Biosafety At the University of Ottawa
advertisement
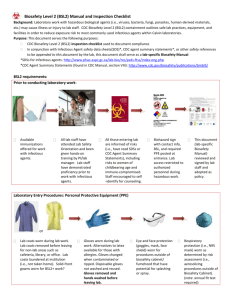
Lois Sowden-Plunkett Sept, 2012 Office of Risk Management http://www.uottawa.ca/services/ehss/biosafety.htm 1. Challenge your understanding 2. Establish good laboratory practices 3. Prevent contamination (you and your work) 4. Ensure research funding Because research is now continues $$$ interdisciplinary, it is now necessary to retool yourself with new skills and new understanding. BIOHAZARD BIOSAFETY BIOSECURITY BIOSURETY A potentially infectious agent or hazardous biological material that presents a risk or potential risk to the health of humans, animals, plants, and the environment CFIA, PHAC, EC, DFAIT, TC, TRICOUNCIL & OTHER FUNDING SOURCES, NIH.... viruses, bacteria, fungi, parasites, biological toxins, prions, and other micro-organisms or genetic systems, by virtue of their replicative properties, are potentially harmful to humans, animals, plants and/or the environment. Recombinant DNA, cultured cell lines, tissues and anatomical specimens from human or animal subjects, and blood and other bodily fluids are also potentially infectious unless tested and proven otherwise. • found in your intestines • aid in food digestion Extensively used for recombinant DNA application • E.coli synthesize vitamins B1,B2 & K. • do not cause any harm if are in limited number. • deficiencies of these vitamins cause many diseases DH5 alpha BL 21 XL1Blue • beware of your antibiotics which can destroy your E.coli June 2, 2011 World Health Organization Sept 18, 2012 mutation of the E. coli bacteria in Europe E-0157:H4 E-0157:H7 (first reported in 1982) 1,500 sick, 470 have developed a rare kidney failure complication, 18 dead unlabelled and/or unbranded ground beef products available for sale from August 24 through September 16, 2012 P. aeruginosa P. stutzeri P. fluorescens Ubiquitous in the environment Opportunistic affects humans, animals and plants Survival out of host (months on dry surfaces) Risk groups Characteristics Hepatitis B,C & HIV Don’t assume because you know the person there is no risk UPEI June 27, 2012 300 Students at potential risk Don’t even assume you don’t have it. The testing involved a lancet and a receptacle for the blood. If it’s not tested, it’s not safe! The lancets were single use only, but the receptacles were used by several students. UNIVERSAL PRECAUTION The combination of measures employed when handling biohazardous materials to: Protect personnel from exposure to infectious agents Prevent environmental release and contamination It’s good for you, it’s good for the science and it’s the law! Safety Principles: 1. Administrative controls 2. Engineering Controls 3. Practices and Procedures 4. Personal Protective Equipment In practical terms, this means: Training, risk assessments, authorizations, certification of rooms and equipment, appropriated practices, health assessment Measures employed to protect biohazardous materials, or critical relevant information, against theft or diversion by those who intend to pursue intentional misuse. (selected agents, U99, BSE) Physical barriers Buildings, doors, locks, key card access Psychological barriers Security personnel, cameras Monitoring Activities Patrols, monitoring by support staff Personnel Clearance Access to authorized personnel only What is BIOSURETY? Biosurety is defined as the combination of security, biosafety, agent accountability, and personnel reliability needed to prevent unauthorized access. To be safe and compliant it is really quite easy, it’s all about: 1. Diligence 2. Knowing who is responsible 3. Knowing your risk 4. Practicing GMP (good microbiological practice) Chancellor Senate (Academic Issues) Board of Governors (Governance / Management Issues) President & Vice-Chancellor Administration Ctte Vice-President Academic and Provost Faculties - Deans Vice- President Research (PHAC and CFIA Applicant Authority) Assoc. V. P. Research (Delegate of V.P R. & Chair BSC) Vice- President Resource B/G Ctte – Health Safety, & Environment Biosafety Committee ( Assoc. VP Research, Deans, Director ORM, & BSO-Corp. ORM - Director LEGEND: Chairs, Principal Investigators, & Professors – (BMUC Holders) BSO– Corp. (PHAC/ CFIA Lead Contact) ORM- BSO – Corp. ( Assist. Director Radiation and Biosafety) Corporate Governance Academic Research ORM – BSO-Op. (Biosafety Specialist) Management Your faculty, your colleague, PS, PRS, HR ... Federal & Provincial Agencies Municipalities International Funding Agencies So let’s get a hand on this ! Pathogenic………………..Non-pathogenic Naturally occurring……..Manipulated Ubiquitous………………..Evolving/Rare It’s as easy as: 1 -2-3-4 ! Pathogencity Infectious dose Mode of transmission Survival outside host and host range Communicability Immunization Prophylaxis / Treatment WHMIS Class D, division 3 of WHMIS (Poisonous and Infectious Material - Biohazardous Infectious Material) RISK GROUPS: Risk Group 1 Individual Low Community Implications Low Unlikely to cause disease in healthy workers or animals Rarely cause serious human or animal disease 2 Moderate Limited 3 High Low 4 High High May cause serious disease Likely to cause very serious disease Mammalian Cell Lines Untransformed mammalian cell lines - Risk Group 1 MCF-7 (Human breast carcinoma cell line) NIH 3T3 (Mouse fibroblast cell line) Transformed mammalian cell lines – Risk Group 2 HeLa (Human - contains papovavirus) Animal (may be infectious without your knowledge, or were intentionally injected with a pathogen Recombinant DNA In vitro incorporation of genetic material from one cell into another or from one organism to another Level of risk depends on: • the source of DNA being transferred • the vector • the host PRIONS Includes unconventional agents, slow viruses and prions causing progressive neurological diseases ex CJD, BSE, Scrapie Resistant to destruction Precautions: Handle tissues as Risk Group 2 or higher Handle formalin-fixed tissues and paraffin-embedded blocks as if still infectious Follow up-to-date disinfection protocols. Toxins Endotoxins are part of the outer membrane of the cell wall of Gram-negative bacteria. Escherichia coli, Salmonella, Shigella, Pseudomonas, Neisseria, Haemophilus influenzae, Bordetella pertussis and Vibrio cholerae. Tetrodotoxin (TTX) is a potent neurotoxin with no known antidote. CONTAINMENT LEVEL: ROOM INTEGRITY Laboratory locations & access control Air Handling and directional air flow Work Surfaces Agents Used Lab services (water, drains, gas, electrical and safety) ( certification, commissioning) measures required for handling each organism safely in a laboratory setting Specific to the risk group level and amounts being used CL 1, 2, 3, or 4 First line of defence. Ensures protection of personnel and immediate environment from exposure to the infectious agent. ‘Protective envelope’ that infectious agent or animal. Petri dish, vial Biological safety cabinets animal caging equipment encapsulates the Protects the environment external to the laboratory from exposure Includes facility design and operational practices Employs: 1. Directional airflow 2. Air and Drain filtration 3. HEPA Filtration of lab air 4. Pressure differentials 5. Laboratory Design 6. Operational Practices Freezer Incubator Sink Fumehood Coats office Air intake 4 BSC Dead air Basic laboratory Requires no special design features Biosafety cabinets are not required and work may be performed on the open bench. Clinical, diagnostic, research and teaching facilities with level 2 agents. May require a class I or class II biological safety cabinet Emergency plan Access controlled Containment Level 3 Specialized design and construction including commissioning and annual certification Research projects reviewed by a specific panel Standard operating procedures enforced for the safety of the individual and proper operation of the lab. Personnel – additional training and supervision. Canadian Centre for Human and Animal Health in Winnipeg, Man. Design specifications are extremely stringent The worker is completely isolated from infectious material. personnel security clearance and qualifications scrutinized Only 20% can identify the cause or event 80% are caused by human errors 20% are caused by equipment failure Types of accidents causing LAIs Spills and sprays Needles Vaccinia virus Sharp objects and broken glass Bites or scratches from animals Pseudomonas Attenuated – Lab Adapted Strains Laboratory-Acquired Infection With an Attenuated Yersinia pestis Strain—Chicago, Illinois, 2009 1 2 3 4 5 • Agent characteristics & biological material • Personnel supervising & personnel using the material • Environment: laboratory, facility, community • Experimental protocols & lab practices equipment • Equipment Agent characteristics & biological material Is this a material you have used before? Do you know the source and whether it has been tested for which agents and to prove it is non-replicating What are the characteristics of the material upon receipt? What are the implications of the manipulations you are planning? Is this a material for which LAI have been reported or are materials of concern ( gov’t, society, etc)? SOURCE OF INFECTION • Microorganisms • Cells and tissues • Blood and body fluids • Any items contaminated with the above Laboratory Associated Infection SOURCE HOST SUSCEPTIBLE HOST • Immune system • Vaccination status • Age ROUTE ROUTE OF TRANSMISSION • Percutaneous inoculations • Inhalation of aerosols • Contact of mucous membranes • Ingestion Semen Vaginal Secretions Tissue Cultures Organ Cultures Infected Experimental Animals Other Bodily Fluids: Cerebrospinal, Amniotic, Synovial Pathogen involved Type of body fluid Route of exposure Duration of exposure Volume of blood involved in exposure Concentration of virus at time of exposure PPE worn ONLY IN CANADA Internationally Recognized Resource Designed, Research And Maintained By PHAC And CFIA PATHOGEN MATERIAL SAFETY DATA SHEETS http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/index-eng.php Personnel supervising & personnel using the material • your knowledge and experience • the level of mentorship available • New User Registration Form & Biosafety Health Assessment Forms • records your knowledge level • what you work with • health status Helps identify risk factors and potential for LAIs Criteria for consideration Routes of exposure that need to be blocked Degree of protection offered Ease of use Only effective if correctly selected, fitted, used and cared for the individual is well trained Ensure PPE is removed before leaving the lab Gloves - yes they are mandatory Double gloving a good practice Gloves should not be reused Herpes simplex virus (HSV) Gloves should be changed frequently Glove selection: latex, nitrile, rubber & vinyl Use the correct donning and doffing technique Lab Coats/Gowns Protect street clothing from spills Offer additional body protection Periodic cleaning required Echo virus type 9 Eyewear – need I say more ! NO CONTACTS ! Eye glasses, goggles, facemask Epstein-Barr Virus Infections Facemask – prevent inhalation How many agents do you know that have flu-like symptoms. Influenza Virus Footwear Closed toe and heel shoes only. No sandals! Streptococci bacteria Minimum standard of practice for preventing the transmission of BBP includes: Education Hand washing Use safe work practice Wearing appropriate protective equipment If samples cannot be guaranteed non-infective …… treat as infectious! Environment: laboratory, facility, community Regulatory RequirementS Lab Environ PHAC, CFIA, EC, Fed/Prov/Munipcial) Lab Design (conception, construction, renovations, maintenance) Contain your biohazard (Primary and secondary containment) uO Dept Control Access Fac (Physical controls: lab and inventory) • Experimental Protocols & Lab Practices Equipment Experimental Protocols • have to be researched thoroughly • designed with safety in mind as well as research • engage the supervisor • protocols on-line: http://www.protocol-online.org Remember once you start the protocol you are in research mode, so you better have thought of safety first! Lab Practices Good Lab Practices can save your life ! So adopt then from the start RG 1 or 2 or 3 The practices should change and the level of consciousness you exhibit should as well. PPE Set up Experimental Decontamination Waste Leaving the lab What material is presently being used and/or stored Location Expiry date Use log book MSDS’s Mandatory What samples are critical to save if storage fails, and have I identified them? FINALLY WE CAN START TALKING LAB SPECIFICS TRANSPORTATION OF DANGEROUS GOODS • Infectious substances •Diagnostic samples Yes there is more training you have to go to. IT’S THE LAW Transportation of Dangerous Goods Act: Class 6.2 (Infectious Substances) PHAC/CFIA restrictions Ensure: Proper classification Proper packaging Proper labeling Proper documentation Import/Export Permits Pre-approved Authorized Individuals Lead time (International Regulations….) Appropriate Scheduling (Holidays, Weekends) Transportation within the building Between lab to lab Colleague to Colleague Between Institutions Important Considerations: does material need to be transported at all packaging requirements means and route of transportation regulatory requirements Between lab transfers - 4 sided cart, sealed primary container, secondary container, low traffic route. Off Campus transfers – consult ORM At Shipping & Receiving Verify shipment is yours, and expected. Inspect the integrity of the outer container, to identify if possible damage may have been incurred. If no damage suspected, transfer to lab using appropriate practices. Open outer packaging (note this may require the use of a biological safety cabinet if the risk group requires it.) Package appears damaged thank goodness for tdg my life just got a hole lot easier ! If damage and breakage possible, get your spill kit for your biological sample ( Isn’t it handy that you did a risk assessment!) transfer the package into a secondary container lined with absorbent paper (absorbent side up), close lid of container Transfer to a cart with 4 sides for transfer to lab. •Open in an appropriate fashion; inspecting for leakage, breaks etc •Decontaminate all the areas potentially contaminated. •Dispose of sample in the appropriate manner •Package must be sterilized, defaced prior to disposal. REPORTING: If sample breach containment, inform your supervisor, ORM (x. 3153), and PS Before starting any manipulations Before leaving the lab Whenever the integrity of your gloves is questioned or your hands are obviously soiled Before and after completing any task in a BSC Every time gloves are removed Before contact with one’s face or mouth At the end of the day FREQUENTLY – ABC Aseptic technique is a set of specific practices and procedures performed under carefully controlled conditions with the goal of minimizing contamination by pathogens. S Space and work flow? C Clean, aseptic, or sterile technique? R I Routine, aseptic or surgical hand hygiene? Instruments and supplies? Personal protective equipment? P Trash: sharps, infectious waste, radioactive T waste, pathology or routine waste? a·sep·sis /āsepsis/ · : The absence of bacteria, viruses, and other microorganisms. · The exclusion of bacteria and other microorganisms, typically during surgery, http://www.youtube.com/watch?v=4mKhULnxqcw Avoid use whenever possible Use a BSC for all operations with infectious material Fill syringes carefully Shield needles when withdrawing from stoppers Do not bend, shear or recap needles. Dispose of all used needles/syringes in yellow SHARPS containersharps containers Mouth pipetting is prohibited. Never force fluids out. To avoid splashes, discharge the liquid down the receiving container wall. Never mix material by suction and expulsion. Reusable pipettes should be placed horizontally in a disinfectant-filled pan. Sterilization in an open flame may create aerosols which may contain viable microorganisms. Shorter handles minimize vibrations Disposable plastic loops are good alternatives Flaming produces aerosols so why do it? • Equipment Use it & maintain it properly, your life depends on it ! Before use Check centrifuge rotors & tubes for cracks Avoid Overfilling Place caps or stoppers properly Balance loads Use sealed buckets (safety cups) or sealed rotors Before leaving: ensure centrifuge achieves run conditions After run Centrifuge has to be completely stopped before opening the lid Check for spills or leaks before removing samples. Clean spills Allow aerosols to settle (30 min) or open in a BSC Operate in a BSC whenever possible. Allow aerosols to settle for 5 minutes before opening. Decontaminate after use Blender Do not use glass blender jars Use safety blenders which can be autoclaved Lyophilizers (used for dehydration process) Use glassware designed for vacuum work, ensure there is no damage before using Use vapour traps whenever possible Cryostats, Nitrogen Storage Vessels, - 80 °C Freezers Cryostats: Wear gloves during preparation of frozen sections and heavy gloves when accessing the cryostat. Decontaminate frequently. contain HEPA filters which remove particles (min 0.3 microns) from supply and exhaust air with 99.97% efficiency . Vertical or horizontal laminar flow HEPA filtered supply air only Provide product protection only HEPA filtered supply and exhaust air Personnel and environment Biological Safety Cabinet protection 3 Class II + III http://www.youtube.com/watch?v=Wg61LdngWlQ Before using the cabinet: Ensure BSC is certified Disinfect work surfaces with appropriate disinfectant Turn off UV lamp; turn on fluorescent lamp Place essential items inside cabinet be prepared to work from Clean to Dirty Allow the blower to run for 5-10 min before work Hand movements when entering, within and exiting BSC must be slow and deliberate to prevent disturbing air flow Ensure: material and equipment is placed near the back of the hood, especially aerosol-generating equipment. Do not block any vents Use techniques that reduce splatter and aerosols. After using the cabinet: Leave blower on at least 5 minutes to purge cabinet Remove and decontaminate equipment and materials Disinfect cabinet surfaces Turn off blower and fluorescent lamp, turn on UV lamp Maintenance: Before and after each use - Wipe down work surfaces Weekly - Clean UV lamp Monthly - Wipe down all vertical surfaces Annually – Verify UV lamp intensity - Decontamination with formaldehyde gas (managed by ORM x 3153) Certification – is required if the cabinet was moved that as filter seal could have been breached (contact ORM x 3153) DECONTAMINATION ? DISINFECTION ? STERILIZATION ? Decontamination: The destruction of microorganisms to a lower level such that it removes danger of infection to individuals. Sterilization: The complete destruction of all viable microorganisms. Disinfection: Use of agents (physical or chemical) to destroy harmful organisms on inanimate objects Heat: Autoclaving (most practical and recommended) Incineration (for disposal of sharps and tissues) Irradiation: UV light (wavelength of 253 nm is germicidal) Gamma (disrupts DNA and RNA) Filtration HEPA (biological safety cabinets, ventilation) Items that CAN be autoclaved: Culture dishes and related devices Cultures and stocks of infectious material Discarded live and attenuated vaccines Contaminated solid items (petri dishes, eppendorf tips, pipettes, gloves, paper towels) Items that CANNOT be autoclaved: chemicals (flammables, oxidizers, phenols, acids, alkalides) chemotherapeutic or radioactive waste bleach (or other chlorinated products) certain kinds of plastics Sharps (not at the University of Ottawa) Many autoclaves are now run by dedicated staff, however, if you are operating an autoclave: Learn how to use it! Ensure PPE is worn Recognize acceptable material and packaging Proper loading and unloading All users/operators must take autoclave training http://www.benchfly.com/video/139/using-an-autoclave/ Preparation of waste: Use only approved autoclave bags Do not overfill autoclave bags Separate material for re-use from that which will be disposed, and dry from liquid material If outside of bag is contaminated, double bag All flasks containing biological material should be capped with aluminum foil Ensure items are labeled with contact information Generally for disinfection rather than sterilization Choice depends on: Type of material to be disinfected Organic load Chemical characteristics Most common are chlorine compounds and alcohols (broad range) Vegetative bacteria (E.coli, Staph) 2% domestic bleach 75% Ethanol Quaternary ammonia 6% formulated Hydrogen peroxide Mycobacteria and fungi 10% domestic bleach 75% Ethanol Phenolic compounds Spore forming bacteria (Bacillus) 10% domestic bleach Glutaraldehyde Formaldehyde 6% formulated Hydrogen peroxide Viruses Enveloped (HIV, Herpes) 2% domestic bleach 75% Ethanol Quaternary ammonia 6% formulated Hydrogen peroxide* Non enveloped (Hepatitis, Adenovirus) 10% domestic bleach 6% formulated Hydrogen peroxide* Glutaraldehyde Formaldehyde Discarded biological material from teaching, clinical and research laboratories and operations is biomedical waste. Includes but is not limited to: Animal waste Biological laboratory waste Human anatomical waste Human blood and body fluid waste Sharps All biological waste should be decontaminated prior to disposal (including level 1 agents). Treated waste is no longer considered ‘biomedical’ (i.e. microbiological waste, blood and bodily fluid waste) and can be disposed of in the regular waste stream. Any waste that cannot be treated (i.e. sharps, carcasses, tissues and body parts) remains biomedical waste and must be incinerated off site. Biomedical Waste (treated) *in compliance with sewer use by-laws with H2O (1:10) Biomedical Waste (untreated) YOU TELL ME ..... Mitigates the risk of: 1. Personnel exposure 2. Contamination a) sample b) environment It’s you or them, make your decision! It’s you or it’s them, make a choice! What are we talking about ? Are you prepared? Did you anticipate this? I told you that risk assessment would come in handy! ◦ What is the risk? ◦ What is the route of exposure? ◦ Are aerosols still suspended? ◦ Is the risk contained? REMEMBER – if the risk was inhalation, there may not be any evidence of an exposure having occurred. Inform all those in the vicinity. Restrict access and resuspending or relocation of particles. Vacate area for 30 minutes before re-entering. Report, sign area, seek medical assistance. Spill response will vary depending on: what, where, how much, when, who Cover spill area with absorbent material Soak the spill area with an appropriate disinfectant (i.e. 10% bleach, Virox) Pour disinfectant from the outside of the absorbent material towards the inside Leave on for 20 to 30 minutes Pick up any broken glass (with forceps!) and place in a SHARPS container Wipe up with absorbent material Waste should be disposed in appropriate biohazardous waste container UO template is available: (http://www.uottawa.ca/services/ehss/docs/SPILL RESPONSEPLAN.pdf) Don’t forget it must be tailored to be lab specific. All potential exposures immediately to: Your supervisor /PI ORM x 5892 5411 (through Protection Services) No Excuses! Occupational Health, Disability and Leave Form On-line https://web30.uottawa.ca/v3/riskmgmtfrm/aioreport.aspx?lang=en YOU WANT FUNDING FAST – HERE ARE SOME TRICKS Purchasing & Receiving of Biological Agents PHAC, CFIA, Environment Canada Inventory Records Transportation/Transfer Transport Canada- TDG Tricouncil, Funding Agencies , Contracts (MTA) Require compliance to the established biosafety program (based on federal, provincial, municipal and international requirements. Project Spec Form ( Project Review) New User Registration Form Training Streamlining them, On-line migration But they must be complete in that they must be detailed EFFORT = RESULTS Delays are a result of incomplete submissions Project specific form (Tricouncil requires biosafety review) Describe what you are doing as it relates to your awarded grant What agents you will use ---- NO SHORT CUTS! It has to be what is described in your grant proposal or MTA ASK YOURSELF Would my answers pass a Funding Agency AUDIT ? Biohazardous Material User Registration Form It incorporates: training, experience, proposed work details Biosafey Health Assessment Form ( it is for your own safety) “How soon do you need it?” “You want it when?” In order to facilitate a quick turnaround, provide: reference to which grant copies of MSDS’s reference documents REMEMBER: Suppliers may need PHAC / CFIA Importation permits or letters of compliance. *Restrictions may exist Material Transfer Agreement conditions Existing Import Permit conditions *Permits required (PHAC, CFIA (animal, plant, aquatic), DFAIT) *Facility certification *Transportation of Dangerous Goods *International Holidays Time factors: complete submission gov’t turn around (2-4 wk) Lead time Grant cycle http://www.uottawa.ca/services/ehss.biosafety.htm Biohazardous Materials User Registration Biosafety Health Assessment Survey UOttawa webpage Services ORM Programs (left column) Biosafety You haven’t finished training until you take the training comprehension test. Access to test on Virtual Campus is granted by Biosafety Compliance Specialist, requires providing: Name, email, employee/student # It’s for your own safety! CONFUSED ? OVERWHELMED ? QUESTIONS ? Lois Sowden-Plunkett lsowden@uottawa.ca Ext. 3058 Pierre Laflamme plaflam2@uottawa.ca Ext. 3153