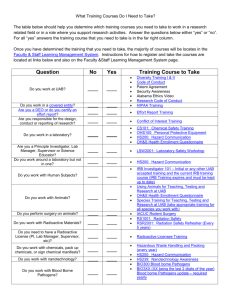
Laboratory Biosafety Manual - OSEH
advertisement

Laboratory Biosafety Manual (BSL Level) Room (Number) Building (Name) Department (Name) PI/Lab Director (Name) Revised by OSEH 2/14/2013 1 Validation and History for Biosafety Manual Director’s Certification: I hereby certify that I have reviewed the contents of this manual and that it reflects my current operating policy for the laboratories (room numbers) located in (building). (Principal Investigators Name – please print on line ) (Signature) (Date) (List all Co-Principal Investigators Name– please print) (Annual Review Dates) 2 Chapter 1– Introduction .................................................................................................. 6 Acknowledgments ..................................................................................................................................... 7 Definitions ................................................................................................................................................. 7 Risk Group Classification ........................................................................................................................ 9 Laboratory Biosafety Level ..................................................................................................................... 9 Chapter 2 - General Information and Structure ......................................................... 10 Commitment to Safety.............................................................................................................................10 Management Structure and Responsibility ...........................................................................................11 Oversight ..................................................................................................................................................11 Chemical Hygiene Plan (CHP) ...............................................................................................................11 Research Agents.......................................................................................................................................11 Laboratory Access ...................................................................................................................................13 Laboratory Security ................................................................................................................................13 Select Agents ........................................................................................................................................13 Personnel Training ..................................................................................................................................14 Facilities ....................................................................................................................................................15 Negative pressure tissue culture rooms .............................................................................................15 Bench Tops ...........................................................................................................................................15 Laboratory Furniture .........................................................................................................................15 Workplace Practice Controls..............................................................................................................15 Vaccinations (if applicable) .....................................................................................................................16 Posting and Labeling Requirements ......................................................................................................16 Signs ..........................................................................................................................................................16 Labels and Tags .......................................................................................................................................16 Audit Management ..................................................................................................................................17 Storage of Biohazardous Materials ........................................................................................................17 Transport of Hazardous Materials to Storage Areas ...........................................................................18 Chapter 3 - Laboratory Practices .................................................................................. 18 Standard Microbiological Practices .......................................................................................................18 Biosafety Procedures ...............................................................................................................................18 Personal Protective Equipment ..........................................................................................................18 Laundry and Decontamination of Protective Clothing ........................................................................19 Standard Microbiological Practices BSL2+ ..........................................................................................20 Good Microbiological Techniques..........................................................................................................21 Use of pipetting aids ............................................................................................................................21 Minimization of aerosol production .......................................................................................................22 Protection of vacuum line .......................................................................................................................22 Syringes and Needles ...............................................................................................................................22 Biological Safely Cabinet Use .................................................................................................................23 Biohazardous Waste Disposal Methods .................................................................................................24 Biohazardous Glassware, Plastics and Other Solid Waste ..............................................................24 Biohazardous Liquids– Sanitary Drain .............................................................................................25 OSEH Hazardous Materials Management (HMM) - Collection of Waste .........................................25 Biohazardous Glassware, Plastics and Other Solid Waste ..............................................................25 Biohazardous Regulated Sharps - Note Sharps cannot be treated by the laboratory ...................25 Biohazardous Liquids .........................................................................................................................26 Chapter 4 - Research Animals ....................................................................................... 27 Use of Sharps with Animals ....................................................................................................................28 Animal waste ............................................................................................................................................28 Chapter 5 – Specific Standard Operating Procedures ................................................ 29 Biological Safety Data Sheets ..................................................................................................................29 3 Chapter 6 – Equipment and Facility Management ..................................................... 30 Equipment Care and Use ........................................................................................................................30 Proper Use of Autoclave......................................................................................................................30 Proper Use of Centrifuges ...................................................................................................................32 Spills and Leaks .......................................................................................................................................33 Blenders, Ultrasonic Disrupters, Grinders and Lyophilizers ..........................................................34 Miscellaneous equipment ........................................................................................................................34 Microscopes ..........................................................................................................................................34 Microtomes...........................................................................................................................................34 Cryostats...............................................................................................................................................34 Water baths ..........................................................................................................................................35 Loop Sterilizers and Bunsen Burners ................................................................................................35 Open Flames in Biosafety Cabinets....................................................................................................35 Other Physical and Chemical Hazards ..................................................................................................36 Dry Ice ..................................................................................................................................................36 Liquid Nitrogen ...................................................................................................................................37 Ultraviolet light ....................................................................................................................................39 Electrical Hazards ...............................................................................................................................40 Gel Electrophoresis .............................................................................................................................40 Ethidium Bromide ...............................................................................................................................40 Acrylamide ...........................................................................................................................................40 Additional Chemical Usage.....................................................................................................................41 Phenol ...................................................................................................................................................41 Chloroform...........................................................................................................................................41 Equipment Maintenance .........................................................................................................................42 Cleaning and Decontamination ..............................................................................................................42 Chapter 7 – Radiation Management ............................................................................. 43 Use of Radioactive Isotopes ....................................................................................................................43 Disposal of Isotopes after Usage .............................................................................................................44 Chapter 8 - Emergency Management ........................................................................... 45 Emergency Procedures............................................................................................................................45 Accidental Exposure to an Infectious Agent .........................................................................................45 Spill Response Procedures for Infectious agents and Recombinant DNA ..........................................46 Spill in the Laboratory ............................................................................................................................47 Skin, Mucous Membrane, or Injury Exposure .....................................................................................48 For exposures to recombinant DNA, perform the following: ..........................................................48 Fire Fighting Procedures ........................................................................................................................49 Reporting and Recordkeeping ................................................................................................................49 Chapter 9 - Shipment and Receipt of Infectious Materials......................................... 50 Receipt of Infectious Materials ...............................................................................................................50 Transportation of Biohazardous Materials ...........................................................................................50 On-Campus Transportation ...................................................................................................................51 Hand Carry Between University Labs or Buildings .............................................................................51 Transport by University Vehicle ............................................................................................................51 Off-site Transportation by Courier .......................................................................................................52 Chapter 10 – Appendices................................................................................................ 53 Appendix 1 ....................................................................................................................... 54 Emergency Call List ................................................................................................................................54 Appendix 2 ....................................................................................................................... 55 Schematic of Laboratory.........................................................................................................................55 Appendix 3 ....................................................................................................................... 56 Roster of Approved Personnel and Training Records .........................................................................56 Appendix 4 ....................................................................................................................... 57 Training Completion Form.....................................................................................................................57 4 Training Checklist ...................................................................................................................................58 Appendix 5 ....................................................................................................................... 61 Housekeeping Inspections .......................................................................................................................61 Appendix 6 ....................................................................................................................... 62 Pathogen Safety Data Sheets for Infectious Agents ..............................................................................62 Appendix 7 ....................................................................................................................... 63 Accident Report Forms ...........................................................................................................................63 Appendix 8 ....................................................................................................................... 65 Standard Operating Procedure ..............................................................................................................65 Appendix 9 ....................................................................................................................... 68 Autoclave Use Log ...................................................................................................................................68 5 Chapter 1– Introduction While this manual is not intended to cover every aspect of biosafety, essential basic procedures, precautions and guidelines are discussed. If basic (BSL level) laboratory practices are performed carefully, along with the appropriate experimental design and common sense, workers should have few problems working safely in the (BSL level) environment. It is essential that laboratory personnel maintain good, sound laboratory work practices and precautions. An awareness and respect for the dangerous nature of certain pathogens should always be maintained. Extensive guidelines regarding biosafety containment levels and various agent summary statements can be obtained from the U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Institutes of Health publication entitled Biosafety in Microbiological and Biomedical Laboratories 5th Edition. This document is available from the Department of Occupational Safety Environmental Health (OSEH) website at http://www.cdc.gov/od/ohs/biosfty/bmbl5/bmbl5toc.htm The guidelines should be read before work in the (BSL Level) laboratory is initiated. In addition, those who plan to initiate work in the lab must be familiar with the standard practices that apply as well. _____________________________ Lab Director ___________________ Date 6 Acknowledgments This Biosafety Manual is the result of assessing the safety-management needs of a variety of laboratories that use biological materials at the University of Michigan. We would like to acknowledge and express our appreciation to all the researchers who contributed to this effort. Definitions Biohazardous Material - any material known to harbor organisms or agents capable of infecting or infesting human or animal hosts or causing environmental harm if released. Biosafety - Biosafety is a specialized practice for proper handling and working with biohazardous organisms or biological material, which may harbor biohazardous organisms. Biosafety fits neatly into the traditional programmed approach to safety: Administrative controls to standardize methods to reduce exposure risk Mechanical engineering controls for containment of hazardous materials Medical surveillance and PPE for potentially exposed employee Workplace monitoring to determine exposure levels Biosafety Levels aka Biological Safety Level- (BSLs) describe the combination of safety practices, safety equipment and facility design used to contain the hazards associated with specific risk groups of microorganisms and is based on risk assessment. Biosafety levels are different from risk groups however risk group information is critical in determining the correct biosafety containment level. See below Blood borne Pathogen - an agent known to be transmissible through contact with human blood, such as the human immunodeficiency virus (HIV) or the hepatitis B virus (HBV). Containment: Primary Containment – The protection of personnel and the immediate laboratory environment from exposure to infectious agents is provided by both good microbiological technique and use of appropriate safety equipment. Secondary Containment – The protection of the environment external to the laboratory from exposure to infectious materials, is provided by a combination of facility design and operational practices 7 Infectious Substance - a viable micro-organism, or its toxin, which causes or may cause disease in humans or animals, and includes those agents listed in 42 CFR 72.3 or any other agent that causes or may cause severe, disabling, or fatal disease. IBC - Institutional Biosafety Committee Occupational Exposure – an exposure that may place personnel at risk of injury or infection is defined as percutaneous (e.g., a needle stick or cut with a sharp object), contact of mucous membranes, or contact of skin (especially when the exposed skin is chapped, abraded, or afflicted with dermatitis or the contact is prolonged or involving an extensive area) with blood, tissues, or other bodily fluids to which universal precautions apply. For the purpose of this manual, the occupational exposure must be to fluids or aerosols known to be infectious. OSEH - University of Michigan, Department of Occupational Safety and Environmental Health OVPR – Office of the Vice President for Research Potentially Infectious Material - any material, which may or is known to contain an etiologic agent of human or animal disease. Principal Investigator/Lab Director - the University of Michigan faculty member responsible for the research underway in the laboratory. For the purposes of this protocol, the Principal Investigator is (List PI, address and phone number) Recombinant DNA Molecules - molecules that are constructed outside living cells by joining natural or synthetic DNA segments to DNA molecules that can replicate in a living cell; or molecules that result from the replication of those described above. UCUCA - University Committee on Use and Care of Animals Risk Groups- are the classification of infectious microorganisms based on principle characteristics such as; route of transmission and severity of disease. See below Standard Microbiological Practices (SMP) - basic safe laboratory work protocols for working with biological materials based on containment level. - The main objective of SMP is to provide safety controls needed to protect workers and the environment from contamination in the event that the agents are accidentally released from their primary container. 8 Risk Group Classification Risk Group 1 (RG1) agents are defined and characterized strains of viable microorganisms not known to consistently cause disease in healthy adult humans or animals. Laboratory personnel may become infected through high doses or unusual routes of exposure that are not commonly encountered in a natural setting. Opportunistic RG1 pathogens may cause serious disease in elderly persons and infants, and persons with compromised immune systems. A risk assessment should be used for vaccine strains, as multiple passages in vivo do not ensure avirulence. Risk Group 2 (RG2) agents are associated with human or animal disease which is rarely serious and for which preventive or therapeutic interventions are often available. RG2 organisms have the capability to cause serious disease based on dose, route of exposure, and immune status. Laboratory exposures may cause serious infection, but the risk of spread of infection is limited. The risk assessment should give special attention to those RG2 organisms for which preventative or therapeutic interventions are not available. Risk Group 3 (RG3) agents are associated with serious or lethal human or animal disease and have the potential for respiratory transmission, and for which preventive or therapeutic interventions may be available. Preventative or therapeutic interventions may not be available for some RG3 agents, or are less available than for RG2 organisms. Risk Group 4 (RG4) agents are associated with serious or lethal human or animal disease. RG4 agents may be transmitted via the aerosol route, can be readily transmitted from one individual to another, directly or indirectly, and for which there is no available vaccine or therapy. RG4 agents are NOT permitted at the University of Michigan. Laboratory Biosafety Level BSL1 practices, safety equipment, and facility design and construction include appropriate laboratories in which work is done with defined and characterized strains of viable microorganisms not known to consistently cause disease in healthy adult humans, and are of minimal potential hazard to laboratory personnel and the environment. The laboratory is not necessarily separated from the general traffic patterns in the building. Work is generally conducted on open bench tops using standard microbiological practices. Special containment equipment or facility design is neither required nor generally used. Laboratory personnel have specific training in the procedures conducted in the laboratory and are supervised by a scientist with general training in microbiology or a related science. BSL2 practices, equipment, and facility design and construction are applicable to teaching and research laboratories in which work is done with the broad spectrum of indigenous moderate-risk agents that are present in the community and associated with human disease of varying severity. U of M requires all activities involving infectious 9 materials be conducted in biological safety cabinets. No work with infectious materials in open vessels will be conducted outside the cabinets. RG2 agents infectious to humans or vertebrate animals are stored or manipulated; Human blood, blood products, or other potentially infectious materials, including commercial cell lines; animal tissues or fluids, especially those collected from nonhuman primates, that are contaminated with an agent infectious to humans or vertebrate animals, or materials that were collected from an animal known to be sick are manipulated, including commercial cell lines; Certain types of research utilizing toxins or venom. BSL3 practices, safety equipment, and facility design and construction are applicable to clinical, diagnostic, teaching, research, or production facilities in which work is done with indigenous or exotic agents with a potential for respiratory transmission, and which may cause serious and potentially lethal infection. Primary hazards to personnel working with these agents relate to autoinoculation, ingestion, and exposure to infectious aerosols. All laboratory manipulations should be performed in a BSC or other enclosed equipment, such as a gas-tight aerosol generation chamber. Secondary barriers for this level include controlled access to the laboratory and ventilation requirements that minimize the release of infectious aerosols from the laboratory. RG3 agents such as; Mycobacterium tuberculosis, St. Louis encephalitis virus, and Coxiella burnetii are representative of the microorganisms assigned to this level. BSL-4 No work at BSL4 is conducted at the University of Michigan Animal Biosafety Levels A similar set of four biosafety levels are provided for work with vertebrate animals infected with agents which may infect humans. These Animal Biosafety Levels, ABSL 1 thru 4, provide for practices, equipment, and facilities that are comparable to the laboratory biosafety levels described above. However, there are unique hazards associated with infected animals that must be understood by those personnel with animal contact and addressed in the animal facility. Animal activity can create aerosols and bites and scratches can occur. Chapter 2 - General Information and Structure Commitment to Safety It is the objective of this laboratory, and its management to practice safety in science and to exercise all reasonable and prudent precautions generally accepted as research industry standards. Guidelines recommended by the CDC and NIH for biosafety will be strictly 10 observed and enforced by the laboratory director and management. At the conclusion of initial personnel training, each lab employee will sign a Training Completion Form (See Appendix 4) to be retained with the training records. Management Structure and Responsibility Overall supervision of the (BSL level) laboratory is the responsibility of (Name of Principal Investigator). Management of daily operations in the lab is the responsibility of (Name of Lab Manager or Responsible Person). Access to the laboratory must be obtained from one or both of the above. Oversight This plan meets the quality standards for laboratory safety management as required by UM-OSEH and OVPR. Chemical Hygiene Plan (CHP) The Laboratory Safety Standard requires employers to write and implement laboratoryspecific Chemical Hygiene Plans (CHP). According to this regulation, a Chemical Hygiene Plan applies to all employers engaged in the laboratory use of hazardous chemicals. A “laboratory” is defined as a facility where the laboratory use of hazardous chemicals occurs. A “hazardous chemical” is defined as a chemical for which there is evidence that acute or chronic health effects may occur in exposed employees. The CHP should include specific work practices, procedures, and policies to ensure that employees are protected from all potentially hazardous chemicals used. Recommendations for completing each section of the Chemical Hygiene Plan are provided on OSEH’s Internet web site. The web site contains a generic CHP that can be down loaded and modified for use in your Lab (http://www.oseh.umich.edu/research/chem-hygiene.shtml ). If you have any questions regarding the CHP, please contact OSEH at 76 3-6973. Research Agents Until otherwise specified, infectious agents approved for use in the laboratory include: (please use genus species naming format and list the risk group (1-3)) Name Name 11 Name Name Pathogen Safety Data sheets (PSDS) if available. http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/index-eng.php Printed copies for the organisms listed above can be found in Appendix 6. 12 Laboratory Access 1) The Principal Investigator or his/her designee authorizes access to the laboratory. Persons requesting to use the laboratory or equipment shall be advised of the potential hazards involved and shall follow all biosafety guidelines as presented in this manual. 2) Access to the (BSL level) laboratory is restricted when work with infectious agents is in progress, after hours, or when laboratory personnel are not available. 3) Restrictions or recommendations will be made on an individual basis. Examples of conditions that might warrant special precautions are HIV infection, immunosuppressive conditions, and drug therapies that suppress the immune system. Additionally, it is recognized that exposure to certain infectious agents may adversely affect a fetus during pregnancy if the mother is infected with the agent. Employees, who fall into any of the above conditions, should inform their personnel physician and the Principal Investigator about the situation. Laboratory Security Certain biohazardous microorganisms and toxins may be of interest to persons or groups involved in terrorism or other illegal activities. Therefore infectious agents that could pose a serious threat to humans, agriculture, or the livestock industry should be kept under secure conditions within the laboratory. Select Agents In compliance with the “Public Health Security and Bioterrorism Preparedness Response Act of 2002” (Public Law 107-188) and the Select Agents regulations from the Centers for Disease Control 42 CFR 73 (http://www.cdc.gov/od/sap/42_cfr_73_final_rule.pdf) and USDA 9CFR 121, 7 CFR 331 (http://www.aphis.usda.gov/programs/ag_selectagent /), any research project which will utilize Select Agents and High Consequence Livestock Pathogens and Toxins on campus requires special registration. Please contact OSEH if you plan to use any of the listed agents or toxins in your research (List of Agents and Toxins, http://www.cdc.gov/od/sap/docs/salist.pdf). The highest level of security is reserved for materials referred to as Select Agents, and these require a Biosecurity Plan to be implemented. The Institutional Biosecurity Plan is available through UM-OSEH and is administered in conjunction with Department of Public Safety. The Plan defines which viable agents and quantities are regulated. If a request is received from another institution or corporate entity for a dangerous organism for academic purposes, the Principal Investigator is responsible for ensuring that the receiving entity is a valid research organization and that the transfer has administrative 13 approval from both institutions. When a request is received, the Principal Investigator must notify the Biological Safety Officer for approval to send the agent. Personnel Training 1) Once a year all personnel working in the (BSL level) laboratory will be instructed by the Principal Investigator or Laboratory Manager on the special biological safety procedures to be used. Attendance at this session is mandatory. 2) OSEH conducts the Comprehensive Laboratory Safety training course several times a month and upon request. All new lab employees and anyone who has not yet attended must attend this course. OSEH recommends that employees be trained at least every three years thereafter. See OSEH’s web page http://www.oseh.umich.edu/training/mylinc.shtml for training dates, times and sign-up procedures. 3) Personnel must have prior experience with the agent in use or must be provided with suitable and sufficient information, instruction and training on working with the agent prior to initiating work. A training course entitled “Working Safely with Viral Vectors is available for new or entry-level lab personnel who plan to use viral vectors in vitro or in vivo, and who cannot demonstrate significant previous experience and expertise in the necessary aspects of biosafety and regulatory compliance. The course is provided by the University of Michigan Vector Core Laboratory and is sanctioned by the Institutional Biosafety Committee (IBC) and the Department of Occupational Safety and Environmental Health (OSEH). Registration for the course is available on the OSEH website at http://www.oseh.umich.edu/training/mylinc.shtml 4) New employees must read a copy of the Biosafety Manual and associated documents as listed in the Training Completion Form (Appendix 4) prior to starting work in the laboratory. 5) New employees must exhibit competency in good microbiological techniques as listed in the Recombinant DNA/ Infectious Agent Training Checklist (appendix 4) prior to starting work in the laboratory. 6) It is the direct responsibility of the Principal Investigator or Lab Manager, to initially instruct new employees of the safety procedures used in the laboratory. This includes a thorough review of the appropriate operating procedures of the laboratory. See Recombinant DNA/ Infectious Agent Training Checklist (appendix 4) 14 Facilities Negative pressure tissue culture rooms In general, a separate tissue culture room provides a higher level of containment for working with potentially airborne recombinant DNA vectors (ex. adenoviral vectors) or infectious agents than the general laboratory. Mechanical ventilation should provide an inward flow of air (negative pressure) without recirculation to spaces beyond the laboratory. This is sometimes referred to as a one-pass ventilation system. Laboratory personnel should verify that the direction of airflow is into the laboratory. UM-OSEH provides this check as a service during inspections. Bench Tops Bench tops should be impervious to water and resistant to acids, alkalis, organic solvents, and moderate heat. The work areas should be kept clean and dust free as to prevent contamination of samples and laboratory acquired infections. Bench tops should be disinfected with 1:10 dilution of bleach solution or other appropriate disinfectant daily, following any spill, and at least once a month when bench top is used infrequently. Laboratory Furniture Laboratory furniture should be capable of withstanding anticipated loading and uses. Spaces between benches, cabinets, and equipment should be accessible for cleaning. Chairs and other furniture used in laboratory work should be covered with a non-fabric material that can be easily decontaminated. Workplace Practice Controls All personnel must routinely use appropriate controls when handling biohazards or materials that may harbor biohazards. These include: Engineering Controls - Primary Barriers (e.g., biological safety cabinets and their respective ventilation systems) are the preferable method for containment of biohazards. Aerosol-generating procedures with biohazardous materials that pose an inhalation risk should always be handled in a biosafety cabinet. A biosafety cabinet is designed to contain microorganisms, which are released during work within the cabinet. Selection of the type of primary barrier should be based on the risk assessment. - Secondary Barriers (e.g., building design features include floor to ceiling walls, operating areas under negative pressure and using closed doors). Many 15 laboratories have monitoring systems built-in to indicate any system failures that could affect secondary containment. Laboratory personnel should be familiar with these devices if they are available. Vaccinations (if applicable) Lab personnel must be provided with information regarding vaccines that may be available to protect them against laboratory acquired infection. Under some circumstances, the Laboratory Director may require immunization as a condition of employment within the biohazard laboratory. Information to be provided to employees includes: efficacy, side effects, booster schedule, etc. Vaccinations should be provided to employees free of charge and during working hours. Vaccinations are provided through a certified Occupational Medical service, such as Occupational Health Services (OHS). Personal health status may impact an individual’s susceptibility to infection, ability to receive immunizations or prophylactic interventions. Therefore, all laboratory personnel and particularly women of childbearing age should be provided with information regarding immune competence and conditions that may predispose them to infection. Posting and Labeling Requirements The necessity for establishing policies and procedures for proper identification of hazardous biological agents within the University's laboratories is to alert support and emergency personnel who may enter the area to take precautionary measures and to restrict traffic to potentially hazardous areas. Signs All areas and laboratories that contain biohazardous agents must be posted with a “Caution” sign. A biohazard label, incorporating the universal biohazard symbol, should be placed on the face of these signs. These signs shall: Indicate the biosafety level of the laboratory. List the name and telephone number for the Principal Investigator to facilitate contact in case of emergency. Required procedures for entering and exiting the laboratory. Contact OSEH at 647-1143 to request a customized door sign. Labels and Tags Biological hazard warning labels must be used to identify containers of infectious materials, infectious waste, refrigerators, incubators and/or freezers where biohazards are stored, infectious waste containers, equipment which may be contaminated through normal use of 16 biohazards, laboratory animals (cages) which are potentially infectious or combinations thereof which are contaminated with biohazardous materials. The label must consist of the universal "Biohazard" Symbol). These labels should be affixed as close as safely possible to the container, refrigerator/freezer, equipment, animal cage or other containers. Audit Management General Maintaining accurate records and documentation is a critical part of any Biosafety Program. In order to prove that specific requirements of the Biosafety Program have been accomplished, appropriate documentation must be filed. Documentation is required for the following: Biosafety training: Documentation should be available to prove that employees have been trained in the proper use of the specific biohazards with which they work. Documentation should be provided for new personnel and to document retraining (See Appendix 4) Accident Investigation and Injury Illness Recordkeeping. http://www.umich.edu/~connect/pdf/iirf.pdf Inspection/Audit Reports: Self-inspection and follow-up reports should be maintained for at least one year. http://www.oseh.umich.edu/pdf/BL2checklist.pdf In the case of highly hazardous organisms (Select Agents), electronic entry logs for the laboratory must be maintained. Storage of Biohazardous Materials All infectious materials to be stored must be clearly labeled. The storage space (e.g., freezer, refrigerator) must also be labeled with the universal biohazard symbol. Additional information including contact name and emergency numbers should be visible in case of emergency, i.e., freezer breakdown. Expired and other unwanted material must be decontaminated properly. Materials for long-term storage must be annually inspected and each container must be checked for cracks and other damages and properly disposed or replaced. In the event of a freezer melt-down, all materials that are unable to be salvaged must be properly treated by autoclaving or chemical disinfection. 17 Transport of Hazardous Materials to Storage Areas Live infectious materials, which are removed from the facility for storage in liquid nitrogen or –80 º freezers, should be stored in non-breakable, cryovials. The vials must be surface decontaminated with 70% ethanol after sealing and then transported to the freezers in non-breakable, impermeable, closed containers (ex. Biotransport Carrier). The container used for this purpose must be labeled with a biohazard label. Chapter 3 - Laboratory Practices All Biosafety Containment level practices and facilities encompass all the requirements described below as well as containment level specifics outlined in this manual. Standard Microbiological Practices Persons working in the laboratory must be fully aware of the potential hazards to themselves and their co-workers. Personnel must meet the specific entry/exit requirements for this space. Persons must wash their hands after working with potentially infectious materials and before leaving the laboratory. Eating, drinking, smoking, handling contact lenses, applying cosmetics, and storing food for human consumption are not permitted in the laboratory Food must be stored outside the laboratory area in cabinets or refrigerators designated and used for this purpose. Mouth pipetting is strictly prohibited; mechanical pipetting devices must be used Policies for the safe handling of sharps, such as needles, scalpels, pipettes, and broken glassware must be developed and implemented. Whenever practical, laboratory supervisors should adopt improved engineering and work practice controls that reduce risk of sharps injuries. Laboratory coats, gloves, and protective eyewear must be worn when working in the laboratory Non-experimental animals and plants are not permitted in the laboratory. Biosafety Procedures Personal Protective Equipment Personal Protective Equipment (PPE). PPE should be selected in accordance with the hazards identified. All laboratory personnel are required to wear appropriate PPE corresponding to the chemical, biological and radiological substances being used. Appropriate PPE may include: gloves, safety glasses, safety goggles, face shields and laboratory coats. The minimum level of protective equipment in a lab should include lab coats, safety glasses and appropriate gloves. Persons who wear contact lenses should 18 also wear eye protection. To determine if the laboratory personnel are wearing the appropriate type of glove, you can refer to a glove selection chart. Glove selection charts are available through various laboratory supply catalogs. Two pairs of gloves should be worn when appropriate. Alternatives to latex gloves should be available. Dispose of protective clothing appropriately, or deposit it for laundering. Do not launder lab coats at home. OSEH can assist in the correct selection of PPE. Laboratory dress code should strongly discourage the wearing of shorts and open toe shoes. The Personal Protective Equipment, General Guideline has been developed to provide the University community with the necessary information to identify work situations that require the use of PPE, the proper selection and use of PPE, and documentation of this information. This information is important to help ensure the safety and health of all UM employees. The Personal Protective Equipment, General Guideline can be found on OSEH’s web site at http://www.oseh.umich.edu/pdf/guideline/ppe_guideline.pdf . Special handling practices include: The frequent changing of PPE; changing gloves when the gloves are contaminated or the integrity has been compromised, or when otherwise necessary; do not wash or reuse disposable gloves. Eye, face and respiratory protection should be used in rooms containing infected animals as determined by the risk assessment. The removal of PPE when work has been completed with infectious materials or when leaving the lab followed by hand washing with an appropriate decontaminating soap Disposing of PPE with other contaminated laboratory waste or decontaminated it before reuse. Ensuring eye and face protection (goggles, mask, face shield or other splatter guard) is used for anticipated splashes or sprays of infectious or other hazardous materials when the microorganisms must be handled outside the biosafety cabinet or containment device. Prohibition of eating, drinking, smoking, chewing gum, removing contact lenses, or applying cosmetics either while in the biohazard area or while wearing potentially contaminated PPE. Laundry and Decontamination of Protective Clothing Potentially contaminated lab coats or protective outer garments are to be handled as little as possible with a minimum of agitation to prevent contamination of the air or of persons handling them. The risk of actual disease transmission from contaminated laundry is low, however care should be taken when handling such clothing. Lab coats should not be taken home for laundering. Professional laundering service is available. Disposable lab coats are available as an option. 19 Standard Microbiological Practices BSL2+ All of the above plus 1) All procedures are performed carefully to minimize the creation of splashes or aerosols. All infectious agents are handled in a biosafety cabinet. 2) Work surfaces should be decontaminated at least once a day and after any spill or splash of potentially infectious material with appropriate disinfectant . 3) All cultures, stocks, and other regulated wastes are decontaminated before disposal by an approved decontamination method, such as autoclaving immediately after use. Materials to be decontaminated outside of the immediate laboratory are to be placed in a durable, leak-proof container and secured for transport from the laboratory. 4) Laboratory personnel must be provided medical surveillance, as appropriate, and offered available immunizations for the agents handled or potentially present in the laboratory. 5) Careful management of needles and other sharps are of primary importance. Used disposable needles must not be bent, sheared, broken, recapped, removed from disposable syringes, or otherwise manipulated by hand before disposal. Used disposable needles must be carefully placed in conveniently located punctureresistant containers used for sharps disposal. 6) Do not handle broken glassware directly by hand. The glassware should be removed by mechanical means such as a brush and dustpan, tongs, or forceps. Plastic ware should be substituted for glassware whenever possible. 7) Place all cultures, tissues, or specimens of body fluids in a durable leak-proof containers that prevents leakage during collection, handling, processing, storage, transport, or shipping. 8) PPE requirements; dedicated lab coat that remains in lab, gloves and eye protection. Laboratory personnel must wash their hands after working with potentially hazardous materials and before leaving the laboratory. Fabric lab coats autoclaved before laundering. 9) Spills and accidents should be immediately reported to the Principal Investigator and the University Biological Safety Officer (647-1143). 20 Good Microbiological Techniques Use of pipetting aids Pipettes are used for volumetric measurements and transfer of fluids that may contain infectious, toxic, corrosive or radioactive agents. Laboratory associated infections have occurred from oral aspiration of infectious materials, mouth transfer via a contaminated finger and inhalation of aerosols. Exposure to aerosols may occur when liquid from a pipette is dropped onto the work surface, when pipetting liquid cultures, or when the last drop of an inoculum is blown out. A pipette may become a hazardous piece of equipment if improperly used. A variety of pipetting aids are available, but caution must be exercised with all of them as the use of excessive force when inserting a pipette can fracture the pipette and cause serious injury to the hands. The safe pipetting techniques, which follow, are required to minimize the potential for exposure to hazardous materials. Mouth-pipetting any substance, however innocuous, is prohibited Replace glass pipettes with disposable options whenever possible. If working with biohazardous or toxic fluid, confine pipetting operations to a biosafety cabinet. Always use cotton-plugged pipettes when pipetting biohazardous or toxic materials, even when safety pipetting aids are used. Check your pipette at the beginning of the working day for dust and dirt on the outside. If needed, wipe with 70% ethanol. Do not prepare biohazardous materials by bubbling expiratory air through a liquid with a pipette. Do not forcibly expel biohazardous material out of a pipette. Never mix biohazardous or toxic material by suction and expulsion through a pipette. Do not discharge material from a pipette at a height. Whenever possible allow the discharge to run down the container wall. Prevent cross contamination by: using sterilized tips or sterilized filter tips and autoclave the pipette. Avoid contamination to or from fingers by using the tip ejector. Keep the pipette vertical when pipetting in order to prevent the liquid from running into the pipette body Place contaminated, reusable pipettes horizontally in a pan containing enough liquid disinfectant to completely cover them. Do not place pipettes vertically into a cylinder. Autoclave the pan and pipettes as a unit before processing them for reuse. Pans or collection containers for contaminated pipettes should be placed inside the biosafety cabinet. 21 Minimization of aerosol production Procedures with a high potential for creating aerosols, such as vigorous shaking and vortexing, should be performed in the back third of the biological safety cabinet. Never pour or decant virus suspensions. Do not forcibly expel the last drop of infectious agent suspension from a pipette. Discharge pipetted material near the surface of fluid or down the wall of a tube. When opening culture tubes, bottles and flasks, manipulate them slowly. When resuspending liquid cultures, use a swirling action to create a homogeneous suspension with a minimum of aerosolization. Once cultures are resuspended, wait a few minutes to reduce aerosols before opening the container. Do not spray disinfectant directly onto liquid spills, as this will create aerosols. Instead cover spill with paper towels and pour disinfectant, around and over the spill. Allow suitable contact time (20 minutes). Protection of vacuum line Vacuum lines should be protected by a disinfectant trap. Use a plastic aspirator suction flask with a second vacuum flask connected to it as a backup. To the second vacuum flask attach a high efficiency particulate air (HEPA) vacuum filter (ex. VacuShield product). These filters can isolate and confine infectious materials, preventing fluid and aerosol contamination of vacuum pumps or aspiration suction systems. Filters are available through laboratory supply catalogs. Contact OSEH (647-1143) if you need more information regarding HEPA filters for your vacuum system. The vacuum collection flasks should be attached in series from the vacuum source in the biosafety cabinet or a vacuum pump. If this set up is placed outside of the biosafety cabinet, it should be contained in a tray or pan to prevent accidental spills. Syringes and Needles Syringes and hypodermic needles are dangerous instruments. The use of needles and syringes should be restricted to procedures for which there is no alternative. Blunt cannulas should be used as alternatives to needles wherever possible (i.e., procedures such as oral or intranasal animal inoculations). Needles and syringes should never be used as a substitute for pipettes. When needles and syringes must be used, the following procedures are recommended: Use disposable needle locking syringe units whenever possible. When using syringes and needles with biohazardous or potentially infectious agents: a. Work in a biosafety cabinet whenever possible. b. Wear gloves. c. Fill the syringe carefully to minimize air bubbles. 22 d. Expel air, liquid and bubbles from the syringe vertically into a cotton pledget moistened with disinfectant. e. Do not use a syringe to mix infectious fluid forcefully. f. Do not contaminate the needle hub when filling the syringe in order to avoid transfer of infectious material to fingers. g. Wrap the needle and stopper in a cotton pledget moistened with disinfectant when removing a needle from a rubber-stoppered bottle. If there is concern of the disinfectant contaminating sensitive experimental materials, sterile cotton square may be used and immediately discarded into an autoclave bag. Bending, recapping, clipping or removal of needles from syringes is prohibited. If it is essential that a contaminated needle be recapped or removed from a syringe, the use of a mechanical device or the one handed scoop method must be used. The use of needle clipping devices is prohibited and the devices must be discarded. Use a separate pan of disinfectant for reusable syringes and needles. Do not place them in pans containing pipettes or other glassware in order to eliminate sorting later. Used disposable needles and syringes must be placed in conveniently located appropriate sharps disposal containers and discarded as infectious waste. Biological Safely Cabinet Use The biological safety cabinet (bsc) is the principal device used to provide containment of infectious splashes or aerosols generated by many microbiological procedures. To assure sterility inside the cabinet and establish proper air flow for containment, the blower should be turned on at least 10 minutes before infectious materials are to be put in the biosafety cabinet. Check to ensure that the airflow markers fall within the posted safe ranges before working in the hood. Airflow alarms are present on all cabinets. If airflow is incorrect, discontinue work and contact OSEH at 647-1143. Make sure that all biohazard materials are properly secured, and notify the Principal Investigator or Laboratory Manager. Before using the biosafety cabinet, wipe down the interior so as to avoid accidental exposure to potentially infectious agents and to avoid contamination of cultures. Use 10% bleach, followed in 5 to 10 minutes with 70% ethanol to prevent pitting of the stainless steel, and allows to dry. Always keep a bottle of disinfectant (e.g., bleach, 70% ethanol, etc.) in the hood for decontaminating, or in case of a spill. 23 All activities involving infectious materials must be conducted in biological safety cabinets. No work with infectious materials in open vessels will be conducted outside the cabinets. Work should be performed as deeply into the biological safety cabinets as possible. NEVER place anything over the front grille of a cabinet. Disrupting the airflow in this manner allows contaminated air from inside the cabinet to blow out of the cabinet into the lab or directly at the person sitting at the cabinet. It also allows non-sterile air from the room to blow into the cabinet over your experiments. Materials should be placed in the bsc so as to not block air flow into the rear grille. Leave a few inches for air to flow around things. Any disruption of the airflow in the cabinet decreases its effectiveness. Before manipulating infectious materials, try to make sure that you have everything you need in the bsc. The fewer times you pull your hands out of the bsc, the less disruption of the airflow. Any infectious agents that are centrifuged must be contained in screw cap tubes and the aerosol-barrier rotor caps used. The centrifuge container must be loaded and unloaded in the biological safety cabinet. Any waste generated in the biological safety cabinet must be decontaminated or autoclaved for disposal. The biological safety cabinet must be disinfected with the appropriate disinfectant after each use. Biohazardous Waste Disposal Methods The following are various methods of disposal/treatment for different types of biohazardous waste. Biohazardous Glassware, Plastics and Other Solid Waste Autoclave (Steam Sterilization) Laboratories with access to an autoclave should treat their own solid biohazardous waste and verify the sterilization of waste monthly by using a biological indicator (Appendix 9). Check that there are no standing liquids or hazardous chemicals. Place waste in a university standard autoclave bag – a clear bag with a biohazard symbol and a printed-on sterilization indicator badge (example Fisher Scientific part number 01-826A). Autoclave with bag open or loosely tied. After sterilization cycle, close bag. The sterilized waste can be transported directly to the dumpster by Building Services or laboratory staff, without boxing or labeling. 24 Chemically Disinfect Soak contaminated materials in 1:10 dilution (10% concentration) of household bleach (contains 5% sodium or calcium hypochlorite) to water or other suitable commercial disinfectant. Note: if contaminated materials contain a high organic load use 1:5 dilution (20% concentration) of bleach, 1% sodium or calcium hypochlorite. Following treatment, place the waste in an impervious container such as a cardboard box and label as uncontaminated glass or plastic waste. Building Services or laboratory staff can transport this waste to the dumpster. Biohazardous Liquids– Sanitary Drain Ensure there are no chemicals in this waste. Treat liquid biohazardous waste with a 1:10 dilution of household bleach (contains 5% sodium or calcium hypochlorite) to water for at least 30 minutes or use another suitable commercial disinfectant. Note: if liquid materials contain a high organic load use 1:5 dilution (20% concentration) of bleach. Follow manufacturer’s label instructions for appropriate concentration and contact time. Rinse the treated material down the drain with copious amounts of water OSEH Hazardous Materials Management (HMM) - Collection of Waste Biohazardous Glassware, Plastics and Other Solid Waste ***If a laboratory does not have access to an autoclave, HMM (763-4568) must be contacted for collection of the waste. Solid biohazardous waste should be collected in a properly labeled biohazard pail or biohazard box. Various containers are available through Hazardous Materials Management (HMM). Containers can be ordered by calling HMM at 763-4568. All containers of solid biohazardous waste must have a “biohazard label” attached. Labels are available through HMM for identifying biohazardous waste. Labels can be ordered by calling HMM at 763-4568. When waste accumulation begins the accumulation start date must be written on the label. The accumulation start date is the date the waste is first generated. All biohazardous waste must be treated or sent for disposal within 60 days. Biohazardous Regulated Sharps - Note Sharps cannot be treated by the laboratory All sharp objects such as scalpel blades, hypodermic needles, Pasteur pipettes and, contaminated broken glass etc. must always be disposed of in approved "sharps collection bins" (available from HazMat). A fluorescent orange or orange-red label that has the biohazardous symbol in a contrasting color must be affixed to the container. 25 Biohazardous Liquids ***If a laboratory cannot dispose of the material in the sanitary drain, HMM can be contacted for collection of the waste. Various containers are available through Hazardous Materials Management (HMM) for the collection of Liquid biohazardous waste. Containers can be ordered by calling HMM at 763-4568. Package the container in a cardboard box so that the material can safely be moved by HMM staff. All containers of solid biohazardous waste must have a “biohazard label” attached. Labels are available through HMM for identifying biohazardous waste. Labels can be ordered by calling HMM at 763-4568. When waste accumulation begins the accumulation start date must be written on the label. The accumulation start date is the date the waste is first generated. All biohazardous waste must be treated or sent for disposal within 60 days. Pathological Waste- Note all pathological waste must be sent for proper disposal through HMM Place pathological waste in a 5-gallon bucket and securely seal the lid. A fluorescent orange or orange-red label that has the biohazardous symbol in a contrasting color must be affixed to the container. Call HazMat at 763-4568 for waste pick-up. For further information see the Laboratory Refuse Collection Poster http://www.oseh.umich.edu/labcoll.shtml and/or Biohazardous Medical Waste Guideline http://www.oseh.umich.edu/pdf/guideline/guidbmwd.pdf . 26 Chapter 4 - Research Animals All research experiments involving animals shall be conducted in accordance with the associated Institutional Animal Care and Use Committee (IACUC) approved protocol. Animal research that involves a hazard (biological, radiological, or chemical) shall be reflected in the approved IACUC protocol. Contact the IACUC office for additional information. The Department of Biological Safety shall approve work with human pathogens or recombinant DNA in animals (including transgenic animals) prior to initiation. Contact the Department of Biological Safety to initiate the approval process. Care and Handling of Research Animals Comprehensive reviews indicate that animals infected with a wide range of biological agents are capable of shedding infectious micro-organisms in the saliva, urine or feces. In the absence of specific information to the contrary, all infected animals should be regarded as potential shedding infectious micro-organism. Procedures appropriate for the handling of infected animals are given below: Careful handling procedures should be employed to minimize the dissemination of dust from the animal, bedding and the cage. Cages should be sterilized by autoclaving. Feeding and watering devices should remain in the cage during sterilization. All water devices should be of the "non-drip" type. Cages should be examined each morning and at each feeding time so that dead animals can be removed. Dead animals should be placed in leak-proof containers (plastic bags, covered metal trays, canisters, or fiber cartons) that are appropriately marked with date, experiment, biohazard label, cage number, etc., and stored in designated refrigerators or cold rooms prior to necropsy or disposal. Heavy gloves should be worn when feeding, watering, handling, or removing infected animals. Bare hands should never be placed in the cage to move any object. When animals are to be injected with infectious agents, the animal handler should wear appropriate PPE including protective gloves should be worn according to procedures posted. All disposable PPE is single use and should be disposed of in the designated waste container upon exiting the space. Protective eyewear including safety glasses or goggles should be decontaminated and remain in the room. Restraint devices and practices should be used to reduce the risk of exposure during animal manipulation and administration should take place inside a certified biosafety cabinet. All lab staff administering biohazardous material to animals or staff who will be handling animals following administration must complete the Unit for Laboratory Animal Management (ULAM) Hazard Containment Lecture and Workshop. Sign-up for these courses is available on the ULAM website www.ulam.umich.edu 27 Infected animals to be transferred between buildings should be placed in ventilated cages or other aerosol-proof containers. Animals exposed to infectious agents in aerosols should be housed in individually ventilated cages in gas-tight cabinet systems, or in rooms designed for protection of personnel by use of ventilated suits or biological safety cabinets. Additional standard and special practices for Animal Biosafety Levels 1 through 4 are described in Biosafety in Microbiological and Biomedical Laboratories. No work for animal biosafety level 4 is permitted at U of M. Use of Sharps with Animals When inoculating animals, position the hand that is holding the animal “behind” the needle or use a pair of forceps to hold the animal in order to avoid puncture wounds. Be sure the animal is properly restrained prior to the inoculation and be on the alert for any unexpected movements of the animal. Before and after injection of an animal swab the injection site with an appropriate antiseptic. Animal waste Animal waste shall be considered infectious if it is derived from animals infected with zoonotic diseases (transmissible from animals to human) or purposely infected with agents infectious to humans. Carcasses, body parts, tissue, body fluids, excreta, and bedding should be considered infectious. Animal waste can be properly disposed of in the DLAR facility. Animal carcasses that have not been intentionally infected should be returned to DLAR for disposal. Do not place animal carcasses in with other biohazardous waste to be autoclaved. Infected animal carcasses or tissue that is also contaminated with hazardous chemicals or radioactive materials is a type of mixed waste. This type of waste poses special safety and regulatory problems and should not be generated if at all possible. The Office of Environmental Management should be consulted before generating this type of waste. 28 Chapter 5 – Specific Standard Operating Procedures Standard operating procedures for research involving biohazardous and rDNA materials must be developed. Laboratory staff must be trained on SOPs annually and/or whenever new SOPs are added. Required elements of an SOP include: risk identification, exposure controls, and emergency response procedures for handling spills and injuries, waste disposal, shipment and/or receipt of materials. Additional procedures should be written to protect laboratory and animal care staff from animals that have been exposed to biological agents. Examples of specific procedures for individual operations can be found in Appendix 8. Safety precautions should be noted for each procedure. A Standard Operating Procedure template is available in Appendix 8. Biological Safety Data Sheets In addition to the inventories of Safety Data Sheets (SDSs) compiled for hazardous chemicals, all laboratories performing research with known or potential bio-hazardous agents must maintain a comprehensive collection of Pathogen Safety Data Sheets(PSDSs) for each bio-hazardous agent. Questions or concerns regarding acquisition of PSDSs of biohazardous materials should be directed to OSEH at 647-3133. 29 Chapter 6 – Equipment and Facility Management Equipment Care and Use Proper Use of Autoclave 1) Steam Sterilization is defined as 121C for at least 15 minutes peak temperature. A conventional autoclave used in laboratories may take as long as 15 minutes to reach peak temperature, and may take 15 minutes or more to be safe to open. Therefore, a standard autoclave “cycle” is at least 45 minutes total, under ideal conditions. Any interfering factors would necessarily increase this treatment time. 2) An autoclave must be available for the (BSL Level) laboratory and must only be operated by personnel who have been properly trained in its use. Autoclave Safety Training is available through OSEH. See the OSEH website for further information and registration http://www.osehtraining.umich.edu/osehtraining/ . Improper sterilization could result in laboratory personnel, other personnel involved in disposal of laboratory waste, or the community at large being exposed to potentially infectious agents. Chemical integrators are recommended for every load; place on the middle, largest, or densest of the waste bag. A subsequent color change indicates that the load has been exposed to the required conditions for a sufficient length of time. Record autoclave waste runs in the log form appendix 9. 3) Biohazardous materials must not be placed in autoclaves overnight in anticipation of autoclaving the next day. 4) Wrap packages to allow for steam penetration; aluminum foil does not allow steam penetration, and should not be used for wrapping. 5) Do not overload the chamber. 6) Avoid over packing of autoclave bags. 7) Do not seal bags or close bottles and other containers tightly. 8) Do not stack containers. 9) Label waste by writing lab name and date on autoclave tape The changes that are seen on autoclave indicator tapes following an autoclave cycle do not guarantee that the contents of containers are sterile: they indicate only that the tape on the outside of the packages has been exposed to a certain amount of heat or steam. Proper autoclave performance is essential for sterilization. The time required for effective 30 sterilization depends on the size of the load, volumes of liquid and density of materials to be autoclaved. Assessing autoclave performance regularly (at least once per month) is critical, the use of a heat-resistant biological indicator (BI) such as Bacillus stearothermophilus, should be used to ensure that the cycle in use really achieves sterilization conditions. (See Autoclave Performance Program) Safe work practices when using an autoclave include the following: Read the operating manual and post proper work procedures near the autoclave. Never autoclave hazardous chemicals. Dry hypochlorites, or any other strong oxidizing material, must not be autoclaved with organic materials such as paper, cloth or oil: OXIDIZER + ORGANIC MATERIAL + HEAT = MAY PRODUCE AN EXPLOSION. Special precautions should be taken to prevent accidental removal of material from an autoclave before it has been sterilized or simultaneous opening of both doors on a double door autoclave. Open the door slightly to allow escape of steam before unloading. Wear insulated gloves or mitts when unloading. Autoclave Performance Program Purpose: To ensure autoclaves are performing correctly. All general use autoclaves used for the sterilization of biological and recombinant DNA-containing waste must be validated at least once per month. A heatresistant biological indicator (BI) such as Bacillus stearothermophilus, must be used to test the microbial killing power of the sterilization process; it is important to use a positive control (an indicator not autoclaved). Ensuring that sterilization is occurring in the autoclave is of the utmost importance as it relates to human safety; to facilitate this process a log sheet to document monthly performance verification of sterilization is provided below for printing. Log sheet should be kept in biosafety manual page 67. Guidance on basic autoclave procedure: Estimate the total volume of solids and add time to the sterilization cycle for larger amounts of material. • 2 liters = 30 minutes (e.g. 2 sleeves of LB plates made from 2 liters of media) • 4 liters = 60 minutes • 6 liters = 90 minutes Add water to bags of waste containing mostly dry materials (paper towels, gloves, tips, etc.) to help generate steam for sterilization. Put bags of waste in a heat resistant autoclave bin or tray to prevent fluid from leaking out of bag into the autoclave. (See example image below) 31 Do not twist the bags closed and tape shut them when preparing them for autoclaving as this prevents the steam from being able to penetrate the waste and prohibits the sterilization process. (See example image below) Do put lab name and date on autoclave tape in case there are questions regarding the waste the appropriate lab can address concerns. (See example image below) Failure Procedure: If the autoclave has failed to pass criteria that indicate sterilization has occurred. The tests should be repeated once more and if the failure is confirmed, the appropriate contact person for the autoclave must be notified of the autoclave failure. The autoclave contact person is expected to follow up the maintenance service provider for the autoclave. Notice of failure must be provided to all users by placing an “Out of Order, Do Not Use!” sign conspicuously on the autoclave concurrent with a request for repair. Proper Use of Centrifuges All centrifugation shall be done using centrifuge safety buckets or sealed centrifuge tubes in sealed rotors. Each person operating a centrifuge should be trained on the proper operating procedures. Improperly used or maintained centrifuges can present significant hazards to users. Failed mechanical parts can result in release of flying objects, hazardous chemicals and biohazardous aerosols. The high-speed spins generated by centrifuges can create large amounts of aerosol if a spill, leak or tube breakage occurs. The following procedures for centrifugation are recommended: 1) 2) Check glass and plastic centrifuge tubes for stress lines; hairline cracks and chipped rims before use. Use unbreakable tubes whenever possible. Fill and decant all centrifuge tubes and bottles within the biological safety cabinet. Avoid filling tubes to the rim. The maximum for centrifuge tubes is ¾ 32 3) 4) 5) 6) 7) 8) 9) 10) 11) full. Wipe outside of tubes with disinfectant before placing in safety cups or rotors. Use screw top caps or stoppers on centrifuge tubes. Avoid using lightweight materials such as aluminum foil as caps. Once samples to be centrifuged are prepared, load tubes into buckets inside the biological safety cabinet and seal carefully before moving to centrifuge. Aerosol-free (sealed) centrifuge buckets or rotors are required for all centrifuging of infectious substances. Only the correct size tubes should be used in any centrifuge bucket. Buckets should be kept clean and free of broken glass and plastic. Follow manufactures recommendations for tube and rotor maximum safe operation speeds. Ensure the rotor has stopped before opening the centrifuge lid when the run is complete. After centrifugation, buckets should be opened in a biological safety cabinet to prevent exposure from aerosolized particles. Always visually inspect rotor for signs of tube leakage prior to opening buckets. Decontaminate the outside of the cups or buckets before and after centrifugation. Clean and disinfect rotors, and centrifuge interiors. Inspect Orings regularly and replace if cracked or dry. Never leave a centrifuge in a contaminated state. Ensure that the centrifuge is properly balanced. When using high-speed or ultra-centrifuges, additional practices should include: Connect the vacuum pump exhaust to a disinfectant trap. Record each run in a log book: keep a record of speed and run time for each rotor. Install a HEPA filter between the centrifuge and the vacuum pump. Never exceed the specified speed limitations of the rotor. Regularly inspect the rotor for contamination, corrosion, or cracks. Spills and Leaks Report all spills of infectious agents to OSEH Biosafety. In the event a sample may spill or leak inside the centrifuge due to failure of the rotor or associated centrifuge parts the following steps should be followed: Close the centrifuge lid immediately with the samples remaining inside and turn the centrifuge off. It may be necessary to vacate the lab depending on the nature of the spilled material and its ability to generate an aerosol. When the lab must be vacated, 33 secure the room such that others cannot gain access. Post signage indicating restricted entry. All personnel should decontaminate themselves and seek medical attention as necessary. Notify principal investigators, lab supervisors, and coworkers as soon as possible. Wait at least 30 minutes before entering the lab to allow aerosols to settle and decontaminate. Note this step is based on risk assessment lab should have SOP based on agents used in lab. Blenders, Ultrasonic Disrupters, Grinders and Lyophilizers The use of any of these devices results in considerable aerosol production. Blending, cell-disrupting and grinding equipment must be used in a biological safety cabinet when working with biohazardous materials. Miscellaneous equipment Microscopes Tighten caps on flasks of infectious culture before transporting to the microscope. Infectious cultures in plates or other containers without tight fitting lids must be carried to the microscope in a tray. When using the hemacytometer to count cells, enclose the hemacytometer in a 70% ethanol-disinfected petri dish for transport to the microscope. Disinfect the viewing platform of the microscope after each use. Microtomes Microtome blades are extremely sharp and must be handled with great care and stored safely when not in use. If the knife projects beyond the sectioning area, a suitable guard must be fitted. Handling and changing of microtome blades causes many injuries, and great care must be exercised when performing these operations. Always carry the knife, in its case, to the microtome. Never leave the knife on a microtome. After use, always return the knife to its case or dispose of immediately. Disinfect the microtome by wiping with bleach or sodium hydroxide solution. Slide the ''back'' on to the knife before removing it. Cryostats Frozen sections of unfixed human tissue or animal tissue infected with an infectious agent pose a risk of infection. Freezing tissue does not inactivate infectious agents. Freezing propellants under pressure should not be used for frozen sections as they may cause spattering of droplets of infectious material. Gloves should be worn during preparation of frozen sections. Consider the contents of the cryostat to be contaminated and decontaminate it frequently with 70% ethanol. 34 Consider trimmings and sections of tissue that accumulate in the cryostat to be potentially infectious and remove them during decontamination. Defrost and decontaminate the cryostat with a tuberculocidal hospital disinfectant once a week and immediately after tissue known to contain infectious substances is cut. Handle knives with extreme care. Stainless steel mesh gloves should be worn when changing knife blades. Consider solutions for staining potentially infected frozen sections to be contaminated Water baths Pathogenic or nonpathogenic agents may contaminate water baths. It is recommended that either 1 oz. of bleach or 1 oz. of phenolic detergent be added to each gallon of water used in a bath. Phenolic disinfectants are preferred over bleach, but phenolics must be replenished regularly. Propylene glycol has been used effectively as an alternative in cold-water baths. Raise the temperature to 90ºC or higher for 30 minutes once a week for decontamination purposes. Avoid using sodium azide to prevent growth of microorganisms (sodium azide forms explosive compounds with some metals). Thimerosol should also be avoided as a bacteriostat or fungistat as it contains mercury. All forms of mercury are poisonous if absorbed. Treated water must be disposed of as hazardous waste. To prevent electrical shocks, unplug the unit before filling or emptying. Loop Sterilizers and Bunsen Burners Sterilization of inoculating loops or needles in an open flame generates small-particle aerosols, which may contain viable microorganisms. A shielded electric incinerator or hot bead sterilizer should be used to minimize aerosol production. Disposable plastic loops and needles are good alternatives. Alternatively, disposable plastic loops and needles may be used for culture work where electric incinerators are not available. The loops are semi quantitative and can be used for counting bacteria. Open Flames in Biosafety Cabinets Open flames inside a biosafety cabinet create airflow turbulence that may compromise sterility and worker protection, and heat buildup may damage the HEPA filters. Open flames are extremely dangerous around flammable materials, such as ethanol, which is often found in biological safety cabinets. Follow these tips for avoiding fires in your biological safety cabinet: Use disposable pre-sterilized loops and spreaders. Replace Bunsen burners with alternative technology such as electric loop sterilizers 35 Use only Bunsen burners without pilot flame, excess-temperature protection, flame monitor, and regulated timer. Ensure that the gas supply is clearly labeled inside the cabinet. Inspect your gas lines inside the cabinet before use for kinks, tears, holes, and loose connections and replace worn/damaged lines. Stabilize the alcohol container so that it cannot be tipped over. Reduce the amount of flammable chemicals, equipment and supplies in the cabinet. Use only enough alcohol for one day’s work. Have a “snuffing” lid available in case the alcohol in the container catches fire. Water is not a good choice for putting out fires in biological safety cabinets. If you smell gas, turn off the exterior gas valve and wait until the gas has fully dissipated before lighting any flames. Remember that a biological safety cabinet recirculates air and vapors may build up inside the cabinet. Other Physical and Chemical Hazards Dry Ice Dry ice is the solid form of carbon dioxide, non-combustible, available in flakes, pellets or block form. Dry ice will sublime (vaporizes directly to the gas state) at a temperature of –78.5C (-109.3 F) or higher. Dry ice is commonly purchased from a commercial manufacturer. Dry ice is commonly used to cool reactions or to ship biological specimens. All University lab personnel must follow the safe storage, usage, and handling of dry ice. University personnel responsible for shipping packages containing dry ice, must be properly trained according to Department of Transportation (DOT) and International Air Transport Association (IATA) Regulations. Storage Dry ice is to be stored in a well-ventilated location and placed in a Styrofoam chest, insulated cooler, or a special cooler designed for the storage of dry ice. Because of the thermal expansion of dry ice (one pound of dry ice produces about 250 liters of gaseous carbon dioxide), sufficient gaseous carbon dioxide can be released in a sealed container to cause an explosion. Dry ice is NEVER to be stored in any type of tightly sealed devices such as an ultra-low freezer or plastic/glass container. 36 Dry ice will sublimate about five to ten pounds every 24 hours (blocks last longer) in a typical storage cooler. Plan on purchasing dry ice as close as possible to the time needed. Normal air is composed of 78% nitrogen, 21% oxygen, and only 0.04% carbon dioxide. Concentrations greater than 0.5% (5000 ppm) can become dangerous. Therefore, handle dry ice in well-ventilated locations. Hazards/Precautions: Burns/frostbite: Dry ice can cause burns to the skin in short periods of times. Thermal gloves are to be used if it is necessary to handle dry ice. Suffocation: carbon dioxide is a simple asphyxiant. Always store dry ice in a well-ventilated area to minimize the buildup of carbon dioxide. Personnel must use caution should dry ice be stored in a deep cooler. Personnel must never stick one’s head into the chest to obtain the dry ice. Explosions: Placing dry ice into a tightly sealed container can permit sufficient gas build up to cause an explosion. Never place dry ice inside an ultra-low freezer or other enclosed space. Placement of dry ice in rooms with little or no ventilation can result in a build-up of the carbon dioxide in the area. Do not store dry ice in a confined area such as walk-in coolers, refrigerators, freezers, closets, or cars/vans. When using dry ice to ship materials, the shipper must abide to all applicable shipping regulations. Disposal Dispose unneeded dry ice by letting the unused portion sublimate (recommended for well-ventilated locations because it will occur over a period of several days and the ventilation will take care of the gas liberated); NEVER dispose of dry ice in a sink, toilet or other drain (such action can destroy the structure because of the temperature difference); NEVER dispose of dry ice in the trash or garbage; and NEVER place unneeded dry ice in corridors (some corridors may not be well ventilated and the oxygen level can be reduced to low levels). Liquid Nitrogen Liquid nitrogen is frequently used in chemical research laboratories for the purpose of cooling. There are two major risks associated with the use and handling of liquid nitrogen which present potential hazards: - Liquid nitrogen is extremely cold. At atmospheric pressure, liquid nitrogen boils at -196°C. - Liquid nitrogen produces a large amount of nitrogen gas. 37 Do not allow objects cooled by liquid nitrogen to touch your bare skin. Contact with the skin may cause serious frostbite. Because it is extremely cold, it can freeze human flesh almost instantaneously. Use forceps or tongs to remove straws or canes from the storage container. Protective clothing can reduce the hazards of handling liquid nitrogen. Insulated or heavy leather gloves should always be worn when handling any object that has been in contact with liquid nitrogen. Loose fitting gloves are recommended so that they may be discarded quickly in the event that any liquid nitrogen splashes into them. Special containers are required. Cryobiological storage containers are specifically designed and constructed to withstand the extreme temperature variances involved in handling liquid nitrogen. These special containers should be filled slowly to avoid the expansion stress that occurs as a result of the rapid cooling. Too much stress can damage the container. Do not seal the containers. Cryobiological storage containers are designed to function with little or no internal pressure. The use of any tight-fitting stopper or plug that prevents the adequate venting of gas builds up pressure that could severely damage or even burst the container. Even icing or accumulated frost can interfere with proper venting and containers should be checked for such obstructions. Transfer liquid nitrogen with care. The primary hazards of transferring liquid nitrogen from one container to another are spilling and splashing. Special funnels (with the top partially covered) will reduce splashing. For cryobiological storage containers a self-pressurizing discharge device is available that allows controlled liquid nitrogen, withdrawal up to two liters per minute. Always follow carefully the instructions on containers or accessories when transferring liquid nitrogen. NEVER overfill the containers. Filling above the specified level is likely to produce spillage when the neck tube core is replaced. Use solid metal or wooden dipsticks. Because of the extremely low temperature of liquid nitrogen, plastic measuring devices tend to become very brittle or even shatter. NEVER use hollow rods or tubes; the gasification and expansion of the rapidly cooling liquid inside the tube will force liquid to spurt from the top of the tube. Always wear insulated or heavy gloves when measuring. Nitrogen gas is colorless, odorless, tasteless ... and deadly! It reduces the concentration of oxygen and can cause suffocation. Since it cannot be detected by sight, taste or smell, it may be inhaled as if it were air. That is why liquid nitrogen must always be stored and used ONLY in areas that are fully ventilated. As liquid nitrogen evaporates, the resulting nitrogen gas displaces the normal air-and breathing air that is less than 18% oxygen may cause dizziness, unconsciousness and even death. Nitrogen gas is extremely cold. The eyes can be damaged by exposure to this gas even when the contact is too brief to affect the skin. 38 Handle containers with care. Containers should always be stored in an upright position. Tipping the container or letting it lie on its side can result in spillage and may damage the container or the materials stored in it. Walking or dragging containers could result in a partial or complete vacuum loss. For containers that cannot be easily and safely carried, a roller base can provide safe and easy movement of containers. Container Contents. The extremely low temperature of the liquid nitrogen provides the protection of the materials stored in cryobiological storage containers. When all of the liquid nitrogen has evaporated, the temperature inside the container will rise slowly. The rate of evaporation depends upon the age, condition and use pattern of the container. Opening and closing the container or moving it about will reduce its cooling efficiency. You should check the liquid nitrogen level in your containers at least weekly; make sure there is enough liquid nitrogen in the container to maintain the required temperature to avoid damage to the ampules, canes, straws or vials stored in the container. If the liquid has evaporated faster than usual or if the container is covered with frost or condensation, the vacuum system may be damaged. In such instances, transfer the contents to another container and remove the damaged one from service. Ultraviolet light UV lamps in biological safety cabinets are no longer recommended or supported by UMOSEH. When the lights are working properly, they emit radiation at 254 nanometers, which is can kill infectious agents on the interior surfaces of the cabinets. This wavelength also happens to induce tumors in laboratory rodents and presents an occupational hazard to laboratory workers. Visualization of DNA often involves the use of UV light. Ethidium bromide fluoresces under UV light. The lamp used to generate the UV light is usually a mercury arc lamp. The primary emission of the light is 354 nm. There are other emissions from the visible range (400 nm+) down to and below 254 nm. The most hazardous region for human skin is 270-310 nm. Some mercury arc lamps put out a significant portion (20-30%) of their power in this range. To reduce exposure employees should not use the lamp facing up. While using the lamps, wear a protective face shield and cover exposed skin. The effects of UV are erythema (red skin), photokeratitis (small lacerations of the cornea, or “welder’s flash) and skin cancer. When using a UV microscope personnel must wear protective goggles or glasses. In addition, anyone else in the room during such use should also wear similar protective equipment. 39 Electrical Hazards Electrical hazards can be present in electrophoresis because electricity is fundamental to the process. New electrophoresis machines come with UL and CE designations. These pieces of equipment have past stringent tests for electric shock protection. If the electrophoresis machines do not have these approvals, the operator must ensure that no exposed live wires or contact are exposed. A ground fault interrupter (GFI) can be added to automatically shut off the electricity in the event of an electrical fault. The voltages used for electrophoresis are sufficient to cause electrocution. Cover the buffer reservoirs during electrophoresis. Always turn off the power supply and unplug the leads before removing a gel. Gel Electrophoresis The major hazards of gel electrophoresis are related to the chemical and physical agents. DNA is separated using gels (mainly agarose), a buffer solution, and an electric field (80110 volts). Ethidium Bromide Ethidium bromide is a moderately toxic chemical. It has been shown to be mutagenic. Most suggest handling ethidium bromide as a carcinogen. No skin contact is permitted. When working with ethidium bromide, try to minimize the potential for spills. Where practical, purchase ready-made stock solutions from chemical manufacturers in lieu of mixing your own solutions. If you prefer to mix your own solutions of ethidium bromide, protect yourself by doing this process in a fume hood. Perform all processes that generate ethidium bromide dusts or mists inside the fume hood to minimize inhalation exposures. Prevent accidents by transporting small quantities of ethidium bromide in a secondary container instead of carrying large quantities. Acrylamide Acrylamide is a common research laboratory chemical. Widely used as a cross linking agent for electrophoresis separation procedures, acrylamide is a basic requirement for various biochemical techniques. This familiarity may cause some lab personnel to overlook the hazardous nature of this toxic substance. Acrylamide is a powerful central and peripheral nervous system toxicant. Acute (short-term) exposures to low levels of the monomer can damage nerves and cause effects such as drowsiness, lack of coordination, hallucinations, and confusion. Chronic (long-term) exposures can cause severe nerve damage and result in sensory and motor impairment marked by numbness and weakness in the hands and legs, and difficulty walking and speaking. Based upon a number of laboratory and epidemiological studies, the U.S. EPA has classified acrylamide as a probable human carcinogen. All measuring, mixing, and handling of the acrylamide monomer should take place in a chemical fume hood while wearing latex gloves, which extend over the cuffs of the lab 40 coat. Once the monomer has polymerized it is no longer hazardous, however, since there is never 100% polymerization, there will always be toxic monomer contamination. For this reason polymerized gels should be treated with the same caution as the monomer. Elimination of the hazardous powder is one of the best methods to decrease the risk of acrylamide exposure in the lab. Where practical, purchase pre-mixed acrylamide solutions available from various vendors. These solutions have the added advantage of being specifically designed for each application and can provide a high level of purity and reproducibility. Additional Chemical Usage Phenol Phenol is a very caustic organic solvent that is used to extract protein from DNA preps. Phenol can be readily absorbed through the skin, whereupon it can affect the central nervous system and cause damage to the liver and kidneys. It is also a mutagen, and there is some evidence that phenol may be a reproductive hazard. When heated, phenol will produce flammable vapors that are highly toxic and explosive. Whenever possible, work with phenol in a chemical fume hood, especially when heating it. Never heat or melt phenol in an incubator, microwave, drying oven, or similar appliance. Prevent phenol from contacting skin by wearing neoprene gloves and a laboratory coat. Change gloves frequently. Wear chemical goggles to protect the eyes. Always wash hands thoroughly after handling phenol, even if gloves are used. Chloroform Chloroform is widely used in molecular biology as a solvent in organic extraction. It has been shown that generation of phosgene from chloroform has occurred with or without the exposure to flames, electrical arcs, intense sunlight and hot surfaces. Recently it has been suggested that over time chloroform can break down and form phosgene in older, particularly unstabilized, chloroform containers. Researchers should purchase stabilized chloroform whenever possible. Although amylene is used as a stabilizer, there is evidence that it may not prevent phosgene generation. If unstabilized chloroform is necessary for your work, you must treat it like peroxide forming compounds; dated when received, used quickly, and discarded after a year. If you have opened unstabilized chloroform that has been in the laboratory for more than one year, you should discard it as hazardous waste. Storing chloroform in a dark place (cabinet) in an amber bottle can reduce the rate of chloroform decomposition. 41 Equipment Maintenance 1) Autoclaves, centrifuges, biological safety cabinets, and fume hoods should undergo regular preventative maintenance by qualified personnel. 2) The airflow must be regularly checked on the biological safety cabinets and filters change by qualified personnel. If cabinets are not functioning correctly, contact OSEH (647-1143) to perform maintenance operations. 3) Preventative maintenance records should be kept on all equipment. Cleaning and Decontamination Housekeeping 1) General laboratory Procedures All areas of the (BSL Level) laboratory must be kept clean and orderly. Dirt, dust and clutter are safety hazards and are not consistent with acceptable biological research. Stock solutions of disinfectants should be maintained at each bench top and biological safety cabinet work area: 1. Bleach, 10% sodium hypochlorite 2. Ethanol, 70% solution 3. Other appropriate disinfectants Vacuum lines should be protected by a disinfectant trap (an aspirator suction flask containing bleach) and a HEPA filter between the vacuum port and the aspiration flask to prevent pathogens from entering the vacuum system. All infectious materials, contaminated plastic ware/glassware, and contaminated waste will be disinfected prior to washing or disposal. Contaminated materials are to be placed in sealed clear biohazard bags with red or orange lettering indicating biohazard and printed-on sterilization indicator badge prior to autoclaving. Surfaces are to be decontaminated after each use. The Lab Manager or other laboratory personnel should conduct periodic inspections of the (BSL Level) Laboratory. A copy of a BL2 Recombinant /Infectious Agent Laboratory Audit Checklist can be found on OSEH’s homepage at http://www.umich.edu/~oseh/BL2checklist.pdf for the laboratory’s use. OSEH recommends that inspections be performed and recorded every six months. Records of these inspections should be kept in appendix 5. 42 Chapter 7 – Radiation Management Use of Radioactive Isotopes All personnel working with radioactive materials should be instructed in the use of necessary safeguards and procedures and all visitors should be informed of pertinent precautions to be taken. All personnel and visitors should be supplied with such auxiliary devices as may be necessary for protection. This includes devices such as: 1. Lead or Plexiglas© 2. Radiation badges, rings, gloves, and 3. Radioactive spill cleaning materials The radiation safety coordinator should ensure that every visitor has proper authorization and should recommend that no unnecessary visit to areas involved with radioactive use be made. Radioactive material should be prevented from leaving the jurisdiction of the radiation safety coordinator under circumstances that may subject other personnel to radiation in excess of the limits prescribed by the OSEH Radiation Safety Service. All areas that are to be used for radioactive work must be clearly labeled with the appropriate radiation hazard signs. Contact OSEH, Radiation Safety Service at7644420 for further information. Measures should be taken to ensure that no modification of equipment or installations that might lead to unforeseen radiation hazards is made without provision of the appropriate safeguards. Measures should be taken to ensure that no radioactive material is used by unauthorized personnel who do not have the required training to use the radioisotopes. The radiation safety coordinator must keep concise and up-to-date records of usage, inventory, and disposal of radioisotopes. Any accident, unusual incident, or personal injury, must be reported to the radiation safety coordinator, OSEH Radiation Safety Service, and the Principal Investigator or Lab Manager. Areas where radioactive isotopes are used should be routinely monitored by systematic swipe sampling and sample analysis via a scintillation counter. Shielding 43 1. Radiation emitted from isotopes must be shielded away from the user. 2. When working with 32P, the radiation may be shielded behind a ½ to ¾ inch Plexiglas © shield. 3. When working with 125I, lead must be used to shield the worker from radiation. 4. Contact OSEH, Radiation Safety Service at 764-4420 for any questions regarding shielding. Disposal of Isotopes after Usage When working with potentially infectious agents, any radioactive reagents coming in contact with the biohazard must first be immersed in bleach prior to being discarded into a radioactive waste bag or container. Note: Do Not Use bleach with 125I as it produces a volatile form of the isotope. It is imperative that all potentially infectious waste be disinfected with bleach prior to disposal. 44 Chapter 8 - Emergency Management Emergency Procedures The fundamental rule in dealing with a biological spill is to be prepared. Preparation involves identification of the biohazard risks, both actual and potential, that are involved on the site and determining the types of potential spills or emergencies which can occur. In order to prepare for a biohazard spill, you must first: Know the ventilation system serving the laboratory or room, the corridors and the building in order to enable you to know how aerosols or airborne particles would move; Know where fume hoods and biological safety cabinet exhaust ducting goes after leaving the lab area; Know where biohazard areas are and where biohazardous materials are stored and assessed and what hazard could result in the event of a fire, flood, or explosion; Establish evacuation routes and procedures to be used in the event of an emergency with biohazardous materials; Establish rules for safe handling, storage and disposal of biohazardous materials to minimize accidental release and set standards for use to avoid conditions which might lead to an accidental spill; Establish a standard operating procedure (SOP) to be followed if a spill should occur. This SOP would consist of a step-by-step procedure to follow if a spill occurs. Spill kit materials should be present in proximity to the area where biohazardous materials are handled; Know the occupational medical services' procedures for reporting and dealing with exposure to biohazardous materials. Accidental Exposure to an Infectious Agent Laboratory personnel who are accidentally exposed to a potentially infectious agent must report the incident as soon as possible to the Principal Investigator and the OSEH Biological Safety Officer (763-3133). The Principal Investigator will see that necessary treatment or health monitoring is obtained without delay. University of Michigan Occupational Health Services (C380 Med Inn Building 734-764-8021) will provide follow-up and counseling on risk of infection and its consequences. The Work~Connection Employee Illness or Injury Report form must be completed for all workplace injuries and illnesses (see Appendix 7). 45 Spill Response Procedures for Infectious agents and Recombinant DNA Spills and accidents should be immediately reported to the Principal Investigator and the Department of Occupational Safety and Environmental Health (OSEH) (6471143). Large Spills Outside of the Biosafety Cabinet OSEH will respond to large spills (greater than 200 ml) of BSL-2 (or above) containment level material. Contact OSEH (647-1143) for help with large spill cleanup. Small Spills Outside of the Biosafety Cabinet 1. Don double gloves and eye protection if not already wearing them. 2. Cover spilled material with an absorbent paper towel or Kimwipe. Once the absorbent material is in place over the spill, wet the material with a 10% solution of bleach (1:10 dilution of Clorox containing sodium hypochlorite) or other appropriate disinfectant. 3. Let stand 15-20 minutes, wipe up and wash surface with appropriate disinfectant. 4. Wipe down all equipment and surfaces which may have been splashed. Spill in a Biosafety Cabinet Note: Leave the cabinet turned on. 1. Don double gloves, a lab coat, and eye protection if not already wearing them. 2. Cover spilled material with an absorbent paper towel or Kimwipe. Once the absorbent material is in place, wet material with 10% solution of bleach (1:10 dilution of Clorox containing sodium hypochlorite) or other appropriate disinfectant. Let stand 15-20 minutes, wipe up and wash surface with appropriate disinfectant. 3. If personnel are contaminated, remove potentially contaminated garments at the BSC and decontaminate garments by saturation with 70% ethanol or place in autoclave bag for autoclaving. Wash hands and other potentially exposed skin surfaces thoroughly with soap and water. Don fresh PPE, return to worksite, and spray walls, liners, and equipment with an appropriate disinfectant. 4. Spray or wipe container walls, other work surfaces and equipment with the appropriate disinfectant 46 5. If necessary, flood the work surface, drain pan and catch basin below the work surface with disinfectant. Allow at least 15-20 minutes contact time. 6. Soak up the disinfectant and drain the catch basin into a container. Lift the front exhaust grille and tray and wipe all surfaces. Ensure that no foreign materials are blown into the area below the grille. 7. If a 10% bleach solution is used on metal surfaces, rinse with water or 70% ethanol after decontamination is complete. 8. If the spill overflows into the interior of the cabinet, more extensive decontamination of the cabinet may be necessary. Contact OSEH (763-6973) for decontamination of the cabinet. Spill in the Laboratory 1. If an infectious aerosol may exist outside of a biosafety cabinet, leave the room immediately, lock the door, post a warning sign and inform your supervisor. If clothing is contaminated, remove and turn the exposed side of fabric in on itself and place in autoclave bag or biohazard container. Wait at least 30 minutes before reentering the lab to allow dissipation of aerosol created by the spill. During this time, review clean-up procedures, assemble decontamination materials, PPE and contact OSEH (647-1143). 2. Don fresh gloves, a lab coat or tyvek suit, and eye protection. 3. Carefully lay disinfectant-soaked towels over the spill and pour more around the spill. Use more concentrated disinfectant if the volume of material will significantly dilute the disinfectant. 4. Allow 15-20 minutes contact time. 5. Use forceps to place sharp objects into a sharps container. Using a dustpan and dustbroom, tongs, etc., transfer all contaminated materials (paper towels, gloves, labware, etc.) biohazard waste containers and contact OSEH HazMat (763-4568) for removal. 6. Wipe surrounding surfaces with disinfectant to cover all splash areas. Wipe flat surfaces to remove any material that may have splashed out and settled on those surfaces. 7. Place all contaminated materials, including protective clothing, into an autoclave bag or biohazard waste container. 8. Wash hands with soap and warm water. 9. If a personnel exposure occurred, complete an Illness or Injury Report form (https://www.workconnections.umich.edu/illnessorinjury.php) summit to 47 Work~Connections and report incident to OSEH (763-6973). See additional procedures noted below. Skin, Mucous Membrane, or Injury Exposure 1. If there is an agent-specific protocol for exposures, follow that (e.g., HIV, Herpes B). 2. In the case of skin contact or injury with a contaminated instrument: a. Thoroughly wash area with soap and water. Do not squeeze the wound to induce bleeding. b. Avoid use of abrasive chemical soaps or disinfectant washes as they can cause skin abrasions and a possible additional route of entry for the agent. c. For mucous membranes (e.g., eyes, mouth), flush for a minimum of 15 minutes. 3. Notify UM-Occupational Health Services (OHS) for evaluation of exposure following: a. Contact with mucous membranes; b. Contact with non-intact skin; c. Percutaneous exposure; or d. Any type of exposure that involves concentrated virus. U-M Occupational Health Services -- Campus Employees Mon-Fri 7:30 am – 4:30 pm C380 Med Inn building 1500 East Medical Center Drive, Ann Arbor (734) 764-8021 begin_of_the_skype_highlighting After hours - go to UM Hospital Emergency Dept. – Urgent Care Clinic 5. Complete an Accident-Illness Report Form (https://www.workconnections.umich.edu/illnessorinjury.php) submit to Work~Connections and report incident to OSEH (647-1143). For exposures to recombinant DNA, perform the following: 1. Any situation involving recombinant DNA that poses a threat to an individual's health, safety, or welfare should be handled with the appropriate care including emergency response (911) if necessary. 2. Wash the area thoroughly with soap and water. 48 3. Cover the wound with a sterile dressing. 4. Following this, reporting must occur to: Principal Investigator or Director of Lab (immediately) Biosafety Officer (647-3133) (immediately) Complete an Accident-Illness Report Form (https://www.workconnections.umich.edu/illnessorinjury.php) submit to Work~Connections (within 24 hours) IBC (may be reported through the Biosafety Officer) NIH/OBA (report will be coordinated by the IBC) Fire Fighting Procedures Personal safety is each worker’s primary concern in the event of fire 1) Upon learning of the threat of fire within the building, laboratory personnel will, to the extent possible: 2) Turn of all gas burners, biological safety cabinets, electric motors, and other electrical equipment. Place containers of infectious materials into autoclaves, incubators, refrigerators, freezers or other storage areas. Leave the laboratory as quickly as possible using designated fire evacuation routes. Personnel should be trained by OSEH Fire Safety Services in the operation of fire extinguishers (615-6764). Reporting and Recordkeeping Accidents and spills occurring outside the biological safety cabinets will be reported and accident report forms will be filed under Appendix 7. 49 Chapter 9 - Shipment and Receipt of Infectious Materials General Procedures for receiving and unpacking infectious materials must be established by the labs receiving these materials. Employees who have responsibilities that include the receipt of packages must be given specific instructions regarding the receipt of infectious materials and should be trained and qualified to recognize the hazardous nature of the material being received and recognize whether or not the material has been packaged, labeled and manifested or documented appropriately. This constitutes an audit function for regulatory compliance. Any given package may receive several such audits and visual inspections along its shipping route. Receipt of Infectious Materials Shipments of hazardous materials must be received (generally) by those to whom it is addressed. This is most easily accomplished via a certified carrier such as Federal Express. University Mail Services is certified to accept and transfer hazmat packages from the U.S. Postal Service (USPS). Employees should receive shipments in a designated and secure area of the laboratory. This person should have at-hand and utilize all appropriate personal protective equipment and containment devices (biological safety cabinet or chemical fume hood). Before accepting, the parcel should be carefully inspected for leakage indicated by broken or improperly sealed containers. If the package is rejected (not accepted) due to leakage or other damage, the carrier will work with the shipper to resolve the problem. If the shipment is critical and must be accepted, OSEH should be contacted at 763-6973, and further activities should be conducted with care in a containment device. All contaminated materials should be collected for proper disposal through consultation with OSEH. Employees must review and sign the Training Sheet for the Receipt of Biologics. http://www.oseh.umich.edu/Transportation_of_Biologics_Appendix%20I.pdf . Signed sheets should be faxed back to OSEH (763-1185). Transportation of Biohazardous Materials General All shipments of infectious or diagnostic specimens must be packaged, labeled, and transported in conformance with all applicable local, federal, and international transportation and shipping regulations, including U.S. Department of Transportation (DOT) regulations. Materials that are transported by airline carrier will also comply with packaging and shipping regulations set by the International Air Transport Association (IATA). Personnel who are involved in the preparation, packaging or shipment of infectious substances, biological materials, human/ animal specimens, genetically 50 modified microorganism or any shipment involving the application or use of dry ice must be trained and certified by OSEH. Classes are scheduled monthly and held at the OSEH office. Registration is available at http://www.osehtraining.umich.edu/osehtraining/ . NOTE – this training is required every two years. On-Campus Transportation Packaging The materials must be properly packaged for transport (similar to how you would package them if they were going by courier). For liquids, the inner packaging must be leak proof, and the outer packaging must contain sufficient absorbent material to absorb the entire contents of the inner packaging. For solids and liquids, the outer packaging must be a strong, tight packaging securely closed and secured against movement. The outside of the secondary container must be free of any biohazardous material so that the package can be carried safely between buildings without wearing gloves or lab coats outside. The package must be taken directly to its intended location. If a spill occurs during transport, do not attempt to clean it up without appropriate spill response material and PPE. Keep other persons clear of the spill. Contact OSEH (647-1143) for additional assistance. Hand Carry Between University Labs or Buildings Infectious substances must be transported or moved between laboratories in way as to prevent spills and accidental exposure or release including: Placing material in a primary (specimen) container that is leak-proof and secured with a tight-fitting cap, parafilm, or lab tape. Placing absorbent material (diapers, absorbent towels, pads) around the primary containers for transport of liquids. Placing the primary containers in a secondary transport container that is also sealed and labeled with a biohazard symbol. These materials may be moved on a cart or other device between rooms or buildings. Transport by University Vehicle Unregulated or exempted biological materials may be transported either on campus or to off-site research locations for university business in a university vehicle as long as they meet all packaging, labeling, and training requirements. OSEH does not recommend use of a personal vehicle for transporting materials off campus. Insurance companies may not cover an accident where hazardous materials were transported in a personal vehicle. A university or city of Ann Arbor bus or shuttle cannot be used for the transport of infectious substances or other biohazardous materials. 51 For materials that qualify for transport in university vehicles, the following precautions should be followed: Must have a valid driver’s license Must have authorization to use a university vehicle All materials must be packaged according to a triple packaging system or more restrictive packaging requirements. Hazardous materials should be transported in the trunk, or as far away from passengers as possible. All containers should be clearly labeled with content information. A complete inventory of the material must accompany the package. The vehicle must be driven directly from the point of origin to the intended destination without stopping at other locations on the way. Materials needed to contain or clean-up a spill, such as sorbent pads, gloves, and eye protection, should be available in the vehicle. Off-site Transportation by Courier Biohazardous materials which are to be transported off-site from a facility by a courier must be shipped in accordance with the appropriate DOT or International Regulations. The following information must be known prior to shipment: The infectious agent name; The amount of material to be transported (milliliters or ounces); The name and address of the shipper and the consignee. The material must then: Be packaged in accordance with the appropriate regulation(s); Be labeled in accordance with the appropriate regulation(s); Be accompanied by the appropriate documentation as required; Be transported by an authorized carrier. 52 Chapter 10 – Appendices The following forms and diagrams are referenced in the text of the Laboratory Biosafety Manual. Included in the Appendices are: 1) 2) 3) 4) 5) 6) 7) 8) 9) Emergency Call List Schematic of laboratory Roster of approved laboratory personnel and training records Training Completion Form Housekeeping Logs PSDS Sheets for Infectious Agents Located in Laboratory Accident Report Forms Recombinant DNA Registration Form Standard Operating Procedures Template 53 Appendix 1 Emergency Call List Name Work Phone Home Phone Lab personnel OSEH Janet Follo UM Biological Safety Officer, OSEH 647-3133 Terry Alexander Director UM OSEH 647-1143 Mark Driscoll UM Radiation Safety Officer, OSEH 764-4420 54 Appendix 2 Schematic of Laboratory 55 Appendix 3 Roster of Approved Personnel and Training Records Personnel Type of Training Date Completed Signature of Trainee Detailed list of training materials 1) 2) 3) 4) 5) UM OSEH, Radiation Safety Training Course UM OSEH, Biological and Laboratory Safety New-Hire Training Course DOT shipping of Infectious and Diagnostic Specimens (if applicable – contact OSEH at 3-6973)) ULAM Training (if applicable – contact ULAM at 4-4420)) Reading List Laboratory Biosafety Manual CDC/NIH Biosafety in Microbiological and Biomedical Laboratories UM, OSEH Biohazardous (Medical) Waste Disposal Guideline Laboratory Safety Practices for Progress 56 Appendix 4 Training Completion Form RECOMBINANT DNA/INFECTIOUS AGENT TRAINING Name _____________________________Department__________________ Campus Location ___________________ Campus Phone________________ Employee Classification _____________ Supervisor ___________________ All employees working with recombinant DNA or infectious agents are to be provided with biosafety training at the initial assignment to tasks where occupational exposure may take place and annually thereafter. Lab specific training appropriate to the skill level required for the employee to perform their job safely will be conducted for lab personnel by the lab supervisor or other qualified personnel. Prior to initiating research, the Principal Investigator shall: 1. Make available to all laboratory staff the protocols that describe the potential biohazards and the precautions to be taken. 2. Instruct and train laboratory staff in the practice and techniques required to ensure safety and the procedures for handling spills. 3. Inform laboratory staff of the reasons and provisions for any precautionary medical practices advised or requested (e.g., vaccinations or serum collection) In addition, each lab is required to develop a laboratory biosafety manual, which includes laboratory specific work practices and procedures to ensure that employees are protected from all potentially infectious materials or recombinant DNA. New employees must review this document and associated training materials. Training should be documented. By your signature below, you acknowledge that you have read and understood the contents the biosafety manual and standard operating procedures and know its location within the laboratory. ________________________________________________________________________ Employee Signature Date Document specific employee training below: 57 Description of Training Date Provided By A copy of this form should be maintained in the laboratory's Biosafety Manual. Training Checklist This checklist may be used to assist employers with the laboratory specific training requirements for work with infectious agents or recombinant DNA. Introduction to laboratory specific Biosafety Manual: Location and contents Introduction to laboratory specific Standard Operating Procedures (SOP’s) Review description of the Principles of Biosafety, Principles of Good Microbiological Practice and Universal Precaution. Review modes of transmission, epidemiology and symptoms of pathogenic microbes Review emergency information: Spills, Personal Injury, Fire, and Power Failure Accident reporting and investigation procedures Spill control and clean-up Fire extinguisher First Aid Supplies Evacuation Plans 58 Basic Safety Rules Note rules with special importance for your laboratory. Identify specific areas for food consumption. Review procedures for working after hours. Review the inventory of biohazardous materials for your laboratory Review the UM (OSEH) Waste Handling Procedures Autoclaving (bags, periodic monitoring, preventative maintenance, log) Chemical Disinfection Sharps Disposal Review procedures for procurement, distribution, and storage Review Standard Operation Procedures for use of biohazardous materials Storage (freezer, refrigerator, etc.) Personal Protective Equipment (PPE) Location of procedure (biological safety cabinet, laboratory bench) Waste Disposal (aqueous, solid, biohazardous, radioactive) Review procedures for use of compressed gas cylinders Protective Apparel and Equipment (PPE) Discuss when safety glasses, goggles, or face shields are required. Discuss any need for other protective equipment (aprons, mask, shoe covering) Discuss selection of gloves (latex, cold/hot environments) Discuss disposal procedures for PPE Housekeeping, Maintenance, and Inspections Discuss materials stored or frequently present on the floor. Discuss maintenance items for scientific equipment. Discuss formal and internal inspection programs. Discuss recordkeeping requirements for the lab. 59 Environmental Monitoring Discuss building ventilation. Discuss use of fume hoods, biological safety cabinets or other mechanical ventilation systems. Review SOP’s for working with biologically hazardous materials Review Exposure Control Plan if working with human blood or other potentially infectious materials. Review Hepatitis B Vaccination Program Working with Radioisotopes Review radiological safety practices Review Dosimetry Program Review waste disposal procedures (including waste that may be both radioactive and infectious) Medical Program Discuss need for any medical surveillance (Respirator use, Potentially Hazardous Materials, Animal Handler, Tb, etc…) Discuss vaccinations, if applicable (Hepatitis B, Training Program Discuss laboratory-specific training and OSEH training sessions Additional Safety Session Topics Review recent incidents/accidents/injuries and how to prevent reoccurrence. Review new equipment at least annually. Review new procedures at least annually Review results of recent inspections and how to correct problem areas. 60 Appendix 5 Housekeeping Inspections This section should contain information on laboratory inspections (including the date and recommendations). Inspections may be conducted by the laboratory, OSEH, MIOSHA, NRC, and possibly other organizations. This section should also contain records associated with corrective actions. Laboratories conducting recombinant DNA work at Biosafety Level 2 (BL2) or Biosafety Level 3 (BL3) must be inspected by UM OSEH prior to the initiation of the work and on a regular basis thereafter. The items that OSEH will review during their inspection, as a minimum, are contained on their BL2 Recombinant Laboratory checklist. Key items are proper employee training, availability of a completed Biosafety Manual, and appropriate written procedures. 61 Appendix 6 Pathogen Safety Data Sheets for Infectious Agents PSDS sheets on infectious agents (Office of Laboratory Security) can be found at the following address: http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/index-eng.php Additional PSDS Sheets for the following materials can be obtained by request (6471143). Adenovirus Type C Strain 5 and Recombinant Vectors Moloney Murine Leukemia Virus (MoMuLV) Recombinant Vectors Adeno-Associated Virus (AAV) Serotype 2 Recombinant Vectors Respiratory Syncytial Virus (RSV) Adenovirus Fact Sheet 62 Appendix 7 Accident Report Forms Keep Copies Here Forms available at: http://www.workconnections.umich.edu/forms.html 63 64 Appendix 8 Standard Operating Procedure EXAMPLE ONLY!!! Laboratory Standard Operating Procedure (For the use of biohazardous materials or equipment) Name of Procedure: Working with biohazardous materials in general (Insert agent name(s) here) Prepared By: John Doe Revision Date: Insert Date APPROVALS - Experiments using recombinant DNA require approval from the UM- Institutional Biosafety Committee (IBC) before initiation of experiments. The use of infectious agents is reviewed by OSEH. CONTAINMENT LEVEL – Biological agents may be contained at varying biosafety levels. The IBC will assign the appropriate containment level for the lab and animal work involving recombinant DNA projects. OSEH will assign the appropriate lab and animal containment level for the use of infectious agents. LOCATION - This procedure may be performed at the following location(s): Procedures are performed in Lab (insert lab locations, include animal procedure rooms, surgery rooms or housing areas if applicable) in the biological safety cabinet. The biohazardous materials are stored in a (freezer, refrigerator, incubator) located in room (insert room location) HAZARDS - The following materials and equipment associated with this procedure presents exposure or physical health hazards. Safety precautions are prudent and mandatory: Eyewash/Safety shower is located (insert room location). Remove contaminated clothing and vigorously wash exposed area with soap and water for 10 minutes. Obtain immediate medical attention. Report the incident to the Laboratory Director. See Chapter 7 of the Biosafety Manual for additional information on Emergency Management. ENGINEERING CONTROLS - Prior to performing this procedure, the following safety equipment must be accessible and ready for use: (ex. biological safety cabinet, laminar flow hood, biological disinfectant) Biological safety cabinet is located in (insert room location). Perform all work that may create an aerosol in the biological safety cabinet. The concentrated stock of biological disinfectant is located in the cabinet 65 labeled disinfectant in room 00. Dilute stock solutions are located in the (tissue culture room, biological safety cabinet, in cabinet) PERSONAL PROTECTIVE EQUIPMENT - Prior to performing this procedure, the following personal protective equipment must be obtained and ready for use: (ex. Disposable gloves, safety eyewear, lab coat, apron) Wear gowns, lab coats, aprons or similar protective clothing. Wrap around outer clothing when introducing biological agents into animals or performing necropsies. Lab coats are adequate for tissue culture manipulations. Wear fluid-resistant clothing if there is a potential for splashing or spraying of blood. Wear gloves for all blood and tissue sample collection.. Wear disposable (single use) latex or nitrile gloves. Gloves are located in (insert room location). Replace gloves as soon as possible when visibly soiled, torn or punctured. Wash your hands or any other contaminated skin with soap and water immediately or as soon as possible after removal of gloves and after visible contact with blood or other potentially infectious materials. Use facial barrier protection whenever splashes, spray, droplets, or aerosols may be generated (NOTE: Opening containers creates aerosols). Face protection may include the following: hood sashes, shields, masks and safety glasses, or chin-length face shields. Perform work in a biosafety cabinet when working with aerosols. Remove all PPE immediately upon leaving the work area and as soon as possible if overtly contaminated. Contaminated PPE will be DISPOSED of as biohazardous waste or decontaminated. Animal Use - Approvals are needed from the University Committee on the Use and Care of Animals (UCUCA) and the Institutional Biosafety Committee (IBC) ( if involving rDNA) Perform inoculations carefully to reduce the possibility of creating splashes or aerosols. Ensure appropriate PPE is worn according to the procedures posted in the animal room. All PPE is single use and should be disposed of in the designated waste containers upon exiting the ULAM space. Used needles must be disposed of in an approved sharps container immediately after use. Used needles should not be set on the bench, sheared, bent or re-capped prior to disposal. Whenever feasible, self-sheathing needles should be used to avoid the potential for accidental needle stick injuries. Restraint devices and practices should be used to reduce the risk of exposure during animal manipulation and administration should take place inside a certified biosafety cabinet. All lab staff who will be administering biological materials to animals must receive appropriate training. OSEH will review the protocol details and recommend the appropriate housing. Employees may be required to complete the ULAM Hazard Containment and Hands-On Training if Animal Containment Housing is recommended by OSEH. Employees must follow ULAM Containment Policies and Procedures SOP if Containment Housing is indicated. Arrangements must be made with OSEH for proper disposal of animal carcasses. WASTE DISPOSAL - This procedure will result in the following regulated waste, which must be disposed of in compliance with environmental regulations: Sharps- Dispose of sharps such as needles, broken glass, scalpels in labeled, hard walled containers such as the five gallon pails available from Stores. Label with an “infectious substance” marking. Call for pick-up by HazMat (3-4568). Solids- Place solid waste such as laboratory coats in special biohazardous waste boxes available from HazMat or 55 gallon fiber drums labeled as infectious substance.” Call for pick-up by HazMat. Liquids- If disinfected with bleach, blood and blood products can be poured down the drain. If the biohazardous liquid waste contains other chemicals besides bleach, manifest as chemical waste and call HazMat for pick-up. 66 Autoclaved Waste- Place waste that will be autoclaved in clear autoclave bags that have an indicator badge that turns black once the waste is autoclaved. Do not put sharps or standing liquids in autoclave bags. ACCIDENTAL SPILL - In the event that a hazardous material spills during this procedure, be prepared to execute the following emergency procedure: If a small spill, alert people in the immediate area of the spill. Put on protective equipment. Cover the spill with paper towels or other absorbent materials. Carefully pour a freshly prepared 1 in 10 dilution of household bleach around the edges of the spill and then into the spill. Avoid splashing. Allow a 20-minute contact period. Use paper towels to wipe up the spill, working from the edges into the center. Clean the spill area with fresh towels soaked in disinfectant. Place towels in a sealed container and put an “infectious substance” marking on the container. Report the spill to the Laboratory Director. If a large spill, evacuate the lab and call HazMat at 3-4568 for proper clean-up. PRIOR APPROVAL - This procedure is considered hazardous enough to warrant prior approval from the laboratory director. YES / NO ADDITIONAL PRECAUTIONS & REFERENCES – CERTIFICATION - I have read and understand the above SOP. I agree to contact my Supervisor or Lab manager if I plan to modify this procedure. Signature Name (Print) Date Room # 67 Appendix 9 Autoclave Use Log 68 Autoclave Use Log Form Record daily waste runs or monthly performance runs in log Bldg location of autoclave & Rm# Lab Bldg/Rm# Autoclave operator (name & lab ph #) Run date/Cycle time: e.g. 01-12-13 45min cycle Load description: # of bags, agar plates Cycle Used Gravity/Fast ex Liq/Slow ex Autoclave contact Name - number Chemical Integrator Pass/Fail Biological Indicator Pass/Fail Additional comments (please include: date of concern/comment, operator name, and date person contacted regarding concern) 69 70