What is CA-MRSA - McMaster University
advertisement
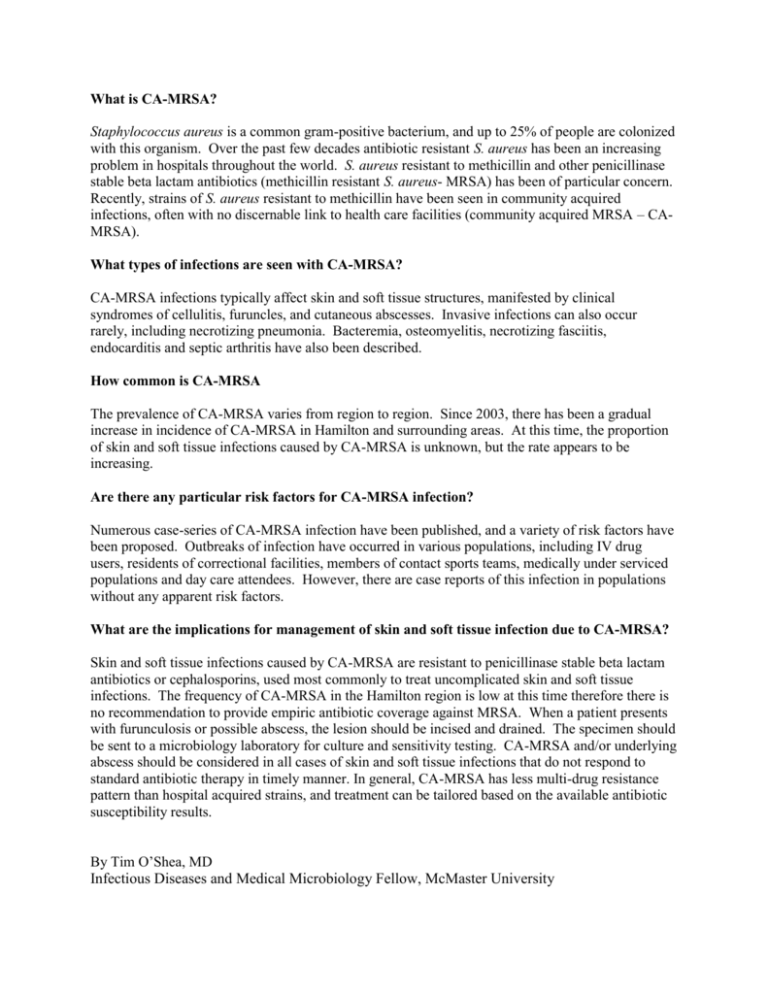
What is CA-MRSA? Staphylococcus aureus is a common gram-positive bacterium, and up to 25% of people are colonized with this organism. Over the past few decades antibiotic resistant S. aureus has been an increasing problem in hospitals throughout the world. S. aureus resistant to methicillin and other penicillinase stable beta lactam antibiotics (methicillin resistant S. aureus- MRSA) has been of particular concern. Recently, strains of S. aureus resistant to methicillin have been seen in community acquired infections, often with no discernable link to health care facilities (community acquired MRSA – CAMRSA). What types of infections are seen with CA-MRSA? CA-MRSA infections typically affect skin and soft tissue structures, manifested by clinical syndromes of cellulitis, furuncles, and cutaneous abscesses. Invasive infections can also occur rarely, including necrotizing pneumonia. Bacteremia, osteomyelitis, necrotizing fasciitis, endocarditis and septic arthritis have also been described. How common is CA-MRSA The prevalence of CA-MRSA varies from region to region. Since 2003, there has been a gradual increase in incidence of CA-MRSA in Hamilton and surrounding areas. At this time, the proportion of skin and soft tissue infections caused by CA-MRSA is unknown, but the rate appears to be increasing. Are there any particular risk factors for CA-MRSA infection? Numerous case-series of CA-MRSA infection have been published, and a variety of risk factors have been proposed. Outbreaks of infection have occurred in various populations, including IV drug users, residents of correctional facilities, members of contact sports teams, medically under serviced populations and day care attendees. However, there are case reports of this infection in populations without any apparent risk factors. What are the implications for management of skin and soft tissue infection due to CA-MRSA? Skin and soft tissue infections caused by CA-MRSA are resistant to penicillinase stable beta lactam antibiotics or cephalosporins, used most commonly to treat uncomplicated skin and soft tissue infections. The frequency of CA-MRSA in the Hamilton region is low at this time therefore there is no recommendation to provide empiric antibiotic coverage against MRSA. When a patient presents with furunculosis or possible abscess, the lesion should be incised and drained. The specimen should be sent to a microbiology laboratory for culture and sensitivity testing. CA-MRSA and/or underlying abscess should be considered in all cases of skin and soft tissue infections that do not respond to standard antibiotic therapy in timely manner. In general, CA-MRSA has less multi-drug resistance pattern than hospital acquired strains, and treatment can be tailored based on the available antibiotic susceptibility results. By Tim O’Shea, MD Infectious Diseases and Medical Microbiology Fellow, McMaster University