to open the MS Word version of the Quarterly Action Agenda
advertisement

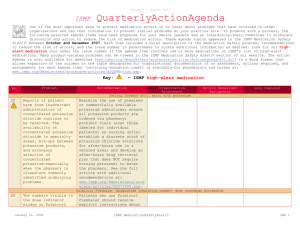
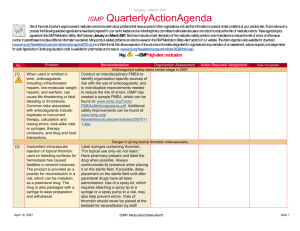
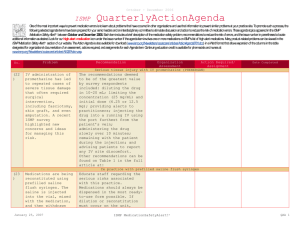
July – September 2015 ISMP QuarterlyActionAgenda One of the most important ways to prevent medication errors is to learn about problems that have occurred in other organizations and to use that information to prevent similar problems at your practice site. To promote such a process, the following selected items from the July—September 2015 issues of the ISMP Medication Safety Alert! have been prepared for an interdisciplinary committee to stimulate discussion and action to reduce the risk of medication errors. Each item includes a brief description of the medication safety problem, a few recommendations to reduce the risk of errors, and the issue number to locate additional information as desired. Look for our high-alert medication icon under the issue number if the agenda item involves one or more medications on the ISMP List of High-Alert Medications (www.ismp.org/sc?id=479). The Action Agenda is also available for download in a Microsoft Word format (www.ismp.org/newsletters/acutecare/articles/Action Agenda1504.doc) that allows expansion of the columns in the table designated for organizational documentation of an assessment, actions required, and assignments for each agenda item. Continuing education credit is available for nurses at: www.ismp.org/sc?id=480. Key: Problem No. —ISMP high-alert medication Recommendation Organization Assessment Action Required/ Assignment Date Completed Pediatric medication safety survey shows improvements still needed (11, 13) (13) Survey respondents reported low implementation with storing adult, pediatric, and neonatal medications separately; prescribing liquid medications in metric doses; verifying line attachment before administering infusions; requiring practitioners to undergo specialized training and competency validation when working with pediatric patients; and barcode scanning breast milk to match the infant with the mother’s milk prior to feeding. Only 41% of pediatric hospitals, 43% of adultpediatric hospitals, and 19% of outpatient facilities require verifying the components of sterile preparations prior to adding them to a solution. Survey results indicate that improvements are still needed to adequately protect pediatric patients from harmful medication errors. Healthcare providers caring for pediatric patients should assess their current practices and develop a plan to improve implementation of the recommended “best practices” in the survey. NAN Alert: Medication cups with more than one dosing scale can lead to confusion A nurse confused two dosing scales on a Ideally, oral syringes that measure only plastic medication cup and administered 1 in mL should be used for oral liquid dram (3.7 mL) instead of the intended 1 mL medications instead of cups. If a dosing dose of morphine sulfate 20 mg/mL oral cup must be used, it should only solution, resulting in a fatal overdose. measure in mL. Until these cups are widely available, some suppliers can customize the cups to measure in mL October 8, 2015 ISMP MedicationSafetyAlert! QAA 1 July – September 2015 ISMP Problem No. QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed only. (13) (14) Ongoing BLOXIVERZ (neostigmine) and VAZCULEP (phenylephrine) confusion Ongoing reports of potentially harmful Make pharmacy and OR/anesthesia mix-ups between look-alike vials of staff aware of the potential for errors Bloxiverz 10 mg/10 mL and pharmacy bulk with these products. Pharmacy bulk packages of Vazculep 50 mg/ 5 mL have packages of Vazculep should never been received. Most recently, a Vazcu-lep leave the pharmacy. Soon, Éclat 50 mg vial was sent to the operating room Pharma-ceuticals will be packaging (OR)/anesthesia instead of Bloxiverz. If 5 Vazculep in a box with “Pharmacy Bulk mL of Vazculep (50 mg) had been Package” highlighted in a yellow injected, believing it was Bloxiverz, the background and the strength massive overdose could have caused highlighted in gold. For now, the extreme hypertension, cerebral vascular company is supplying alert stickers to accident, or death. add to current stock to help staff recognize the potential for mix-ups. Name and dosing confusion between mefloquine and MALARONE (atovaquone/proguanil) Mix-ups have been reported between Include the brand and generic names mefloquine and Malarone. Both are used for when prescribing Malarone, and include malaria treatment or prophylaxis and are the purpose (e.g., malaria prophylaxis or available in 250 mg tablet strengths. treatment) when prescribing either drug. Mefloquine was prescribed daily instead of Confirm the drug, frequency of weekly, and mefloquine was mistaken as administration, and dose regimen with the generic name for Malarone and each order. In order entry systems, dispensed in error. These mistakes could establish an alert that will appear if lead to vomiting, syncope, QT prolongation, mefloquine is prescribed daily and if paranoia, and inadequate prophylaxis. Malarone is prescribed weekly. Guidelines for adult IV push medications (14) While the prescribing, preparation, and administration of IV push medications has become exceedingly commonplace as part of a therapeutic standard of care, the lack of oversight and guidance for administration practices has led to October 8, 2015 ISMP held a 2-day summit to address the lack of standardized practices for IV push medications. Draft guidelines were developed and shared on our website for comment. The final Safe Practice Guidelines for Adult IV Push Medications can be found here: ISMP MedicationSafetyAlert! QAA 2 July – September 2015 ISMP Problem No. significant variability, not only among organizations, but within organizations; even among individual clinical units. QuarterlyActionAgenda Recommendation Organization Assessment Action Required/ Assignment Date Completed www.ismp.org/sc?id=563. Review the guidelines to identify the associated risks and consider implementing these safe practices associated with the use of IV push medications. Loss of potency with certain medications prepared in advance in BD syringes (15, 17) (16) (17) Certain medications (e.g., fentaNYL) have been found to lose potency when prepared in BD syringes and not administered shortly thereafter. The rubber syringe stopper in certain lots interacts with these medications causing a loss in potency. The syringes were never approved for use as a storage system for drugs. This calls into question pharmacy or outsourcer preparation of unit dose syringes in advance of anticipated use. Limit drug exposure in plastic syringes by using them promptly after preparation. However, do not sacrifice safety, and ensure that any process changes do not increase the risk of errors. Make clinical staff aware of the situation and to report unexpected changes in drug effectiveness. Assign staff to watch for updated information from FDA, BD, ISMP, ASHP, or other alerts regarding the situation. RELISTOR (methylnaltrexone) prefilled syringes look like enoxaparin and fondaparinux prefilled syringes A Relistor syringe (12 mg/0.6 mL) was Products should remain in their cartons confused with a generic enoxaparin syringe or blister packs until time of (150 mg/1 mL, Amphastar administration, although automated Pharmaceuticals). The same dark navy dispensing cabinet (ADC) drawers don’t color is used with both syringes. There are always provide enough space. Product other similarities between the syringes that barcode scanning prior to dispensing could also contribute to a mix-up. and administration will help identify Enoxaparin syringes (30 mg/ 0.3 mL, Teva) errors. also look similar to fondaparinux syringes (2.5 mg/0.5 mL, Dr. Reddy’s Laboratories). Stocking mix-ups with intracardiac EPINEPHrine and intravenous (IV) EPINEPHrine syringes Hospitals have inadvertently purchased ISMP has requested Hospira to prefilled syringes of EPINEPHrine 1 consider making the word “intracardiac” mg/10 mL intracardiac injection rather more prominent on the label. In the than the IV formulation, leading to meantime, hospitals should have a October 8, 2015 ISMP MedicationSafetyAlert! QAA 3 July – September 2015 ISMP QuarterlyActionAgenda Problem Recommendation stocking errors in code carts, unit stock, and automated dispensing cabinets (ADCs). Suppliers failing to specify “intracardiac” on order lists contributed to the errors, as did a shortage of IV forms of EPINEPHrine. process in place to ensure replacement products ordered during shortages are appropriate. No. (18) Brintellix 10 mg was dispensed instead of the prescribed Brilinta 90 mg. The two medications were stored side-by-side and the wrong container was selected. The patient fell and was admitted to a hospital after taking Brintellix for 9 days. The US Food and Drug Administration (FDA) has also issued a warning about errors, noting over 50 reports have been received. (18) An employee heard a ticking sound from a sharps container in the emergency department (ED). A “suspicious package” code was initiated, and the ED was closed until an Auvi-Q autoinjector was identified as the cause. The device had been brought to the hospital by a patient who had not reattached the outer case after use, which allowed the battery to drain until it emitted a ticking sound as it died out. Organization Assessment Action Required/ Assignment Date Completed Continued BRINTELLIX (vortioxetine) and BRILINTA (ticagrelor) mix-ups Establishing dose limits in order entry systems may help detect mix-ups if 90 mg of Brilinta is ordered but Brintellix is selected. Consider implementing computer alerts to warn about possible confusion. Encourage prescribers to include the medication’s generic and brand name and indication on orders and prescriptions. Store these drugs in separate locations within the pharmacy. Proper disposal of AUVI-Q (EPINEPHrine) autoinjector is critically important (19) Educate healthcare practitioners and patients about the proper use and disposal of the injector after replacing the outer case. Confusion about the ticking sound may cause patients to be diverted to other facilities during investigation of the noise and potentially delay treatment. Avoid using TPA or TNK when referring to ACTIVASE (alteplase) and TNKASE (tenecteplase) The US Food and Drug Administration Never use abbreviations for drug (FDA) continues to receive reports of names, including TPA, t-PA, or TNK. October 8, 2015 ISMP MedicationSafetyAlert! QAA 4 July – September 2015 ISMP QuarterlyActionAgenda Problem Recommendation mix-ups between Activase (alteplase) and TNKase (tenecteplase) due to the use of abbreviations, “t-PA” or “TPA.” Nurses involved in these cases assumed that t-PA was shorthand for TNKase and attributed the errors to confusion between TNK and TPA. Instead, for alteplase and tenecteplase, use the full drug names—brand, generic, or both. Remove the abbreviations from all order sets, order entry screens, and treatment protocols. Prescribers should state the indication with orders to ensure the correct drug is dispensed. No. Organization Assessment Action Required/ Assignment Date Completed Confusion between error-prone abbreviations for tranexamic acid (“TXA”) and tenecteplase (“TNK”) (14) (15) A physician requested “TXA” for a trauma patient who required tranexamic acid (antifibrinolytic). The nurse thought he said “TNK” and gave the physician tenecteplase (thrombolytic) in a syringe. Expecting an infusion, the physician detected the error. If tenecteplase had been given, the patient might have bled. Both tranexamic acid and tenecteplase may be in an automated dispensing cabinet (ADC) in the emergency department and available via override. Do not use abbreviations for any drug name, including “TXA” or “TNK.” Review all forms of communication where these drug names may be listed (e.g., drug information resources, storage bin labels, entries in ADCs and order entry systems) and ensure that an abbreviation for either name is not used. Consider including an alert in order entry systems and ADC databases that states the indications for each drug and requires acknowledgement prior to removal. Engage pharmacy to ensure an independent double check of fluorouracil infusion rates Over-infusion of fluorouracil has often Ensure an independent double check of been caused by accidental programming the infusion rate by engaging the help of of the incorrect infusion rate, often by an pharmacy. Pharmacy can set up the oncology or home care nurse who may pump and program the initial settings, and not have a second healthcare then hand off the pump and medication to professional to verify the settings the nurse, who then independently independently. verifies the patient’s identification and compares what has been ordered against the pump settings entered by the pharmacist. Methylene blue is a monoamine oxidase inhibitor (MAOI) October 8, 2015 ISMP MedicationSafetyAlert! QAA 5 July – September 2015 ISMP Problem Recommendation A patient taking PARoxetine received methylene blue during a procedure due to the unavailability of the marker dye indigo carmine. Methylene blue is a MAOI; as a result of the interaction, the patient required intubation and admission to the intensive care unit. Methylene blue can interact with selective serotonin reuptake inhibitors and serotonin norepinephrine reuptake inhibitors. Facilities should treat methylene blue as a medication and order the drug so it can be verified/entered into the pharmacy computer system to allow potential drug interactions to be identified. Practitioners without order entry systems should incorporate drug interaction checks for methylene blue within existing processes. No. (19) (19) QuarterlyActionAgenda Organization Assessment Action Required/ Assignment Date Completed Bendamustine (TREANDA) incompatible with some closed system transfer devices A component of bendamustine, N,NDetermine if your facility uses a CSTD dimethylacetamide (DMA), is that is incompatible with bendamustine. incompatible with closed system transfer devices (CSTDs) that contain polycarbonate or acrylonitrile butadiene styrene (ABS). PhaSeal, a CSTD, does not contain these components, and after testing, it is confirmed that PhaSeal is compatible with bendamustine. October 8, 2015 ISMP MedicationSafetyAlert! QAA 6