
1 The Expected Date of Discharge
[EDD] was documented on Pre-
Admission / or within 24 hours of
Admission
2 A named person was identified for coordinating discharge within 24 - 48 hours of admission
3 The appropriate Single Assessment documentation was completed as part of the admission process
Discharge planning was an on-going process, as evidenced by:
3 The EDD was reviewed daily / recorded in patients notes [where admission was longer than 24 hours]
4 Appropriate referrals been completed for complex cases as per the response time specified for each specialty / agency
5 The NHS Continuing Healthcare
Needs Checklist was completed.
The patient was well - prepared for discharge, as evidenced by:
5 Documented in patient record - they are fit for discharge [no longer require acute care and are safe for discharge].
6 Documented - patient agrees to discharge arrangements.
7 An assessment of adherence with medications has been carried out within 72 hours of discharge, and it is documented that patient understands and is able to use medications.
8 14 days supplies of medicines, dressings and appliances were available on discharge and sent with patient.
9 Discharge checklist has been
Discharge and Home of Choice Policy September 2010
84 of 114
completed.
10 Discharge took place on the proposed date of discharge
11 If discharge beyond proposed date, what was the reason for the delay?
Discharge communication enables appropriate follow-up which does not compromise care or patient safety, as evidenced by:
12 Documented discharge letter sent with patient at the time of discharge
13 Discharge letter complete [as per standard listed in 4.7.1]
14 List information missed from Discharge Letter
15 Evidence Discharge Summary sent to
GP with 24 hours
16 Discharge summary complete [as per standard listed in 4.8.1]
17 List information missed from Discharge Summary
25.5 Discharge Policy Audit Tool - Primary / Community Care
10 patients from each community hospital and from each ward in each
Acute hospital have been selected for an audit of the Discharge Policy.
Where these patients have required ongoing care from your service the following information will be requested of you. In order to protect patient anonymity the details of the patient concerned will be given to you separately by ward staff and should not be recorded on this document, with the exception of any patient study number specific to this audit that you are given by the ward staff.
COMMUNITY STAFF QUESTIONNAIRE
Patient’s Study Number
1. Was this patient known to you before their admission to hospital?
Yes No
2. If yes did you contact the hospital to contribute to the ward’s
assessment and treatment of this patient during their stay in hospital?
Yes No
Discharge and Home of Choice Policy September 2010
85 of 114
SECTION 10: - Governance of Information Related to Discharge and Transfer of Patients
26. Sharing Information between Organisations
Yes No Not appropria te
Were you notified about this patient’s possible discharge before they were discharged?
Did your service have involvement in the discharge planning of this patient?
Did your service have an opportunity to attend the case conference of this patient?
Was the discharge documentation, medication and any dressings, appliances or equipment with the Patient when they were discharged?
Was the documentation, medication, any dressings, appliances or equipment adequate [e.g. information on documentation sufficient for you to safely pick up care of patient and supplies sufficient for 14 days]
If no, explain what was missing, and it’s impact on patient’s care
Is there any evidence that patient/ carer was aware of how to use medications obtained during hospital?
If no, explain any difficulties patient / carer had regarding medication:
Is there any evidence that patient/ carer was aware of how to use any equipment obtained during hospital?
If no, explain any difficulties patient / carer had regarding equipment:
In your opinion was this a safe discharge which was successful as it did not compromise care?
If no, please explain, and suggest “contingency plans” which could have been put in place.
Discharge and Home of Choice Policy September 2010
86 of 114
26.1 NHS Cumbria recognises the benefit of working in partnership and that in some instances information needs to be shared between the NHS and
Organisations in support of achieving the discharge and transfer of a patient.
26.1.2 Statutory powers for sharing information already exists for some cases in the following legislation:
Children Act 1989
Children Act 2004
Crime and Disorder Act 1998
Criminal Justice Act 2003
Data Protection Act 1998
Human Rights Act 1998
NHS Confidentiality Code of Practice 2003
Police and Criminal Evidence Act 1984
Police Reform Act 2002
Road Traffic Act 1988
Terrorism Act 2000
26.2 Multi-Agency Public Protection Arrangements Protocol
26.2.1 Where such information sharing is not provided for under legislation, staff should familiarise themselves with the respective information sharing agreement for their organisation and the particular client group that is being transferred or discharged, in order to determine how and when personal information may be shared. The agreement should set out:
how the information sharing process will be conducted and recorded
set minimum standards for preserving information so that it is secure and protected from compromise, but available to those with a professional need to know
26.2.2 When considering whether information can be shared, individuals need to take into account Trust policies, national codes of practice and guidelines for best practice etc and determine whether there are any constraints or guidelines which the nature of their work places upon them. When considering these risks, the central concern where information sharing about individuals is involved, is whether the sharing is justified balanced against the rights of the individual set out in the Data Protection Act 1998 and the Human Rights Act 1998.
26.2.3 Consent to contact and seek the support of partner organisations should be sought from all individuals (or their carer, parent or guardian where appropriate). Consent should be both explicit and informed, and freely
Discharge and Home of Choice Policy September 2010
87 of 114
given by the person involved. Consent should include permission for information to be requested from other organisations as appropriate, as well as information provided by the responder.
26.2.4 Information to be provided in response to a request may be returned by any means agreed between the partners as befits the sensitivity and urgency of the information required. Permitted formats for the exchange of sensitive personal information should follow Trust policy, and staff must ensure they are familiar with the approved methods.
26.3 Retention & Destruction of Records
See guidance:
http://www.dh.gov.uk/en/PublicationsandStatistics/Publications/Publication sPolicy
26.4 Security
Do not save information on “desktop” or C: drive. Ensure information is saved to the drive on the PC that can be backed up, so that it is secure.
Discharge and Home of Choice Policy September 2010
88 of 114
APPENDIX 1: Glossary of Terms
Assessment A process whereby the needs of an individual are identified and their impact on daily living and quality of life evaluated.
Care Management A process whereby an individuals needs are assessed and evaluated, eligibility for services is determined, care plans devised and implemented and needs are monitored and reassessed.
Care Manager A practitioner who, as part of their role, undertakes care/case management.
Care Package A combination of services designed to meet a persons assessed needs.
Care Pathway An agreed and explicit route an individual takes through health and social care services.
Carer A person usually relative or friend who provides care on a voluntary basis.
Case Co-ordinator A professional who co-ordinates the care plan, monitors provision and facilitates communication between agencies. Maintains contact with the patient and ensures reviews are undertaken.
Closer to Home A policy to develop services to support patients receiving appropriate care closer to their homes.
Community Hub To act as the central point of referral for community services within a locality for service users who require rapid access to care, reassessment of care needs following a new episode of illness or breakdown of social care, have complex and multiple needs, require an episode of rehabilitation including short term intervention or longer term rehabilitation or access to a community bed.
Discharge and Home of Choice Policy September 2010
89 of 114
Community Matron A case co-ordinator who actively manages and joins up care by offering, amongst others, continuity of care, coordination and a personalised care plan for vulnerable people most at risk.
Fit for Discharge When physiological, social, functional and psychological factors or indicators have been taken into account following a multi-disciplinary assessment if appropriate, and it is safe for the patient to be discharged or safe to transfer from hospital to home or another setting.
Patients do not have to be clinically stable to be discharged where they can be managed safely at home / community through input from services such as Short-Term Interventions.
Individualised Budgets The value of the sum determined by a local authority to support a person following an assessment of their needs for social care support.
Medicines Reconciliation Defined as the process of obtaining up to date and accurate medication list that has been compared to the most recently available information and has documented any discrepancies, changes, deletions or additions, resulting in a complete list of medications accurately communicated.
Multi-agency Services or activities which involve staff drawn from a range of organisations, such as statutory agencies (health, social services, education etc) and voluntary groups.
Multi-disciplinary When professionals from different disciplines work together.
Multi-disciplinary assessment An assessment of an individuals needs that has actively involved professionals from different disciplines in collecting and evaluating this information.
Discharge and Home of Choice Policy September 2010
90 of 114
NHS Funded Continuing Healthcare -
Continuing Care - care provided over an extended period of time to a person aged 18 or over. This care may be delivered by a combination of health and social care services to meet the physical or mental health needs of someone as a result of disability, accident or illness.
NHS Continuing Healthcare - a package of
Continuing care arranged and funded solely by the NHS.
Joint Package of Continuing Care - arranged where a person does not qualify for NHS
Continuing Healthcare, but the NHS and Local
Authority both have responsibility to contribute to that person’s care.
NHS Funded Nursing Care - funding provided by the NHS to care homes providing nursing.
This supports the provision of nursing care by a registered nurse for those assessed as
Nurse-Led Discharge within clear protocols.
Primary Care Assessment Service A unit staffed by Primary Care which undertakes assessment and treatment of minor illnesses and injuries; care that was previously managed by GP Out of Hours, Minor Injury
Units and A&E for less serious attendees.
Rehabilitation eligible.
Is about Nurses taking responsibility for initiating, driving and following through on the decision to discharge which may be carried out in partnership with medical colleagues and
A programme of therapy and re-enablement designed to restore independence and reduce disability.
Self-directed Support The County Council recognises that, apart from a very few individuals, people make decisions affecting their lives on a daily basis .
It is
Discharge and Home of Choice Policy September 2010
91 of 114
Single Assessment Process
Timely Discharge important that those individuals who are able to do so, are supported in making their own decisions and deciding for themselves how support should be organised to meet their needs. This is equally true if they require support and meet the criteria for services determined by the County Council.
A process that places the individual at the heart of assessment, with care plans that ensure people receive effective and timely responses to their health and social care needs with care that is co-ordinated to prevent duplication by professionals.
Timely discharge is when the patient is discharged home or transferred to an appropriate level of care as soon as they are safe for discharge/transfer.
Discharge and Home of Choice Policy September 2010
92 of 114
APPENDIX 2: Supporting Policies, Protocols and Documentation
The Discharge and Transfer Policy should be read in conjunction with the following:
Continuing Care Pathway Framework
Home of Choice Policy and Guidance
HM Transfer Prison Policy
Infection Control Policy
Northwest Ambulance Policy
Medication Policy
Mental Capacity Act
Multi-agency Mental Capacity Act Policy
Safeguarding Adults - CPT /001/027
Safeguarding Children - CPT/001/037
Single Assessment Process
Information Sharing Protocol, September 2009 (NHS Cumbria)
Records Management Strategy, September 2009 (NHS Cumbria)
Records Management Procedures, September 2009 (NHS Cumbria)
The Home of Choice section should be read in conjunction with the following:
Local Authority Circular - LAC(2004)20
National Assistant Act 1948 (Choice of Accommodation) Directions 1992
Guidance on National Assistance Act 1948 (Choice of accommodation)
Directions 1992
Updated Guidance on National Assistance Act 1948 (Choice of accommodation) Directions 1992 Results of Public Consultation
New guidance published on Choice of accommodation directions
Published Thursday 14 October 2004 Reference No: 2004/0366
Discharge and Home of Choice Policy September 2010
93 of 114
National Assistance (Residential Accommodation) (Additional Payments and Assessment of Resources) (Amendment) (England) Regulations 2001
NHS Cumbria Escalation Policy v. 4, Draft, March 2009
Discharge and Home of Choice Policy September 2010
94 of 114
APPENDIX 3: Underpinning Principles for Effective Discharge and Transfer of Care & Home of Choice
Principles in this policy are underpinned by the:
1) Discharge from Hospital Pathway Process and Practice DOH 2003
2) Community Care [delayed discharges] Act 2003
3) The National Framework for NHS Continuing Healthcare and NHS
Funded Care 2007
4) Mental Capacity Act 2005
5) NHS Constitution 2009
3.1 Discharge from Hospital Pathway Process and Practice DOH 2003
Key Points:
Unnecessary admissions are avoided and effective discharge is facilitated by a “whole system approach” to assessment processes and the commissioning and delivery of services
The engagement and active participation of people who use the services and their carer(s) as equal partners is central to the delivery of care and in the planning of a successful discharge.
Discharge is a process and not an isolated event. It has to be planned at the earliest opportunity across the primary, hospital and social care services, ensuring that patient and their carer(s) understand and are able to contribute to the care planning decisions as appropriate.
The process of discharge planning should be co-ordinated by an acting named person who has responsibility for co-ordinating all stages of the patient journey. This involves liaison with the preadmission case co-ordinator / care manager / community matron, district nurse or social worker in the community at the earliest opportunity and the transfer of those responsibilities on discharge.
Staff should work within a framework of integrated multidisciplinary and multi-agency team working to manage all aspects of the discharge process.
Effective use is made of transitional and intermediate care services so that existing acute hospital capacity is used appropriately and patients achieve their optimal outcome.
The assessment for and delivery of continuing health and social care is organised so that individuals understand the continuum of health and social care services, their rights and receive advice and information to enable them to make informed decision about their future care.
Discharge and Home of Choice Policy September 2010
95 of 114
3.2 Community Care [delayed discharges] Act [2003]
Overview:
New duties were placed upon the NHS and Local Authorities [LA] in
England relating to improved communication between health and social care systems in relation to the discharge of patients and also communication with patients and carers. The NHS is required to notify the councils of any patient’s likely need for community care services, and the patients proposed discharge date.
The Act also introduced a system of Reimbursement for delayed hospital discharges [The local process is described in detail in Cumbria
Partnership Executive Reimbursement Protocol 2005]. This applies currently to adult patients receiving acute medical care. If a patient remains in hospital because the LA is unable to access or put in place the services that the patient or carer need for discharge to be safe, the council is then liable to pay the NHS body a charge per day of delay.
This duty provides a financial incentive for LA’s to promptly address and transfer people from an acute ward to a more appropriate setting as soon as they are ready for discharge, and provide an appropriate range of support to facilitate avoiding unnecessary admissions.
Currently, non-acute beds and mental health beds are not included in reimbursement, but Department of Health have made clear their intention to include them in the future. The Cumbria Care Home of Choice Policy and Guidance will aim to reduce the delays in discharge by encouraging timely discharge to an appropriate environment.
Primary Care Trusts have a key role to play in working with the NHS bodies and Councils in identifying the main causes of delay in their local systems and in channelling investment to tackle these in order to reduce delays and thus the need for reimbursement. Strategic Health Authorities have a specific duty under the act to establish dispute resolution panels.
3.3 National Framework for NHS Continuing Healthcare and NHS Funded
Care 2007
Overview:
The Department of Health describes continuing care as the provision of care over an extended period of time as the result of disability, accident or illness to meet both physical and mental health needs. It can be provided
Discharge and Home of Choice Policy September 2010
96 of 114
in a range of settings from an NHS Hospital, Care Home or Hospice to a person’s own home.
Continuing Care can include both health and social care funding.
Every patient over age 18, who may have continuing care needs must be considered for eligibility for NHS Continuing Healthcare before any long term plans are put in place [Follow the process set out in Section 6].
If individuals, following a multi-disciplinary assessment are identified as possibly meeting the criteria and a referral made to a team of funded NHS care assessors team. They will carry out their assessment and apply the criteria to determine eligibility.
The above applies regardless of whether the individual is in a hospital care home or their own home. The NHS is responsible for arranging as well as funding continuing care services.
3.4 Mental Capacity Act 2005
Overview:
The Act applies to people over 16 in England and Wales. It protects people who cannot make their own decisions about some things. The act sets out:
How to help someone make their own decision about something
How to work out if someone can make their own decisions
about something
What to do if someone can’t make decisions about something sometimes
The Act sets out 5 key principles which underpin the legal requirements.
These are a. A person must be assumed to have capacity unless it is established that they lack capacity. b. A person is not to be treated as unable to make a decision unless all practicable steps to help him to do so have been taken without success. c. A person is not to be treated as unable to make a decision merely because he makes an unwise decision. d. An act done, or decision made, under this Act for or on behalf of a person who lacks capacity must be done, or made, in his best interests.
Discharge and Home of Choice Policy September 2010
97 of 114
e. Before the act is done, or the decision is made, regard must be had to whether the purpose for which it is needed can be as effectively achieved in a way that is less restrictive of the person’s rights and freedom of action.
No one can assume a person lacks capacity because of how old they are, how they look, or how they behave.
No one can assume a person cannot make a decision because of their disability, their inability to make more complicated decisions or because they have not been able to make decisions like that in the past.
Where someone has to make a decision on behalf of a person who lacks capacity, they must decide what is in the person’s best interests. This can only be done properly by listening to what the person wants, consulting people who know them, and making sure they are involved.
Assessing Capacity
The person who assesses an individual’s capacity to make a decision will usually be the person who is directly concerned with the individual at the time the decision needs to be made. This means that different people will be involved in assessing someone’s capacity to make different decisions at different times e.g. a HCA may need to assess if a person can consent to being bathed or a staff nurse may need to establish capacity to consent to change a dressing. In health care settings most care and treatment is provided by a multidisciplinary team, however, the establishment of capacity to consent is the responsibility of the person proposing the treatment. If anyone thinks a person lacks capacity, it is important to then ask the following questions:
Does the person have all the relevant information they need to make the decision?
If they are making a decision that involves choosing between alternatives, do they have information on all the different options?
Would the person have a better understanding if information was explained or presented in another way?
Are there times of day when the person’s understanding is better?
Are there locations where they may feel more at ease?
Can the decision be put off until the circumstances are different and the person concerned may be able to make the decision?
Can anyone else help the person to make choices or express a view
(for example, a family member or carer, an advocate or someone to help with communication)?
Lack of Capacity / Lack of ability to decide:
Discharge and Home of Choice Policy September 2010
98 of 114
For the purposes of the Act, a person lacks capacity in relation to a matter if at the material time he is unable to make a decision for himself in relation to the matter because of an impairment of, or a disturbance in the functioning of, the mind or brain. This means that a person lacks capacity if:
they have an impairment or disturbance (for example, a disability, condition or trauma) that affects the way their mind or brain works, and
the impairment or disturbance means that they are unable to make a specific decision at the time it needs to be made.
A person is unable to make a decision if they cannot:
understand information about the decision to be made (the Act calls this ‘relevant information’)
retain that information in their mind
use or weigh that information as part of the decision-making process, or
communicate their decision (by talking, using sign language or any other means)
Independent Mental Capacity Advocates [IMCAs]
The Act sets up a new service, Independent Mental Capacity Advocates
[IMCAs] for people who have no family or friends to provide help with decisions.
An IMCA is needed when there is no-one close to the person who lacks capacity to give an opinion about what is best for them, and:
an NHS body is proposing to provide serious medical treatment or
an NHS body or local authority is proposing to arrange accommodation in hospital or a care home or other longer-term accommodation and
– the person will stay in hospital longer than 28 days, or o they will stay in a care home for more than eight weeks.
It is the person responsible for the proposed treatment (the decision maker) who is responsible for contacting the IMCA service.
IMCA services in Cumbria are provided by Advocacy Experience who can be contacted on
Mobile 0844 800 2776
Tel 01925 651400
Email IMCA@advocacyexperience.com
Power of Attorney
Sometimes one person will want to give another person authority to make a decision on their behalf. A power of attorney (LPA) is a legal document that allows them to do so. Under a power of attorney, the chosen person
(the attorney or donee) can make decisions that are as valid as one made
Discharge and Home of Choice Policy September 2010
99 of 114
by the person (the donor). LPAs can cover personal welfare (including healthcare and consent to medical treatment) for people who lack capacity to make such decisions for themselves. Personal welfare LPAs might include decisions about:
where the donor should live and who they should live with
the donor’s day-to-day care, including diet and dress
who the donor may have contact with
consenting to or refusing medical examination and treatment on the donor’s behalf
arrangements needed for the donor to be given medical, dental or optical treatment
assessments for and provision of community care services
whether the donor should take part in social activities, leisure activities, education or training
the donor’s personal correspondence and papers
rights of access to personal information about the donor, or
complaints about the donor’s care or treatment.
Advanced Decisions
The Act also introduces the legal framework for Advanced Decisions. An advance decision enables someone aged 18 and over, while still capable, to refuse specified medical treatment for a time in the future when they may lack the capacity to consent to or refuse that treatment. It has the same effect as a decision that is made by a person with capacity: healthcare professionals must follow the decision. If the advance decision refuses life-sustaining treatment, it must:
be in writing (it can be written by a someone else or recorded in healthcare notes)
be signed and witnessed, and
state clearly that the decision applies even if life is at risk.
To establish whether an advance decision is valid and applicable , healthcare professionals must try to find out if the person:
has done anything that clearly goes against their advance decision
has withdrawn their decision
has subsequently conferred the power to make that decision on an attorney, or
would have changed their decision if they had known more about the current circumstances.
Advance decisions to refuse treatment for mental disorder may not apply if the person who made the advance decision is or is liable to be detained under the Mental Health Act 1983.
Discharge and Home of Choice Policy September 2010
100 of 114
Consent for Children and Young People (CYP)
The care and treatment of Children and Young People (CYP) and their capacity to consent is a complex area involving several areas of legislation including
Legislation Scope
Section 8
Family Law
Reform Act
1969
Children
1989
Act
Consent to treatment of 16 & 17 year olds : their consent to treatment as effective as if they were of full age (they are presumed to have capacity to consent)
Wide ranging provisions concerning care
& upbringing of children & young people
( under 18 ); including: definition of parental responsibility; care orders; child protection and secure accommodation, services for children ‘in need’.
Mental
Capacity Act
2005
Legal framework for decision making on behalf of people ( aged 16 and over ) who lack capacity to make decisions for themselves. DOLS apply only to 18 & over
Mental Health
Act 1983
Makes provision for compulsory admission to hospital and treatment for mental disorder as well as Supervised
Community Treatment – no age limits
Also, decisions relating to CYP (including those in respect of discharge) can be made by those individuals who have Parental Responsibility for CYP provided the fall within the Zone of Parental Responsibility (ZPR). A brief summary is given below:
Legal
Authority
YP able to YP unable to Competent consent consent Child
N/A Yes YP/Child consents
Yes
MCA 2005 N/A Yes, if lacks N/A capacity within MCA & treatment not involve detention
Child lacks competence
N/A
N/A
Discharge and Home of Choice Policy September 2010
101 of 114
Parent consents
Do not rely Yes, if within Do not rely Yes, if within on consent ZPC on consent
MHA 1983
NHS Constitution 2009
Court If MHA criteria not met, apply to court
ZPC
3.5 NHS Constitution 2009
Key points:
The Constitution establishes the principles and values of the NHS in
England. It sets out the rights to which patients, public and staff are entitled, and pledges which the NHS is committed to achieve, together with responsibilities which the public, patients and staff owe one another to ensure the NHS operates fairly and effectively.
In respect of discharge, the patient has the right to:
Respect, consent and confidentiality
Each person will be treated with respect and courtesy
Personal information will be kept confidential, patient records will be kept safe and secure
Patient’s can have access to their own health records, including any letters sent between clinicians about their care
Informed Choice
Patients have a right to make choices about their NHS care and to information to support these choices.
Involvement in Healthcare
Patients have a right to be involved in discussions and decisions about their healthcare, and to be given information to enable them to do this.
The NHS commits to:
Make the transition between services / discharge as smooth as possible
Ensure decisions are made in a clear and transparent manner
Discharge and Home of Choice Policy September 2010
102 of 114
3.6 Patient’s And Carer’s Discharge Standards
Patients being discharged from hospital have the right:
To full information on their diagnosis and the assessment of their health and social needs in preparation for discharge.
To be fully involved in planning their own discharge, together with a relative, carer or friend as appropriate.
For the discharge plan to start on or before admission where possible.
To full information on the services available in the community relevant to their care.
To full information on short or long term nursing or residential care; including financial implications.
To be given an appropriate contact number where they can get help or advice on discharge.
To be given a clear, legible discharge letter detailing the support services provided for them [where appropriate].
To full information on health authority eligibility criteria for continuing care.
The discharge planning team to be available as a point of contact to offer support and advice to patients, carers, statutory and voluntary agencies.
Information on advocacy support.
To have access to the trust complaints procedure and any complaint regarding their discharge arrangements investigated and a full explanation given.
If still not satisfied, then to be given access to the health service commissioner
Source: Discharge from hospital:, pathway, process and practice, Appendix 4.3,
Department of Health, 28 January 2003.[Page 45]
Note: adapted from the work of the liaison nurses, York Health Services Trust.
Discharge and Home of Choice Policy September 2010
103 of 114
APPENDIX 4: Example of DH “DISCHARGE CHECKLIST”
Addressograph
Patient NHS No
Patient Name
1 Length Of
Stay (LOS)
Discharge Planning Checklist
Signature Record
All members of staff using this Integrated Care Pathway should use Black ink and complete either the Trust’s signature sheet or the signature sheet in the
Introduction Section of the Easy Care Documentation.
State the anticipated length of stay for the patient in days………………..……… Initials……………..
Before admission to hospital or on admission to hospital
Yes
Initials
No
Initials
Date Time State reason(s) if this has not happened
2 Emergency social problems
Has the anticipated
LOS been discussed with patient and carer?
Are there any emergency social problems created by admission?
3
GP Is the patient registered with a GP?
State the patient’s pre admission abilities in relation to potential discharge issues
4 Existing services
Does the patient have any existing support services at home?
Yes
Initials
No
Initials
Date Time
If yes, has telephone referral been made to Social
Services?
□ Yes □ No
If no, advise the patient on how to register.
Actions
5 Pre
Admission
Abilities
6
Does the patient require help with activities of living?
Is a referral required to
Social Services?
If yes, complete the appropriate assessment using the Single
Assessment
Process /
Documentation
If yes, complete the appropriate assessment using the Single
Assessment
Process /
Documentation
If yes, refer using the Single
Assessment
Discharge and Home of Choice Policy September 2010
104 of 114
Referrals Is a referral required to
Physiotherapy?
Is a referral required to
Occupational therapy?
Process
If yes, refer using the Single
Assessment
Process
If yes, refer using the Single
Assessment
Process
Within 24 hours of admission
7
Predicted date of discharge
Has the MDT agreed treatment plan?
Has the predicted date of discharge been identified?
Has the predicted date of discharge been discussed with the patient and carer?
8
Patient information
Has the patient been given relevant literature?
During Admission
Yes
Initials
No
Initials
Date Time State reason(s) if this has not happened
□ Awaiting diagnostic tests
□ Awaiting consultant’s decision
□ Awaiting for
MDT decision
□ Other state
9 Nurse Led
Discharge
Yes
Initials
No
Initials
Date Time State reason(s) if this has not happened
10 Continuing
Health
Care
11 RNCC
12 Length of
Stay (LOS)
Has the MDT agreed the suitability of the patient for the Nurse
Led Discharge?
Does the patient require a Continuing
Health Care referral?
Does the patient require a Registered
Nurse Care
Contribution (RNCC)?
Will the patient be discharged within their anticipated LOS?
If yes, refer to the Discharge
Liaison Nurse
(DLN) and state why
If yes, refer to the DLN and state why
□ Medically unstable
□ Delayed discharge – refer to the
DLN
□ Other state
Discharge and Home of Choice Policy September 2010
105 of 114
Patient NHS No
Patient Name
Addressograph
At Least 24 – 48 hours before discharge, complete this Discharge Checklist
Yes
Initials
No
Initials
Date Time State reason(s) if this has not happened
13
Diagnosis
14
Patient and carer arrangements
15 Support
Services
16 Discharge
Summary
17 Time of discharge and use of the Discharge
Lounge
Does the patient understand their condition and treatment plan?
Has written advice been given to patient?
Has the discharge arrangements been confirmed with the patient and carers?
Is the patient returning to their normal place of residence?
Has the patient got a key?
Has the patient got clothes?
Is there food at home?
Is the heating on at home?
Has the discharge arrangements been confirmed with the service providers?
□ Social Services □
GP □ DN
□ Other state
Has the Single
Assessment documentation been completed detailing the patient’s current care needs?
Is the patient being discharged after 10 am?
If yes, is the patient being transferred to the Discharge
Lounge? □ N/A
Has the Discharge
Lounge been contacted & transfer arranged? □ N/A confirmed?
□ Own / Carer /
106 of 114
If no, order a temporary GP letter
State time
If no, why not?
19 Medication
20 Medical
21 certificate
Equipment
Relative □ Taxi
□ Hospital Transport
□ Other
If hospital transport is being considered does the patient meet the Hospital
Transport criteria?
Has the patient’s medication (TTO’s) been ordered?
Medication explained to patient?
Is a Medical (sick)
Certificate required?
Has the patient received and been educated in the use of any aids / equipment
22 OPA Outpatient appointment(s) made?
□ Given to patient
□ Posted
If yes, has it been issued?
□ Yes □ No
If yes, complete equipment section on the multi
Professional
Discharge
Summary
□ N/A
Discharge and Home of Choice Policy September 2010
107 of 114
State time patient leaves the ward: …………….. Initials ……..
Day of Discharge Yes
Initials
No
Initials
Date Time State reason(s) if this has not happened
23 Clinically Is the patient clinically fit
Fit for discharge?
24 GP letter GP letter □ Given to patient
□ Faxed □ Posted
25 Valuables Has the patient’s valuables / property been returned?
Extracted from the Department of Health - Discharge Planning Checklist
Version 1 - October 2005
Discharge and Home of Choice Policy September 2010
108 of 114
APPENDIX 5: Guidance on Discharge Summaries - Agreed
Standards -Academy of Royal Colleges
[these are one the clinical quality performance indicators in the quality schedule of the Acute contracts]
Discharge/transfer Communication http://hiu.rcplondon.ac.uk/clinicalstandards/recordsstandards/DRAFT_Stds_6-
0_Discharge.doc
Standard 11
A clinical communication must be provided for all doctors involved in the care of the patient when care is transferred out of the hospital.
All doctors involved in the care of a patient includes the general practitioner and any secondary/tertiary care consultant who either regularly cares for the patient or that the patient has been referred to.
Standard 12
The patient must be informed as to what information will be communicated to which other doctors involved in their care, and given the opportunity to object, in accordance with GMC guidance.
Consent should be obtained for disclosure of clinical information and documented.
Standard 13
A copy of the clinical communication must be kept in the record.
Standard 14
The Patient should be given a copy of the clinical communication, unless it is clinically inappropriate to do so.
It should be recorded that the patient has been given a copy of the clinical communication unless it is clinically inappropriate to do so, in which case the reason should be documented.
Standard 15
If the communication is duplicated using carbon copy paper then the duplicate sheets must be legible.
Standard 16
The clinical communication should be dispatched so that it is available to the receiving doctor when the patient is next seen.
Standard 17
The transfer or discharge communication should contain information under the following headings:
20 Clinical Documentation
21 Care Event
22 Review of case
23 Current Confirmed Diagnoses
Discharge and Home of Choice Policy September 2010
109 of 114
24 Significant Past Illnesses
25 Risks and Warnings
26 Procedures: Treatments
27 Problems and Issues
28 Care Plan
29 Projected and Actual Outcomes
30 Provision of Information to Patient and Carers
31 Personal Preferences
Other headings from Standard 3 may also be used.
Standard 18
Discharge summary information should be validated by a responsible clinician
Standard 19
Discharge Summaries should be multidisciplinary where multidisciplinary care is to be continued
Discharge and Home of Choice Policy September 2010
110 of 114
REFERENCES
Care Service Improvement Partnership (CSIP) Planning for Discharge www.cat.csip.org.uk/index.cfm?pid=8
Cumbria Health and Well-being Scrutiny Committee, Adult Social Care
Scrutiny Panel, (04/2007), “Together We Care, The Joint Care Management of Older People with Complex Needs” www.scrutiny/cumbria.gov.uk
Cumbria Partnership Executive (2005) Reimbursement Protocol, Protocol for the Management of Discharge Arrangements from Acute Hospitals, Version 8
Cumbria PCT (2006) Cumbria Care Home of Choice Policy and Guidance
Department of Health (2000) Practitioners Guide to Carers’ Assessment, under the Carers’ and Disabled Children Act www.devon.gov.uk/contrast/practitionersguide-2.pdf
Department of Health Change Agent Team (2003) Definitions of Medical
Stability and “Safe to Transfer”, London: Department of Health Change Agent
Team with input from Reimbursement Implementation Team www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_4071847
Department of Health, Prison Health and HM Prison Service (2006) A Twelvemonth Study of Prison Healthcare Escorts and Bedwatches, London, DH www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_062794
DH (2009) NHS Constitution www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_093419
DH (2007) Effectiveness of Inpatient Discharge Procedures www.dh.gov.uk/en/Researchanddevelopment/A-
Z/Primaryandsecondarycareinterface/DH_4015561
DH (2007) “Single Assessment Process (SAP) for Older People” www.dh.gov.uk/en/SocialCare/Chargingandassessment/SingleAssessmentPr ocess/index.htm
DH (2004) Achieving Timely “Simple” Discharge from Hospital: a Toolkit for the Multi-disciplinary Team www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_4088366
DH (2004) The Continuing Care (NHS Responsibilities) Directions
Discharge and Home of Choice Policy September 2010
111 of 114
www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsLegislati on/DH_4077239
DH (2004) The Delayed Discharge (Continuing Care) Direction www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsLegislati on/DH_4077240
DH (2004) National Standards, Local Action: Health and Social Care
Standards and Planning Framework 2005/06 0 2007/08 www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_4086057
DH (2004) Annex A, Standards for Better Health www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_4086057
DH (2003) Discharge from Hospital, getting if right for people with Dementia, a
Supplementary checklist to help with planning the discharge from acute general hospital settings of people with Dementia www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_4007881
DH (1999) Discharging responsibilities of discharge liaison nurses and their role in discharge planning, Department of Health (downloadable copy is not available)
Health and Social Care Joint Unit & Change Agent Team (2003) Discharge from Hospital: Pathways, Process and Practice, DH www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAn dGuidance/DH_4003252
Health Informat ics Unit, “Clinical Standards, Record-keeping for Inpatients,
Discharge and Transfer Communication”, Royal College of Physicians http://hiu.rcplondon.ac.uk/clinicalstandards/recordsstandards/rec_summary.as
p
HSC 2003/009, LAC (2003) 21 The Community Care (Delayed Discharges etc) Act, Guidance for Implementation www.dh.gov.uk/en/Publicationsandstatistics/Lettersandcirculars/Healthservice circulars/DH_4064934
Joyce, Theresa, (2007) Guidance on Determining the Best Interests of Adults who lack the Capacity to make a Decision (or Decisions) for themselves
(England and Wales), British Psychological Society
Mental Capacity Act, 2005, Office of Public Sector Information, www.opsi.gov.uk/acts/acts2005
Discharge and Home of Choice Policy September 2010
112 of 114
National Audit Office (2003) Ensuring the Effective Discharge of Older
Patients from NHS Acute Hospitals, London, The Stationery Office www.nao.org.uk/publications/0203/ensuring_the_effective_dischar.aspx
National Prescribing Centre, “Medicines Reconciliation, A Guide to
Implementation” www.ncpi.org.uk/medicines_management/safety/reconcil/library/guide_reconc iliation.php
NHS Cumbria “Control of Infection Manual which constitutes the policies and procedures for infection control throughout the Trust” www.cumbria.nhs.uk/pct/about/publications/policies/clinical/Infection%20Contr ol%20Policies%20Introduction.pdf
NHS Cumbria “Transfer of Patients Policy” CPCT/001/002
NICE and National Collaborating Centre for Primary Care (2009) “Medicines
Adherence
– Involving Patient in decisions about prescribed medicines and support adherence” NICE Clinical Guidance 76, January http://www.nice.org.uk/nicemedia/pdf/CG%2076%20Medicines%20adherence
%20QRG%20FINAL.PDF
NICE and National Patient Safety Agency (2007) Technical patient safety solutions for medicines reconciliation on admission of adults to hospital.
December, www.nice.org.uk/nicemedia/pdf/PSG001GuidanceWord.doc
North Cumbria Acute Hospitals NHS Trust (2004) Discharge Policy
Royal Pharmaceutical Society of Great Britain (2005) The safe and secure handling of medicines, A Team Approach - A revision of the Duthie Report
(1988) led by the Hospital Pharmacists’ Group of the Royal Pharmaceutical
Society www.rpsgb.org.uk/pdfs/safsechandmeds.pdf
Social Care
Policy and Innovation (System Reform), 06/2007 “The National
Framework for NHS Continuing Healthcare and NHS Funded Nursing Care”,
DH, www.dh.gov.uk/publications
Social Care Policy and Innovation (System
Reform), 09/2007, “NHS
Continuing Healthcare Checklist”, DH, www.dh.gov.uk/publications
Social Care Policy and Innovation (System Reform), 10/2007, “Decision
Support Tool for NHS Continuing Healthcare”, DH, www.dh.gov.uk/publications
Discharge and Home of Choice Policy September 2010
113 of 114
Acknowledgments
This policy was written with contributions from:
Dr John Billet, Consultant, Elderly Care Medicine
Kay Gilbey, Associate Director of Nursing, MBUHT
Lisa Drake, Commissioner, Copeland Locality
Dave Eldon, Cumbria Partnership
Mary Carruthers, Matron, CIC
Pamela Mason, Matron, South Lakes Hospitals
Diana Hatton, Matron , Acute Service, FGH
Tanya Holmes, Matron, Emergency Services, FGH
Mark Hulmes, Divisional Senior Nurse, WGH
Emily Griffiths, Clinical Lead, Community Services, South Cumbria
Clare Gorman, General Manager, Elderly Care, Stroke, Rehabilitation
Cheryl Page, County Manager, Adult Social Care
Paul Bridle, Adult Social Care, South Lakes Hospitals
Anne Harrison, Adult Social Care, Manager, WCH Social Work Team
Tony Evans, Adult Social Care, CIC
Andrea Loudon, Head Medicines Management, NHS Cumbria
Mel Bradley, Pharmacist, NHS Cumbria
Val Ogilvie, Matron, HMP Haverigg
Janet Ferguson, Cumbria Palliative Care Lead, NHS Cumbria
Jane Hartwell, Macmillan Clinical Nursing Service, CIC
Deborah Bullock, Northwest Ambulance Service, Cumbria
Beth Toomey, Community Matron, Copeland
Lynne O’Neill, Administrator, Carlisle Locality
Alison Graham, Community Matron, Copeland
Aline Parkes, Transition Lead- Cumbria Intermediate Care Services
Meryl Taylor, Eden Locality Manager, Learning Disabilities
Sue Turner, Integrated Services, Senior Clinical Lead
Janet Lancaster, Community Liaison Sister, WCH
Lorraine Dixon, Community Liaison Sister, WCH
Lyn Moore, Clinical Service Manager, Children
Janet Porthouse, NHS Continuing Healthcare Team
Jo Cloudsdale, Matron, Wigton/Brampton Community Hospital
Johnette Irving, Nurse Development Lead, NHS Cumbria
Discharge and Home of Choice Policy September 2010
114 of 114