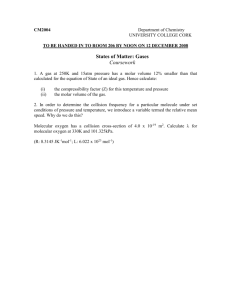
Local anaesthesia
advertisement

Principles of management of impacted teeth An unerupted tooth: is a tooth that is in the process of eruption and is likely to erupt based on clinical and radiographic findings. Malposed tooth: A tooth unerupted or erupted which is in an abnormal position in the maxilla or in the mandible An embedded or impacted tooths: is the tooth that has failed to erupt completely or partially to its correct position in the dental arch and its eruption potential has been lost. The word impaction is from Latin origin| (impactus). Impaction is cessation of eruption of a tooth caused by a physical barrier or ectopic positioning of a tooth. An impacted tooth is one that is erupted, partially erupted or unerupted and will not eventually assume a normal arch relationship with the other teeth and tissues. Impacted Teeth Impacted teeth seen in the following order of frequency: 1. Mandibular third molars 2. Maxillary third molars 3. Maxillary canine 4. Mandibular premolar 5. Maxillary premolar 6. Mandibular canine 7. Maxillary central incisors 8. Maxillary lateral incisors. Causes of Impaction of Teeth Inadequate Space in the Dental Arch for Eruption The phylogcnic theory: Due to evolution, the human jaw size is becoming smaller and since the third molar tooth is last to erupt, there may not be room for it to emerge in the oral cavity. Mendelian theory: Here genetic variations play a major role. If the individual genetically receives a small jaw from one of the parents and/or large teeth from the other parent, then impacted teeth can be seen, because of lack of space. Causes of impaction of a tooth can be divided into local and systemic causes. 1 Indications for Removal of Impacted Teeth 1. Recurrent pericoronitis, pain, infection, caries. pericoronitis is the inflammation of the gingiva surrounding a crown of a partially erupted tooth. 2. Deep periodontal pocket associated with partially erupted tooth. 3. Prior to orthodontic treatment, to control the tooth crowding in the mandible. 4. Prevention of caries: caries of the impacted tooth crown and the adjacent tooth can be seen due to an inability to access and clean the area. 5. Prevention of root resorption: Root resorption of the distal root of the adjacent second molar is seen in the 21 to 30 years of age group. Root resorption of lateral incisor may be seen associated with an impacted maxillary or mandibular canine. 6. Management of cysts and tumours, abscess of odontogenic origin (Associated lesions). 7. Prevention of pathological fractures. 8. Preparation of orthognathic surgery: prior to sagittal split osteotomy of ramus in order to avoid bad split, inadvertent fracture of the mandible, lower third molars are extracted. Maxillary third molars are removed during Le Fort I osteotomy procedure. 9. Management of preprosthetic concerns, before the fabrication of the prosthesis, impacted teeth should be removed. 10.Impacted teeth in the line of fracture. 11.Prophylactic removal. Classification of Impacted Teeth Maxillary and mandibular third molars' are classified radiographically by angulation, depth and arch length or relationship to the anterior aspect of the ascending mandibular ramus. Classification is helpful for the following: • Describes the general position of the impacted third molar. • Aids in estimating the difficulty in removing the tooth. 2 Mandibular third molar classification Winter's Classification: Angulation According to the position of the impacted third molar to the long axis of the second molar. The Winter's classification is suggested: 1. Mesioangular 2. Horizontal (transverse) simultaneously in: i. buccal version ii. lingual version iii. Torsoversion 3. Vertical 4. Distoangular 5. Buccoangular 6. Linguoangular Mesioangular impaction is the most common finding. Forty-three per cent of mandibular impacted third molars are mesioangular. Sixty-three per cent of maxillary impacted third molars are mesioangular. Depth: As per the relationship to the occlusal surface of the adjoining second molar of the impacted maxillary or mandibular third molar, the depth can be judged. 1. Position A: The highest position of the tooth is on a level with or above the occlusal line. 2. Position B: Highest position is below the occlusal plane, but above the cervical level of the second molar. 3. Position C: Highest position of the tooth is below the cervical level of the second molar. The deeper the impacted tooth, the more overlying bone is present and the more the angulation of impaction deviates from parallel to the long axis of the adjacent tooth, the more difficult it is to remove the impacted tooth. 3 Pell and Gregory classification Relationship of the impacted lower third molar to the ramus of the mandible and the 2 nd molar based on the space available distal to the 2nd molar: Class I: Sufficient space available for the eruption of the 3rd molar. Class II: the space available is less than the mesiodistal width of the crown of the 3 rd molar. It denoted that the distal portion of the third molar crown is covered by the bone of the ramus. Class III: The 3rd molar is totally embedded in the bone from the ascending ramus because of absolute lack of space. Maxillary third molar classification Angulation and depth classification is same as mandibular 3 rd molar. Classification in relation to the floor of the maxillary sinus: 1. Sinus approximation (SA): No or athiny bony partition present between impacted maxillary 3rd molar and the floor of maxillary sinus. 2. No sinus approximation (NSA): 2mm or more bone is present. • 4 Maxillary canin classification Labial or palatal placement of impacted maxillary canine. Intermediate position: a. Crown between the lateral incisors and premolar. b. Crown above the root tip with labial, palatal orientation of the lateral incisors or premolar. Aberrant position Impacted maxillary canines lie in the maxillary sinus or nasal cavity. • Class I: Palatally placed maxillary canine a. Horizontal b. Vertical c. oblique • Class II: Labially or buccally placed maxillary canine a. Horizontal b. Vertical c. oblique • Class III: Involving both buccal and palatal bone, e.g. crown is placed on the palatal aspect and the root is toward the buccal alveolar process • Class IV: Impacted in the alveolar process between the incisors and first premolar. • Class V: Impacted in the edentulous maxilla. Classification for Impacted Mandibular Canine 1. Labial a. Vertical b. Oblique c. Horizontal 5 2. Aberrant a. At inferior border b. On the opposite side Factors Responsible for Increasing the Difficulty Score for Removal of Impacted Teeth • As per the angulation • As per the depth • As per the space available for the eruption • Crown size: large bulbous crown increases the difficulty • Configuration of the roots of the impacted tooth: the point of application of the elevator and the path of delivery of the impacted tooth depends mainly on the configuration of the roots: a. Lengtn of the roots: longer the roots more difficult the extraction. b. Root development: if the root development is (less than one-third) insufficient, then the tooth is more difficult to remove. It moves like a ball in the socket and difficult to elevate. c. Curvature of the roots: dilacerated, curved, divergent roots are difficult to remove. Fused conical roots are easy. d. Root size: thin, slender roots are difficult to remove. Stout, bulbous, hypercementosed roots also increase the difficulty. • Bone texture and density: depends on the age, sex and systemic problems. Younger patients have spongy, elastic pliable bone, while older group of patients may exhibit sclerosed bone. • Size of the follicular sac: presence of large follicular sac makes the extraction easier, as the amount of bone removal is less. Nonexistent or narrow follicular sac around the crown will require bone cutting around the crown difficult extraction. • Space or contact in relation to mandibular second molar: If the impacted tooth is locked against the crown of the second molar and there is no space for elevation, then sectioning of the tooth should be planned. • Relationship to the inferior alveolar neurovascular bundle: proximity of the roots to the neurovascular bundle increases the possibility of the damage, injury to the nerve during extraction. Temporary altered sensation of the lower lip can be experienced by the patient (paraesthesia, anaesthesia) which can last for few days or months. Radiological assessment is important. Dentascan can show exact location of the nerve. • Nature of covering tissue: a. Soft tissue impaction. b. Partial bony impaction, covered by soft tissue, as well as partially by the bone. c. Fully bony impaction. • Access to the operative field, inability to open the mouth wide, a large uncontrollable tongue, small orbicularis oris muscle (oral sphincter). Radiological Examination Intraoral X-ray • Intraoral X-rays are possible, if tooth is in the alveolus and not in the ramus • Possible if oral opening is adequate • If there is no gagging • Useful to study the relation with adjoining tooth • Useful to study the configuration of the roots and status of the crown (caries, size, etc.) 6 • Useful to record the relationship with inferior alveolar canal • For parallex technique 'tube shift' method should be used or occlusal film is taken. The position and depth of the tooth can be assessed by taking intraoral X-ray or even lateral extraoral X-ray and tracing can be done, which was originally advocated by George Winter. Three imaginary lines are drawn which are known as Winter's lines: • White line: corresponds to the occlusal plane. The line is drawn touching the occlusal surfaces of first and second molar and is extended posteriorly over the third molar region. It indicates the difference in occlusal level of second and third molars. • Amber line: represents the bone level. The line is drawn from the crest of the interdental septum between the molars and extended posteriorly distal to third molar or to the ascending ramus. This line denotes the alveolar bone covering the impacted tooth and the portion of tooth not covered by the bone. • Red line: is drawn perpendicular from the amber line to an imaginary point of application of the elevator. It indicates the amount of bone that will have to be removed before elevation, i.e. the depth of the tooth in bone and the difficulty encountered in removing the tooth. If the length of the red line is more than 5 mm then the extraction is difficult. Every additional mm renders the removal of the impacted tooth three times more difficult (more than 9 mm below the level of the apices of the second molar). 7 Extraoral X-rays For mandibular teeth • OPG • Lateral oblique view For maxillary teeth • OPG • PA view Water's position mandible Indicated in • Patients with restricted oral opening/trismus/ excessive gagging. • Impacted tooth in an aberrant position. • For ruling out associated pathology. • To study the relationship of the tooth to inferior alveolar nerve inferior border. For maxillary teeth relationship to the maxillary sinus. 8 Surgical Removal of Impacted Teeth 1. Asepsis and isolation 2. Local anaesthesia, with or without sedation, or general anaesthesia 3. Incision, flap design 4. Reflection of mucoperiosteal flap 5. Bone removal 6. Sectioning (division) of tooth 7. Elevation 8. Extraction 9. Debridement and smoothening of bone 10. Control of bleeding 11. Closure by suturing 12. Medications antibiotics, analgesics, etc. 13. Follow-up Isolation of Surgical Site • Scrubbing by painting of skin and oral mucosa. Scrubbing solutions used first on skin only: o Cetrimide, absolute alcohol or cetrimide, povidone, and iodine o Cetrimide, absolute alcohol, and chlorhexidine • Cleaning solutions: used on skin only to remove residual soap solution: — Normal saline — Alcohol • Painting solution: act topically to inhibit further growth of microbes: — Povidone-iodine 5 per cent for skin, 1 per cent, for oral mucosa. — Chlorhexidine gluconate 7.5 per cent for skin, 0.2 per cent for rinsing oral cavity Drape the patient with sterile drapes to cover upper part of the face to isolate the oral cavity. 9 Local Anaesthesia • For mandibular molars and canines pterygo mandibular nerve block. • For maxillary molars posterior superior alveolar nerve block and palatine nerve block or infiltration. • For maxillary canines infraorbital nerve block, palatal infiltration of incisive canal and bilateral palatine nerve blocks. Good infiltration is a must to provide haemostasis and to define the tissue planes Incision (Flap Design) The mucoperiosteal flap for removal of impacted tooth is required to be designed well for adequate access and for elimination of obstruction to the pathway of removal. The incision for this mucoperiosteal flap will have an anterior limb and a posterior limb connected with or without an intermediate limb. For Mandibular Molars Anterior releasing incision should begin from the vestibule upwards towards midway of the CEJ of second molar at an angle. If third molar is deep and surgery requires more removal of bone, this incision should be placed anterior to the second molar. The incision is then continued in the gingival sulcus (over the alveolar crest, if tooth is fully embedded) up to the distal aspect of third molar. Distal releasing incision is started from the distal most point of third molar across external oblique ridge into the buccal mucosa. This incision should not be taken on the lingual aspect of the ridge, as the lingual nerve can be found at or above the crest of the alveolar ridge, in approximately 17 per cent of the population. However, the normal position of the lingual nerve is 2 mm inferior to the crest and 0.5 mm lingual to the lingual cortex of the mandible in the third molar region. The length of this mucoperiosteal flap and the number of teeth included will be determined by the amount of exposure necessary to gain the visibility of the region and the experience of the clinician. The incision should not be extended too far upward distally to avoid: i. Intraoperative brisk bleeding from the buccal vessels and anastomosing branches from lingual and facial arteries. ii. Postoperative trismus due to cutting through the fibers of temporalis muscle. iii. Herniation of buccal pad of fat into the surgical field. The sharp point of periosteal elevator is used to carefully elevate a mucoperiosteal flap beginning at the point of the incision behind the second molar. The elevator is brought forward to elevate the periosteum around the second molar and down the releasing incision. The other flatter end of the periosteal elevator is then used to elevate the periosteum posteriorly to the ascending ramus of the mandible. 10 For Maxillary Molars The anterior releasing incision is started anterior to second molar from the vestibule and till the mesial interdental papilla of the second molar. The incision should follow the gingival sulcus of second molar and continue over the tuberosity area from the distal most point of second molar. For Maxillary Canines If the canine is buccally placed: • Flap with anterior releasing incision • Trapezoidal flap • Semilunar flap. If the canine is palatally placed—the incision is taken in the gingival sulcus on the palatal side from the mesial aspect of the first molar of the same side. Releasing incision is given obliquely across the palate and should be deflected away from the palatine foramen. If unilateral an incision is restricted to the canine region of the opposite side. If bilateral an incision is extended to the first molar of the opposite side. For Mandibular Canines If buccally placed then crevicular incision from the midline is taken up to first molar. Anterior releasing incision is given close to the midline. Care should be taken to protect the mental nerve. If the canine is placed on the lingual side, then lingual envelop flap is taken. Bone Removal Aim i. To expose the crown by removing the bone overlying it. ii. To remove the bone obstructing the pathway for removal of a tooth. 11 How much Bone is to be removed? Adequate amount of bone should be removed to enable for elevation. But the extensive bone removal can be minimized by sectioning the tooth. Two Ways of Bone Removal a. High speed, high torque handpiece and bur technique b. Chisel and mallet technique. Bur technique Either no. 7/8 round bur or a straight no. 703 fissure bur is used. Either of these burs can be used for bone removal or for sectioning of a tooth. Burs should be always used along with copious saline irrigation to avoid thermal trauma to the bone. First step: The bur is used in a sweeping motion around the occlusal, buccal and distal aspect of the mandibular third molar crown to expose it and to have its orientation. Second step: Once the crown has been located, the buccal surface of the tooth is exposed with the bur to the cervical level of the crown contour and a buccal trough Hjj or gutter is created. The buccal trough should be made in the cancellous bone. It is important that the adequate amount of trough is created to remove any bony obstruction for exposure and the delivery of the tooth, especially around the distal aspect of the crown. The distolingual portion of the tooth should be exposed without cutting through the lingual bony plate to prevent damage to the lingual nerve. For the canine removal, the gutter, trough is created around the surface of the crown free from the contact with the neighbouring, overlying teeth. The bone removal around the crown is done till CE junction and to expose the crown beyond the greatest width. Important precautions while drilling the bone: • Protect overlying soft tissues by retraction with either periosteal elevator or Langenbeck retractor • Continuous irrigation either with normal saline to reduce the thermal necrosis of bone. Chisel and mallet technique • Historical importance • Very rarely used • Less bone necrosis than bur technique • Can cause inadvertent fracture of the bone 12 • The jaw bone should be supported, while using this technique. First step: For mandibular, maxillary molars, the first step is the placement of vertical stop cut, which is made by placing a 3 mm or 5 mm chisel vertically at the distal aspect of the second molar with bevel facing posteriorly (5 to 6 mm height). The aim is to prevent the force transmission anterior to the direction of the bone removal. Second step: At the base of the vertical stop (limiting) cut, the chisel is placed at an angle of 45° with the bevel facing upwards or occlusally, and oblique cut is made till the distal most point of third molar. This will result in the removal of a triangular piece of buccal plate distal to second molar. Additional triangular piece of bone is removed at the junction of vertical and oblique bone cut to gain the entry of the elevator tip. Finally the distal bone must be removed, so that when the tooth is elevated, there should be no obstruction at the distobuccal aspect. In case of canine removal, bone is cut till the level of CEJ and to expose the entire crown. Lingual Split Bone Technique • Quick and clean technique • Creates a saucerization of the socket, thereby reduces the size of the residual blood clot • Used for mandibular third molar removal, especially those which are placed lingually • Support the mandible at the inferior border. Steps 1. Vertical stop cut is made by placing the chisel with the bevel facing posteriorly, distal to the second molar. 2. With the chisel bevel downward, a horizontal cut is made backward from the lower end of the vertical limiting stop cut. 3. The buccal bone plate is removed above the horizontal cut. 4. The distolingual bone is then fractured inward by placing the cutting edge of the chisel along the dotted line A. Bevel side of the chisel is facing upward and cutting edge is parallel to the external oblique ridge. The chisel is held at 45° to the bone surface. 5. Finally small wedge of bone, which then remaining distal to the tooth and between the buccal and lingual cut, is excised and removed. 6. A sharp straight elevator is then applied and minimum force is used to elevate the tooth. As the tooth moves upward and backward, the lingual plate gets fractured and facilitates the delivery of the tooth. 7. After the tooth is removed, the lingual plate is grasped with the haemostat and freed from the soft tissue and removed. 8. Smoothening of the edges is done with bone file. Wound irrigated and sutured. 13 Tooth Sectioning, Elevation and Extraction • Reduces the amount of bone removal (conserves the bone) required prior to elevation of the tooth • Reduces the risk of damage to the neighbouring teeth • Planned sectioning permits the parts of the tooth to be removed separately in an atraumatic manner by creating space into which it is displaced and the remaining crown or root segments removed. • The direction in which the impacted tooth should be sectioned is dependent on the angulation of the impacted tooth, based on the line of draw of the segments. • Can be performed either with a bur or chisel. Bur use is preferable. Mallet blows may give psychological discomfort to the patient. • The bur is used in a controlled fashion to avoid damage to the vital structures and surrounding teeth and soft tissues. • The tooth is usually sectioned one-half to three-fourths with the bur and then it is completely sectioned with the elevator. Horizontal Impaction Same as that for distobuccal impaction. Mesioangular Impaction Distal half of the crown is sectioned off from the buccal groove till the CEJ; from buccal to lingual and extended into the furcation. A straight elevator is placed in the cut and rotated to fracture the distal portion of the crown which is removed. Then a straight elevator is placed on the mesial aspect of the third molar below the cervical area. A purchase point can be prepared into the crown at the mesiobuccal line angle with a small round bur, if the access to the elevator is not possible. Then a crycr or crane pick elevator can be used to elevate the tooth, engaging the purchase point. Vertical Impaction Sectioning is similar to mesioangular disimpaction procedure. Distoangular Impaction 14 Most difficult to remove, because of its pathway of delivery into the ascending ramus. Large amount of distal bone removal is required. The crown is sectioned from the roots just above the cervical line after sufficient bone is removed from the occlusal and distobuccal aspect. The entire crown is removed to improve the visibility and access to the roots. If the roots are divergent, they are further sectioned into two pieces and delivered individually. If the roots are convergent the simple use of straight elevator is sufficient. Elevation a. Coupland elevator: placed at the base of the crown. b. Winter criers: may be used in wedging action, buccal elevation. Buccal elevation may be done in molar and canines by drilling a purchase point in the roots just below CE junction. • Wedging action is useful, when molar crown is split vertically down to bifurcation of roots. Important precautions Support the inferior border and lingual cortex of the bone in the mandibular impaction. Support to the palatal bone in the maxillary third molar or canine 15 impactions during elevation should be given. Support the neighbouring tooth to prevent luxation of the same. Debridement and Smoothening of Bone Margins • Irrigation of the socket • Curetting to remove any remaining dental follicle and epithelium • Look for pieces of coronal portion (especially in carious teeth or sectioned teeth), check for remnants of bone, granulation tissue, and bleeding points. • Check for caries (root/crown), erosion, and damage to the adjacent teeth. • Round off the margins of the socket with large vulcanite round bur or bone file. • Irrigate the socket again. • Control bleeding before suturing.. Closure 3-0 black silk is used. Interrupted sutures given and maintained for 7 days. Complete surgical procedure for the removal of lower impacted third molar. In case of molars, suture distal to second molar should be placed first and should be water tight to prevent pocket formation. In case of palatally impacted canines, incisive papilla should be sutured carefully to reduce postoperative bleeding. Complications Intraoperative Complications During Incision For molars, facial vessel or buccal vessel may be cut. For lower canines mental vessels and for upper canines incisive canal or greater palatine vessels may be damaged. During Bone Removal Damage to the second molar, damage to the roots of overlying teeth, slipping of the bur into the soft tissues, fracture of the mandible when using chisel and mallet. During Elevation • Luxation of neighbouring or overlying tooth • Fracture of the adjoining bone • Fracture of the tubcrosity • Slipping of the tooth Into pterygomandibular, temporal spaces, sublingual pouch and maxillary sinus. • Damage to nasal wall, overlying teeth, lingual, inferior alveolar or mental nerve. During Debridement Damage to inferior alveolar nerve or lingual nerve. Damage to maxillary sinus. Postoperative Complications Pain, swelling, trismus, hypoesthesia, sensitivity, loss of vitality of neighbouring teeth. Pocket formation. Sinus tract formation, oroantral fistula, oronasal fistula. 16