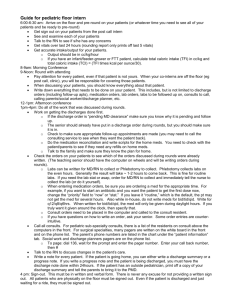
Discharge Planning Policy - Portsmouth Hospitals Trust
advertisement

Discharge Planning Policy Version 8.1 Name of responsible (ratifying) committee Patient Safety Working Group Date ratified 16 February 2012 Document Manager (job title) Matron for Discharge Services Date issued 27 February 2012 Review date 01 July 2015 Electronic location Management Policies Related Procedural Documents See Section 8 Key Words (to aid with searching) Simple Discharge Policy; Discharge Planning; Leaving Hospital Policy; Going Home Policy; Patient discharge; Interagency relations; Patient transport services; Home care of patient; Primary care teams; Pharmacy; Occupational therapy; Physiotherapy; Speech and language therapy; Social services; Nutrition; Dietetics; District nurse services; Clinically Stable Discharge Read; PDD; CDT; IDB Version Tracking Version Date Ratified 8.1 03.02.2015 Brief Summary of Changes Author Minor changes and extension of review date R Davies Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 1 of 21 CONTENTS INTRODUCTION ................................................................................................................................ 3 PURPOSE .......................................................................................................................................... 3 SCOPE ............................................................................................................................................... 3 DEFINITIONS ..................................................................................................................................... 3 DUTIES AND RESPONSIBILITIES ..................................................................................................... 5 This should be used in conjunction with the Safer Bundle which each CSC has agreed to, please refer to Appendix D. ..................................................................................................................... 5 Complex Discharges .................................................................................................................. 11 1.1. Rapid Discharge ................................................................................................................ 13 1.2. Self Discharge ................................................................................................................... 13 1.3. Discharge from Children’s In-Patient Areas ....................................................................... 13 1.4. Discharges from Day Surgery ............................................................................................ 14 1.4.1. Physical Assessment Criteria ............................................................................... 14 1.4.2. Documentation to be provided to the patient/relative/carer ................................... 14 TRAINING......................................................................................................................................... 15 REFERENCES AND ASSOCIATED DOCUMENTATION ................................................................. 15 EQUALITY IMPACT STATEMENT ................................................................................................... 16 MONITORING COMPLIANCE .......................................................................................................... 17 Appendix A ....................................................................................................................................... 18 Discharge Checklist .......................................................................................................................... 18 Appendix B ....................................................................................................................................... 19 List of Documentation to Accompany Patient on Discharge .............................................................. 19 Appendix C……………………………………………………………………………………………………..20 The Discharge and Transfer Planning Process for Simple and Complex Discharges………………20 Appendix D…………………………………………………………………………………………………..21 10-Step Plan………………………………………………………………………………………………….21 Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 2 of 21 INTRODUCTION Portsmouth Hospitals NHS Trust (the Trust) recognises that to facilitate a smooth discharge from care in hospital to care in the community, the discharge plan must be well defined, prepared and agreed with each individual patient. To allow sufficient time for suitable and safe arrangements to be made, discharge planning should begin on admission, or at pre-admission clinics, with a predicted date of discharge being identified within 48 hours of admission and communicated to patients and, if appropriate, their carers/relatives. This policy is written in accordance with the NHS and Community Care Act 93/98, the Department of Health Discharge from Hospital: Pathways, Process and Practice 2003, The Community Care Act (Delayed Discharges) 2003, NHS Continuing Care 2004 and Achieving Simple, Timely Discharge from Hospital 2004 (refer to Section 8). ‘Ready to go?’ - Department of Health, 2010 and Transforming Social Care – Department of Health, 2008 The principles of discharge apply to all patients who have stayed, for however long, in the Trust. However, there are some departments such as the Children’s unit that have specific processes. PURPOSE The purpose of this policy is to set out the process requirements and staff responsibilities to support well-organised, safe and timely discharge for all patients. It aims to fully involve patients and their carers/relatives in the discharge process and ensure that patients receive appropriate assessment, planning and information about their discharge and after care. SCOPE Patient discharge must be seen as an interdisciplinary and/or multidisciplinary issue. Therefore, this policy applies to all permanent, locum, agency and bank staff of Portsmouth Hospitals NHS Trust and the MDHU (Portsmouth), including doctors, nurses, allied health professionals, social care professionals and managers. Whilst the policy outlines how the Trust will manage effective discharge implementation it does not replace the personal responsibilities of staff with regard to issues of professional accountability for governance. Recognising that discharge should be working on a “7 day” system. It is expected that most discharges will take place between the hours of 09.00 and 19.00, however in some circumstances a discharge may take place outside of these times. This is usually self discharges and some end of life care discharges. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ DEFINITIONS Simple discharge: Patients with simple discharge needs make up at least 80% of all discharges. They are defined as patients who: - will usually be discharged to their own home - have simple ongoing care needs which do not require complex planning and delivery. Many of these patients will be discharged from medical assessment units, short stay wards, or even A&E itself as well as medical and surgical wards. Time in hospital does not Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 3 of 21 determine whether a patient has simple discharge needs. The key criterion is the level of ongoing care required – and therefore the complexity/simplicity of the discharge arrangements. Complex discharge: The remaining patients in hospital who have more complex needs ( approximately 20% ) require referral for assessment by other members of the multidisciplinary team. Complex discharges relate to patients: - who will be discharged home or to a carer’s home, or to intermediate care, or to a nursing or residential care home, and - who have complex ongoing health and social care needs which require detailed assessment, planning, and delivery by the multi-professional team and multi-agency working, and whose length of stay in hospital is more difficult to predict Please refer to Appendix C for information on simple and complex discharges. NHS Continuing Health Care (CHC) Consideration for NHS CHC Funding will need to determined for health care requirements on discharge for all patients with rapidly deteriorating health problems. Consent and a CHC checklist is completed when a person is medically fit for discharge and have reached their optimum level. The consideration for eligibility for continuing healthcare and NHS funded care needs to form part of the discharge planning in line with requirements in the National Framework (revised November 2012). It is essential that patients, their families and/or carers are fully engaged throughout the process according to best practice as stated in CHC National Framework. Full assessment for CHC. Using the DOH Decision Support Tool (DST) will be completed prior to discharge however this should ideally not take place in the acute setting. The patient should be transferred to an alternative setting for the assessment to be completed. There are continuing care assessments beds available for both Hampshire and Portsmouth, were the assessment can take place in a more suitable environment – should the client have no challenging non compliant behaviours. Patients with an End of Life Care Plan This applies to patients with specialist palliative care needs, however input may be from a single or multi-disciplinary team depending upon the place of discharge. Specialist advice may be required to ensure prompt access to and availability of equipment or services. An estimated date of discharge is not used for palliative care, these patients who have been admitted as part of for end of life care and management. Where the patient’s condition is rapidly deteriorating, the responsible clinician for the patient can use the DoH Fast Track tool to provide evidence to support rapid response to care needs in the community. Patients can be discharged to existing community services not provided through CHC for end of life care support. Discharge Lounge Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 4 of 21 Non-ward environment on both Trust sites which accommodates patients prior to leaving hospital, where care needs can be completed and any communications regarding discharge can be actioned. Please refer to the Discharge Lounge Standard Operating Procedures for more detailed information on the process. Rapid discharge and transfers to community hospitals and care homes: may be simple or complex and usually as a result of pressures to place patients in appropriate care environments as a result of the escalation process. Predicted [Planned] Discharge Date - PDD: a target discharge date to which all agencies can work whilst recognising that the date may change according to the patients needs/clinical status Self discharge: related to patients wishing to self discharge against medical advice ‘To Take Out’ Medicines (TTOs): medicines which the patients take away when they leave hospital Out of Hours Discharge: a discharge that takes place after 1700hrs and before 0800hrs Monday to Sunday DUTIES AND RESPONSIBILITIES This should be used in conjunction with the Safer Bundle which each CSC has agreed to, please refer to Appendix D. Medical Staff The consultant or other appropriate doctor with delegated authority has responsibility for: Please refer to appendix D for the 10 Step Plan. Determining a planned discharge date (PDD) that is communicated to the patient, relatives/carer on admission and recorded in the patient’s notes and on the board within the ward area. ALL patients to have a PDD based on medical and functional suitability for discharge The PDD must be realistic and set within 24 hours of admission Decision Maker review of patients following Board Round SICKEST patients first THEN potential discharges THEN new patients THEN ward round of remaining patients Ensuring that the Patient Journey Board is updated and agreed post consent of the patient and relative details being incorporated in this format Confirming the PDD on the first senior clinical review and ensuring that date is communicated to the multi-disciplinary team (MDT), the patient and their relatives/ carers in relation to Section 2’s for relevant OT or ASC needs. Keeping the patients/relatives/carers fully informed of their progress and treatment in order to progress assessment needs. Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 5 of 21 Liaising with the MDT on a regular basis to enable co-ordination of the agreed discharge date. Ensuring any change in the patient’s PDD is communicated to the MDT/patients/relatives and recorded in the medical notes without delay. Documenting clearly in the medical notes when a patient is medically fit for transfer. Pharmacy Ensuring all TTO medication is prescribed at least 24 hours before discharge. Ward Pharmacist to be informed of any changes immediately, and patients with NOMADs to be identified earlier if possible Patients transferring under End of Life (with an End of Life care plan) should have anticipatory medications written and dispensed accordingly. Patients with a syringe driver should have the pump logged with the hospital equipment library or MOPRS End of Life Team for return and ensure that the process for return is followed (Large addressed padded envelope with instructions to be sent with pump) and that medical engineering are aware of this for return. Ensuring that when a patient is to be discharged with medication prescribed via injection or an infusion pump an authorisation letter is written to the district nurse confirming details of the prescribed medication to accompany the patient on discharge. Completing medical summary of treatment/ medical management plan for on-going care needs for patients transferred to community hospital, care home or social care facility recognising the Electronic Discharge Summary should be completed if unable and a hand written then to ensure concise and legible. Ensuring the General Practitioner receives a written Discharge Summary within 24 hours of discharge. This should be legible i.e. printed or electronic and contain the following information as a minimum: - Initial reason for admission List of investigations carried out and all available results Summary of procedures/treatment carried out during current stay in hospital If necessary, the summary should also include Definitive primary diagnosis or reason for not being available Medication commenced and to be continued following discharge, including duration Medication changed or stopped, including reason Management plan post discharge Escalation plan, if problems occur (i.e. who to contact) If using AMBER Care bundle in hospital suggest use of EPaCCS register and/or Gold Standards Framework in the community. - Current follow up arrangements - Recognising the Electronic Discharge Summary should be completed if unable due to IT breakdown then a hand written should be legible on all copies provided. Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 6 of 21 Providing a further discharge summary to be sent to the General Practitioner within 10 working days if the preliminary letter has been handwritten or the GP needs to be informed of additional information (e.g. test results received post discharge). Issuing a sickness certificate for any anticipated period of incapacity. Reviewing the Do Not Attempt Cardiopulmonary Resuscitation (DNACPR). If a DNACPR decision is to remain in situ/valid on discharge then the doctor (Grade ST3 or above) must discuss this decision and the implications, with the patient or, if they lack capacity, the patients relative/ advocate and/or main carer. Senior Nurse /Nurse in Charge has overall responsibility for: Ensuring that all patients have a PDD recorded in their notes, detailed on the Visible Ward Board and that this date has been communicated to the patient, relatives/carer, as appropriate. Ensuring that systems are in place so that patient discharge is co-ordinated and progresses according to plan. Ensuring that information required to plan and manage patient discharges is gathered, and recorded accurately, especially in respect of conversations with the patient, their family and/or carers: including the date and times of those conversations Continuously monitoring the discharge progress of all patients and, if necessary, ensure positive action is taken to expedite discharges for those who are medically fit and have exceeded their PDD. Any delays to patient progress (diagnostics, tertiary opinion, ASCOT) to be reviewed and escalated as per CSC pathway ie through Matron or General Manager Ensuring the collection and submission of weekly delayed transfers of care monitoring information Ward Nurse is responsible for: Discharge planning commences within 24 hours of admission and that progress is appropriate to achieve the PDD. The patient and relatives / carers are fully involved in the discharge planning process, their needs and wishes are taken into account and they have at least 24 hours notices of the discharge date, whenever possible Patients with complex needs are referred to the Integrated Discharge Bureau (IDB) as early as possible Prompt referrals to the relevant agencies are made, using the appropriate referral criteria and documentation and if the discharge is complex, giving the district nurse / care home staff the opportunity to attend the ward to discuss and organise a package of care. Consideration of the need for continuing health care assessment for all patients with ongoing care needs before referral to Social Services using the continuing care check list located in the discharge planner. The patient’s medication is ordered 24 hours before the discharge Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 7 of 21 Appropriate transport arrangements are made and that all pertinent information regarding the patient’s condition is given to the ambulance service transporting patients. (e.g. Do Not Resuscitate [DNAR] status, infections, issues regarding transferring and in respect to manual handling). When arranging transport for discharge it is vital that the discharge address including Post Code is confirmed and checked as correct, as it may differ to the patient's home address. It is equally important to check that the patient can access their destination address e.g. do they have a key, can they manage any steps at the property. Transport should be made via the On-Line Transport system through the current provider. Transport should only be provided for discharge when there are no family or friends to transport. Transport can be booked 24/7 and all staff should access this system to book accordingly to the patients needs and mobility status. If your patient is not eligible you will be signposted to a directory of alternative transport. . The receiving hospital, care home or social care facility (or community nurse team, if the patient is returning home) is notified of any known infection and the current infection control practices in place e.g. antibiotic therapy, dressing regime, barrier nursing. The patient has the necessary medication, dressings and relevant information about post discharge care. All arrangements and referrals in relation to discharge planning are clearly documented, signed and dated within the discharge planning documentation All healthcare professionals involved with the patient are notified of any change in the patient’s ward placement and or condition/suitability for discharge with a request for a review as appropriate. To improve the quality of patient admission, discharge and transfer between health and social care providers PHT have signed up to 10 Standards which fits with the CQUIN targets as well as other markers. Local of seamless care – improving patients safety and experience at admission, transfer and discharge (ADT) across the Portsmouth and South East Hampshire area. The targets are: Person Centred Approach The process of Interprofessional – inter organisational handover Written and verbal communication Care Plans Record Keeping Risk Management Safeguarding Whole Systems /Partnership working Managing and learning from Incidents Transport and Escort Special Considerations To ensure all Healthcare Professionals are involved ensure the standards are recorded within the relevant document and completed. Current documents are not inclusive of standards as PHT to revalidate current documents which area in line with NMC and professional standards. Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 8 of 21 Any potential delays in discharge are referred immediately to the IDB as soon as they become known outlining the reasons for the delay or potential delay. A Discharge Summary is completed by medical staff and sent to the GP within 24 hours All necessary information for discharge/transfer of care and management is gathered, recorded and communicated appropriately Integrated Discharge Bureau [IDB] will: Coordinate, monitor and ensure patients are discharged from Portsmouth Hospital safely, as far as possible, in line with their planned discharge date [PDD] Provide specialist advice and support, including signposting to other specialist services, to all ward and MDT staff on complex hospital discharges Act as a point of contact for colleagues within community hospitals, primary care, social services and voluntary agencies in relation to people with complex discharge packages or concerns related to the hospitals discharge procedure and process. Facilitate and support staff with discharge planning of patients whose care is being provided on outlying wards Maintain a list of all patients that have - Been in hospital for longer than 14 days Have just been declared medically fit Have been flagged by the ward/discharge MDT as being complex and potentially requiring the assistance of the Discharge Planning Team Monitor progress and advise on the discharge process including identifying and reporting the reasons for any delayed discharges. Monitor, progress, advise and provide training to the organisation in regard to discharge systems and processes including monitoring and reporting all Delayed Transfer of Care [DTOC] issues to local commissioners/ Strategic Health Authority. Discharge Planning Team [DPT] will: Provide specialist advice and support to wards and the multidisciplinary team on complex hospital discharges. Act as a point of contact for colleagues within community hospitals, primary care, social services and voluntary agencies in relation to people with complex discharge packages or concerns related to the hospitals discharge procedure and process. Provide informal and formal teaching and education packages to members of the multidisciplinary team on current issues relating to discharge planning Maintain an up to date database on staff trained to undertake continuing care and funded nursing care assessments. Facilitate the CHC Fast Track discharge process ensuring that patients, who have been identified by a hospital clinician that they are in a terminal phase with a rapidly deteriorating condition, an increased dependency and who have expressed a desire to die at home, are processed immediately and given a facilitated discharge involving MDT, community health and social care rapid response teams, as required [NB: CHC Fast Track Process for Hampshire has changed – refer to DPT intranet site]. Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 9 of 21 Infection Prevention and Control will provide ward staff with additional infection prevention and control advice/input as required, including for those patients who are being transferred or discharged to another facility, including to home Note: if MRSA screening is required before transfer to another healthcare provider, (e.g. transfer to an alternative hospital for specialised treatment) staff should be aware that it could take up to 3 working days for results to be obtained. Further information regarding patients with MRSA, Vancomycin Resistent Enterococci (VRE), CDIFF can be found on the Infection Prevention and Control departmental website Continence Service will provide advice, support and education to wards on all aspects of continence care: addressing such issues in a timely manner will support appropriate discharge. Reasons for referral include: Reversible causes of bladder problems that have been addressed on the ward Bladder problems e.g. urgency, frequency, straining etc. Urinary and/or faecal incontinence Urinary catheter, indwelling or intermittent self catheters (ISC), is causing significant problems. Bladder and/or bowel diary commenced Frailty Pathway A Consultant Geriatrician and Older Persons Nurse Specialist will be present on the AMU 8am-12 365 days per year. Frail patients should be allocated to the Geriatricians Post take ward round list, and will then be reviewed by the Geriatrician and OPNS. The Geriatrician and OPNS will liaise with on-site community matrons, Integrated Discharge Bureau and OPMH Liaison Team, Therapy and Social Services staff regarding the implementation of a community response to support the patient back out of hospital into a community setting, if appropriate, and in preference to a hospital admission. They may make an onward referral to a community virtual ward if needed. Advise relatives/carers of patient condition and capabilities and to recommend action in support of the patient’s current condition Facilitate rapid access to out patient assessment and diagnostic clinics and, when appropriate, in preference to a hospital admission Community Discharge Team The team came into post October 2013 under CQUIN initiative. The role of In-reach Team will be to support and facilitate the safe and timely discharge of patients back out into a community setting. Individual patient discharge, whether simple or complex, remains the responsibility of ward staff to coordinate and expedite. Ensure that patients with likely complex needs on discharge are identified on admission. This includes pursuing discussions with patient and families as early as possible in their treatment pathway regarding likely needs on discharge so that patients experience a minimal delay once identified as clinically stable by Portsmouth Hospital’s clinical teams. Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 10 of 21 Provide background information to wards on the known clinical and social history of the patient and as it relates to discharge from hospital. Provide daily support to ward teams around the planning and undertaking of effective and safe discharge planning Referral Pathways The Community Discharge Team will work with elderly patients with complex needs for discharge and will case manage certain patients out of hospital – where it appropriate for them to do so. However, ward staff will retain responsibility for coordinating all internal discharge planning activities including setting EDD’s, drafting TTO scripts, producing Discharge Summaries, daily liaison with families regarding progress, booking transport and coordinating internal transfers to Discharge Lounge Patient referrals to Community Discharge will be via several routes. a) Individual members of the Community Discharge Liaison Team will attend daily whiteboard rounds to identify patients that are both complex and likely to require community in-reach assistance and planning to leave hospital. They will contribute to the setting of the Expected Discharge Date for all patients on the ward and will prioritise their activities to ensure patients are able to safely leave hospital on that date. b) From the Hospitals PTL - Patient Transfer List [IDB list] complex elderly patients will be identified for community in-reach support as they have recently been flagged as clinically stable by the ward via the green cross notification procedure. This process will capture complex frail elderly patients who may have been outlied from MOPRS recently or are currently under the care of AN Other specialty c) Patients specifically referred to either service by ward staff via bleep or telephone to hub offices. NB: Ward referrals for patient review the OPMH Liaison Team should be faxed to Ext 6591 [02392 286591 - if faxing from outside the hospital] Complex Discharges The health professional coordinating the discharge must ensure all points relating to complex discharges have been considered, as follows: The Discharge Planning Team should normally be involved in the discharge of complex patients and can provide expert advice to ward/ staff and department managers to: Assist ward staff in the identification of patients with ongoing care needs. Support ward staff in assessment of patient discharge needs and assist ward staff in making alternative discharge plans, as appropriate - Advise ward staff about suitability for and availability of Community Hospital beds - Advise ward staff about eligibility and process for accessing Continuing Health Care funding - Provide an ongoing programme of education around CHC matters for ward/department staff. - The patient and home carer (including informal carers) must be central to the Discharge Plan. They must be kept informed of progress on a regular basis by all Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 11 of 21 members of the multidisciplinary team (MDT). Where appropriate the patient and carers will be invited to attend multidisciplinary meetings, discharge planning and case conferences. Any concerns regarding a possible Vulnerable Adult, must be advised to the senior nurse on duty. Any concerns regarding a patient with mental health needs or learning disabilities must be taken into account and the discharge planning process must involve the appropriate specialists, to ensure the discharge is appropriate and that the patient is discharged to the right environment for their safety and on-going care needs If the patient has been deemed not to have capacity following a capacity assessment (refer to the Mental Capacity Act 2005 or Consent policy) a referral to an Independent Mental Capacity Advocate (IMCA) 12 should be considered before making any discharge plans. When patients are transferred to a community hospital/ care home the nurse in charge of discharge must ensure: - - All notes and X-rays are sent with the patient if they are being transferred to a Community Hospital or photocopied notes if they are being transferred to a hospital out of area. Care homes should not receive medical notes. The doctor caring for the patient must complete a medical transfer letter and document in the notes that the patient is fit for discharge. The nurse in charge of discharge should complete and send a nursing transfer letter. The community hospital or care home should be contacted and be given a full handover prior to discharge. A record of what each Hospital requires with the notes and drug charts Transport should be arranged at the earliest opportunity, with the aim that the patient will arrive at their destination no later than 1400hrs on the day of discharge Staff must ensure that information about infections and any particular care needs related to those infections and their control are communicated when a patient moves to the care of another organisation, e.g. community nurse, GP, nursing home or community hospital. This information should include: MRSA status and whether the patent is currently receiving decolonisation treatment - The date of the next MRSA screen - Contact with other patients with known or suspected infections - Any recent history of diarrhoea and/vomiting - Communication with care providers must be documented in the patient’s health records and the Discharge summary must highlight any infection risks and associated care needs. 1 2 Independent Mental Capacity Advocacy [IMCA] - Role IMCA Referral Form Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 12 of 21 1.1. Rapid Discharge Rapid discharge3 should only occur when it is essential to discharge a patient urgently to prevent a bed crises and to achieve emergency care standards. Rapid discharges will be directed by the Business Executive, the Operations Centre Manager or the Hospital Duty Manager When rapid discharges are necessary the nurse in charge of discharge must ensure a safe discharge, by ensuring all of the criteria for simple and/or complex discharges are met Rapid discharge must not occur as a result of poor discharge planning 1.2. Self Discharge Patients may decide to discharge themselves from the hospital against clinical advice. If a patient wishes to self discharge: Staff must advise the patient why it is in their best interest to remain in hospital; The doctor on duty must be informed; The doctor on duty must inform their consultant as soon as possible; Any medication required on discharge must be provided. If the patient refuses to wait for their medication then all reasonable steps must be taken to ensure that the patient receives it, e.g. using a courier service to deliver the medications to their domiciliary residence Relatives and Social Services must be contacted, if relevant; The patients GP must be contacted at the time the patient leaves the hospital; A discharge summary must be sent to the GP within 48 hours of the patient leaving hospital; All actions and discussions must be recorded, dated, timed and signed in the patient’s health records. 1.3. Discharge from Children’s In-Patient Areas Children are only ever admitted to hospital if the care they require cannot be delivered in the community. They are discharged from in-patient care at the first possible opportunity at which community services and their families are able to manage any ongoing care required. Preparation for discharge often includes significant levels of education to accommodate care being continued in the community by a child’s care givers. Discharge planning must begin on admission with a multi-professional and family involvement focus, to ensure all needs are met. The focus of discharge planning is always that the safety and developmental needs of the child are maintained on discharge, supported by and giving support to, those whom they live. The general processes of the Trust apply equally to children as to adults. However, specific community services exist for the support of children requiring ongoing care. These include: - 3 Community children’s services – medical and developmental Peripatetic and school based education services Children’s and adolescent mental health services Health visiting Community Children’s Nursing Team Discharge Lounge – Major Incident Plan Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 13 of 21 - Community Dental Children’s services Social Services Children’s Team Tertiary units and community staff It is essential that Communications with all relevant services is documented. Discharge can only be facilitated once there is agreement of the multi-professional team that the child is medically fit for discharge and that their ongoing needs can be met in the community. Having achieved such agreement, nurse facilitated discharge is acceptable except in cases of children for whom there are Safeguarding concerns. Children for whom there are Safeguarding concerns can only be discharged by the Paediatric Consultant responsible for the child’s episode of care, or the consultant’s paediatric registrar. A decision to discharge the child must be documented in the child’s medical and nursing notes, along with any plan for follow-up after discharge. This is in line with the Laming recommendations 2002. When children are discharged, particularly if they have undergone an operation, it is important that the parents, carers or guardians are aware of what they can expect when the child gets home. To ensure the parents, carers, guardians are fully informed a number of leaflets are provided on discharge. 1.4. Discharges from Day Surgery To achieve a high-quality service discharge planning in day surgery should begin before the adult or child is admitted to the unit. Pre-operative assessment has become essential to the development of day surgery planning. For children and adults alike it provides an opportunity to discuss the patient’s needs and to address any fears or anxieties of the patient, family or carer. Discharge planning must embrace physical, psychological and social aspects of individual patient care. This framework can then be used to develop guidelines for patient discharge following day surgery Discharge criteria should be relevant to the aims and objectives of each individual unit. However, the following aspects must always be assessed when developing discharge criteria for both adult and paediatric patients, irrespective of who takes responsibility for this. 1.4.1. Physical Assessment Criteria Conscious level should be consistent with pre-operative state Cardiovascular and respiratory assessments should be stable Alimentary – input and output assessment should be undertaken Patients should be conscious and orientated Pain, nausea and vomiting should be minimal and controlled Wound site – surgical bleeding should be minimal, i.e. not requiring a dressing change Mobility of the patient – patient should be able to walk at a pre-operative level. 1.4.2. Documentation to be provided to the patient/relative/carer Information, both verbal and written, about the patient’s recovery at home in relation to their procedure: the patient’s and the parent’s/carer’s level of understanding should be checked Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 14 of 21 Information about any required follow-up appointments must be provided Any required medication to take home must be provided and any required support and guidance on administration Contact telephone for emergency and continuing care Copy of the discharge summary TRAINING The Discharge Planning Team provides a monthly programme of education for ward/department staff on discharge Continuing Health Care – systems and processes. This is part of the PHT training plan with Learning and Development incorporated within the setting direction and patient safety day. Discharge planning training is provided to all relevant new staff as part of the hospital’s induction processes as part of setting direction. The discharge Competency is part if the generic competencies to be completed by all staff working at PHT REFERENCES AND ASSOCIATED DOCUMENTATION http://www.england.nhs.uk/ourwork/part-rel/transformation-fund/bcf-plan/ External Ready to go? - Department of Health, 2010. Transforming Social Care - Department of Health, 2008. Local Authority circular LAC (DH)(2009) 1 - Department of Health, 2009. User-led Organisations Project Policy - Department of Health, 2007. Urgent Care Pathway for Older People with Complex Needs - Best practice guidelines. Department of Health, 2007. Carers (Equal Opportunities) Act 2004. Office of Public Sector Information. Implementation of Direction of Choice of Accommodation Achieving timely "simple" discharge from hospital - Department of Health, 2004, Supporting people with long term conditions - Department of Health, 2005. Discharge from Hospital: Pathway Process and Practice: Department of Health (2003) Active Timely ‘Simple’ Discharge from Hospital – A Toolkit for the Multidisciplinary Team: Department of Health Ensuring the Effective Discharge of Older Patients from NHS Acute Hospitals. The National Audit Office Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 15 of 21 Ready to Go? : Dept of Health Internal Patient Identity Policy Discharge Planning Team [intranet site] Transfer Policy Standard operating procedure for safe patient use of the discharge lounge 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly. Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 16 of 21 10. MONITORING COMPLIANCE As a minimum the following elements will be monitored, to ensure compliance Minimum requirement to be monitored Lead Tool Discharge requirements which are specific and relevant for each patient group: 100% of discharge requirements met Patient Experience of discharge: 100% of user surveys demonstrate a positive response to discharge arrangements Quality of documentation and information provided to patients on discharge from PHT: 100% of patients have appropriately completed documentation Senior Nurse – Discharge Services Audit of discharge planning documentation completed by ward staff in individual patient records Telephone survey of random inpatients within 1 week of discharge Process for discharge out of hours followed in 100% of cases Senior Nurse – Discharge Services Senior Nurse – Discharge Services Senior Nurse – Discharge Services Audit of documentation for patients leaving hospital via the Discharge Lounge Review of discharge check lists to ensure process followed to include evidence of dialogue with Community Support Teams Patient Transport Service conveyance log Frequency of Report of Compliance Annually Reporting arrangements Lead(s) for Acting on recommendations Policy Audit Report to: Nursing and Midwifery Advisory Committee CSC Heads of Nursing / Senior Nurse – Discharge Services Annually Policy Audit Report to: Nursing and Midwifery Advisory Committee CSC Heads of Nursing / Senior Nurse – Discharge Services Annually Policy Audit Report to: Nursing and Midwifery Advisory Committee CSC Heads of Nursing / Senior Nurse – Discharge Services Annually Policy Audit Report to: Nursing and Midwifery Advisory Committee CSC Heads of Nursing / Senior Nurse – Discharge Services . Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 17 of 21 Appendix A Discharge Checklist Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 18 of 21 Appendix B List of Documentation to Accompany Patient on Discharge PHT ‘Leaving Hospital’ leaflet If patient leaving hospital via Discharge Lounge – PHT Discharge Lounge - Patient Leaflet X2 copy of (Electronic) Discharge Summary Patient Discharge Information sheet (refer Appendix C) Care plan – if ongoing treatment/care will be required post discharge Nurse Transfer of Care letter (if going to Residential or Nursing Home) If the patient is employed - the patient may require a sick certificate. A MED10 certificate stating the patient has been an inpatient may be completed by the nursing staff coordinating the discharge. The medical/surgical team will need to complete a MED3 certificate if the patient requires time off after their hospital admission. A validated on discharge DNACPR agreement – if appropriate PHT Residential Placement Information leaflet– for >65 patient who are either: o awaiting placement o leaving hospital to complete Continuing Health Care application process o leaving hospital to wait elsewhere for a vacancy to arise in nursing home of choice Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 19 of 21 Appendix C Ready to Go? – Department of Health, 2010 Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 20 of 21 Appendix D 10 Step Plan Ready to Go? – Department of Health, 2010 Discharge Planning Policy Version: 8.1 Issue Date: 27 February 2012 Review Date: 01 July 2015 (unless requirements change) Page 21 of 21