Acute respiratory distress syndrome
advertisement

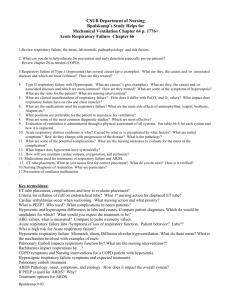
Critical Care Nursing Theory ARDS Acute Respiratory Distress Syndrome (ARDS) Acute respiratory distress syndrome (ARDS) represents a complex clinical syndrome (rather than a single disease process) and carries a high risk of mortality. ARDS was first described in 1967 and was termed adult (rather than acute) respiratory distress syndrome because of a misconception that the syndrome occurred only in adults Diagnostic criteria for ARDS have been hard to define because ARDS is at the extreme end of a continuum of acute, hypoxic lung injury resulting in acute respiratory failure. Acute respiratory distress syndrome (ARDS) Definition: Is a sudden and progressive form of acute respiratory failure in which the alveolar capillary membrane becomes damaged and more permeable to intravascular fluid. The Alveoli fill with fluid, resulting in severe dyspnea, hypoxemia refractory to supplemental O2, reduced lung compliance, and diffuse pulmonary infiltrates. ARDS is a serious reaction to various forms of injuries to the lung. It is characterized by inflammation of the lung parenchyma leading to impaired gas exchange with concomitant systemic release of inflammatory mediators causing inflammation, hypoxemia and frequently resulting in multiple organ failure. This condition is often fatal, usually requiring mechanical ventilation and admission to an intensive care unit. A less severe form is called acute lung injury (ALI). Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 1 Critical Care Nursing Theory ARDS Risk Factors for (ARDS) PATHOPHYSIOLOGY The pathological pulmonary alterations of ARDS are directly related to a cascade of events resulting from release of cellular and biochemical mediators. The activation, interactions, and multisystem actions of biological mediators are extremely complex. Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 2 Critical Care Nursing Theory Dr. Abdul-Monim Batiha ARDS Assistant Professor Of Critical Care 3 Critical Care Nursing Theory ARDS Stages of Acute Respiratory Distress Syndrome Stage 1 (first 12 hr): Normal chest x-ray, Dyspnea, tachypnea, Pathological Change: Neutrophil sequestration, no evidence of cellular damage. Stage 2 (24 hr): Patchy alveolar infiltrate, primarily in dependent lung areas; normal heart size, Dyspnea, tachypnea, cyanosis, tachycardia, coarse crackles, Pathological Change: Neutrophil infiltration, vascular congestion, fibrin strands, increased interstitial and alveolar edema Stage 3 (2–10 days): Diffuse alveolar infiltrates, possibly air bronchograms, decreased lung volume, normal heart size Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 4 Critical Care Nursing Theory ARDS Systemic inflammatory response syndrome (SIRS) presentation Stage 4 (>10 days): Persistent infiltrates, new pneumonic infiltrates, recurrent pneumothorax Multiple organ involvement, difficulty maintaining adequate oxygenation, sepsis, pneumonia Systemic Inflammatory Response Syndrome: Systemic inflammatory response syndrome (SIRS) describes the inflammatory response occurring throughout the body as a result of some systemic insult. Most patients with ARDS manifest the symptoms that define SIRS. Systemic Inflammatory Response Syndrome (SIRS) Criteria SIRS is manifested by two or more of the following: ■ Temperature greater than (38°C) or less than (36°C) ■ Heart rate greater than 90 beats/minute ■ Respiratory rate greater than 20 breaths/minute or an arterial carbon dioxide tension (PaCO2) less than 32 mm Hg ■ White blood cell count greater than 12,000 cells/mm3 or less than 4,000 cells/mm3 OR more than 10% immature (band) forms Integrated Assessment of the Patient with (ARDS) Stage 1 (first 12 hr) Physical Examination • Restlessness, dyspnea, tachypnea, Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 5 Critical Care Nursing Theory ARDS • Moderate to extensive use of accessory respiratory muscles Diagnostic Test Results • ABG: Respiratory alkalosis • CXR: No radiographic changes • Chemistry: Blood results may vary depending on precipitating cause (e.g., elevated white blood cell count, changes in hemoglobin) • Hemodynamics: Elevated PAP, normal or low PAWP Stage 3 (2–10 days) Physical Examination • Decreased air entry bilaterally • Impaired responsiveness (may be related to sedation necessary to maintain mechanical ventilation) • Decreased gut motility • Generalized edema • Poor skin integrity and breakdown Diagnostic Test Results: • ABG: Worsening hypoxemia • CXR: Air bronchograms, decreased lung volumes • Chemistry: Signs of other organ involvement: decreased platelets and hemoglobin, increased white blood cell count, abnormal clotting factors • Hemodynamics: Unchanged or becoming increasingly worse Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 6 Critical Care Nursing Theory ARDS Stage 4 (>10 days) Physical Examination: • Symptoms of MODS, including decreased urine output, poor gastric motility, symptoms of impaired coagulation OR • Single-system involvement of the respiratory system with gradual improvement over time Diagnostic Test Results: • ABG: Worsening hypoxemia and hypercapnia • CXR: Air bronchograms, pneumonthoraces • Chemistry: Persistent signs of other organ involvement: decreased platelets and hemoglobin, increased white blood cell count, abnormal clotting factors • Hemodynamics: Unchanged or becoming increasingly worse Comparison of Acute Lung Injury (ALI) and Acute Respiratory Distress Syndrome (ARDS) Criterion PaO2:FIO2 regardless of level ALI ratio, Less than 300 PEEP Chest x-ray Pulmonary wedge pressure Bilateral infiltrates ARDS Less than 200 Bilateral infiltrates artery Less than 18 mm Hg or Less than 18 mm Hg or no indication no indication indication of left atrial hypertension Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 7 Critical Care Nursing Theory ARDS Hyopxemia and PaO2/FiO2 ratio below 200 (e.g., 80/0.8=100) despite increased FiO2 by mask, cannula, or endotracheal tube are the hall marks of ARDS. NURSING ALERT The treatment for ARDS is aimed at symptom management, but the underlying cause must be treated or the ARDS will not resolve. Supportive measures will assist the patient while the underlying cause is being treated. MANAGEMENT 1. OXYGEN DELIVERY Oxygen delivery is determined by hemoglobin, Recent studies on transfusion requirements indicate that values of approximately 8.0 g/dL are sufficient for critically ill patients, except for those with cardiac disease. Therefore, transfusion to maintain normal hemoglobin is no longer accepted therapy and should be discouraged Therapies to optimize cardiac output are directed toward enhancing preload and contractility and normalizing afterload. Fluid administration to ensure adequate intravascular volume and optimize preload is important before other interventions are initiated. (PAWP) should be maintained at greater than 12 mm Hg and breath sounds and ABGs closely monitored during fluid administration. Positive inotropic agents, such as dopamine or dobutamine, are used to enhance contractility and increase cardiac output. Vasoconstrictors, such as norepinephrine, may be added to the therapies to counteract the SIRS induced vasodilation 2. MECHANICAL VENTILATION Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 8 Critical Care Nursing Theory ARDS use of the lowest fraction of inspired oxygen (FIO2) to achieve adequate oxygenation and use of small tidal volumes (<6 mL/kg) to minimize airway pressures, thus preventing or reducing lung damage (barotrauma and volutrauma) while maintaining the PaCO2 within a relatively normal range PEEP prevents collapse and opens alveolar sacs, allowing diffusion of gases across the alveolar–capillary membrane. Recommended values for PEEP are 10 to 15 cm H2O, Inverse ratio ventilation is another strategy thought to improve alveolar recruitment Reversal of the normal inspiratory:expiratory ratio (I:E ratio) to 2:1 or 3:1 prolongs inspiration time, preventing complete exhalation. This increased end-expiratory volume creates auto-PEEP (intrinsic PEEP) that is added to the applied extrinsic PEEP 3. EXTRACORPOREAL LUNG-ASSIST TECHNOLOGY Extracorporeal lung-assist technology involves the use of large vascular cannulas to remove blood from the patient. A pumping device and circuit circulate the blood, and one or two “artificial lungs” remove carbon dioxide and oxygenate the blood. 4. POSITIONING Frequent position change is well established as a means to prevent and reverse atelectasis and facilitate removal of secretions from the airways. Although not a treatment for ARDS, turning a patient side to side, having the patient sit upright, and using the Trendelenburg position for postural drainage are necessary interventions to prevent worsening of respiratory failure due to atelectasis and pneumonia. Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 9 Critical Care Nursing Theory ARDS Continuous lateral rotation using a kinetic therapy bed turns patients slowly 60 degrees to each side over 11 minutes and is useful to enhance secretion removal Prone positioning, in the patient’s bed improves pulmonary gas exchange, facilitates pulmonary drainage in the dorsal lung regions, and aids resolution of consolidated dependent alveoli (in the supine position), particularly in the dorsal lung regions. Pharmacological Therapy Most of the pharmacological agents used in the ARDS population are supportive. Antibiotic therapy is appropriate in the presence of a known microorganism but should not be used prophylactically. Bronchodilators and mucolytics are useful in ARDS to assist in maintaining airway patency and reducing the inflammatory reaction and accumulation of secretions in the airways. Exogenous surfactant replacement therapy has been used for several years in neonates with hyaline membrane disease to decrease alveolar surface tension and facilitate the maintenance of open alveoli. Pharmacological Therapy The use of corticosteroids to decrease the inflammatory response in late stages of ARDS is regaining popularity with recent case studies and one randomized, controlled trial supporting low doses in the 7- to 10-day range of ARDS Effective use of sedation to promote comfort and reduce respiratory effort, thus decreasing oxygen demand, is an important consideration for nurses dealing with patients with ARDS Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 10 Critical Care Nursing Theory ARDS Nutritional Support Adequate nutrition should be initiated early and maintained, because nutrition plays an active therapeutic role in recovery from critical illness. Nursing Interventions Care is similar to patient with respiratory failure Dr. Abdul-Monim Batiha Assistant Professor Of Critical Care 11